Selecting the right technique for lower limb soft tissue reconstruction is a therapeutic challenge. Despite having several reconstruction options, it's important to choose a technique that is effective and with the least possible donor site morbidity.
ObjectiveDemonstrate the therapeutic efficacy of the medial tab flap in soft tissue reconstruction on the leg, compared to conventional flaps.
Materials and methodsCohort study matched by age. 64 patients with soft tissue defects were selected and according to the intervention divided in: group (1) medial tab flap, and group (2) conventional flaps (sural, soleus, gastrocnemius) followed up to one year postoperatively. Outcome variables: surgical time in minutes, healing, healing time in days, complications.
ResultsThe patients who underwent surgery with medial tab flap and with conventional flaps healed completely. The healing time was 16.2±11.2 days in the tab flap and 16.1±11.2 days in conventional flaps, no statistically significant differences were found between the groups (p=.89).
The surgical time for tab flaps was 225.2±117.8min, and 191.3±117.2min for the comparison flaps (p=.65), there were no statistically significant differences. There were no complications in the medial tab flaps.
ConclusionThe findings suggest that the medial tab flap technique is as effective as the conventional flap technique, with complete flap survival and healing, and without any major complications in this studied group.
La selección adecuada para la reconstrucción de tejidos blandos en la pierna es un reto terapéutico. A pesar de disponer de varias opciones de reconstrucción, es importante elegir una técnica eficaz y con la menor morbilidad posible de la zona donante.
ObjetivoDemostrar la eficacia terapéutica del colgajo de lengüeta medial en la reconstrucción de tejidos blandos de la pierna, en comparación con los colgajos convencionales.
Materiales y métodosEstudio de cohorte emparejado por edad. Se seleccionaron 64 pacientes con defectos de tejidos blandos, divididos, de acuerdo a la intervención, en 1) colgajo de lengüeta medial, y 2) colgajos convencionales (sural, sóleo, gastrocnemio), y se les realizó seguimiento hasta el año postoperatorio. Variables de desenlace: tiempo quirúrgico en minutos, cicatrización, tiempo de cicatrización en días, complicaciones.
ResultadosLos pacientes que fueron sometidos a cirugía con colgajo de lengüeta medial y colgajos convencionales cicatrizaron completamente. El tiempo de cicatrización fue de 16,2±11,2 días en el colgajo de lengüeta y de 16,1±11,2 días en los convencionales, sin diferencias estadísticamente significativas entre los grupos (p=0,89).
El tiempo quirúrgico para los colgajos de lengüeta fue de 225,2±117,8 minutos, y de 191,3±117,2 minutos para los de comparación (p=0,65), sin diferencias estadísticamente significativas. No hubo complicaciones en los colgajos de lengüeta medial.
ConclusiónLos hallazgos sugieren que la técnica de colgajo de lengüeta medial es tan eficaz como la técnica de colgajo convencional, con preservación y cicatrización completa del colgajo y sin ninguna complicación mayor en este grupo estudiado.
Soft tissue defects in the lower extremity are frequently caused by high-energy trauma or chronic disease including peripheral vascular disease, diabetes,1,2 and osteomyelitis.3,4
The scarcity of soft tissue in the anterior aspect of the tibia makes it more susceptible to infection, necrosis, and soft tissue defects, generating a risk of amputation, and therefore the lower extremity must be protected through timely reconstruction to restore the patient's functionality and quality of life. Early soft tissue reconstruction is associated with a low complication rate; on average, only 18% of wounds closed in the first week have complications, compared to those closed after this time, which entail a 50% complication rate.2
The selection of an appropriate method that provides the desired coverage is based on careful assessment of the defect, assessment of associated risks, treatment morbidity, recovery time, ultimate limb function, and surgeon experience.5
Despite the widespread inclination to cover soft tissue defects in the leg with microsurgical free flaps, because of their sophisticated requirements in physical resources and human talent, this approach is not always available,6 especially in low-resource regions such as Latin America.7 Therefore fasciocutaneous flaps are presented as an effective therapeutic option, since the skin and fascia behave as a composite flap nourished by the perforators, that can cover the soft tissue defect satisfactorily. This is the case with muscle flaps, both free and local.5
In response to the need to reconstruct soft tissue defects of the leg in high-energy trauma, where conventional flaps are sometimes not an option because the injuries are trauma associated, a fasciocutaneous flap technique, called the medial flap, has been developed based on the posterior tibial artery perforators (PTAP), using less specialised techniques. The medial flap is similar to the peninsular flap, with the difference that it is based on the angiosome of the posterior tibial artery rather than the angiosome of the saphenous artery (an angiosome is a block of tissue consisting of skin, subcutaneous tissue, fascia, muscle, and bone that is supplied by a specific artery and vein).8
According to its vascularity, it can be classified as a regional pedicle flap with axial pattern, since it is based on subcutaneous arteries of the posterior tibial bundle, which correspond to the same angiosome, but also relies on true anastomoses of another angiosome, such as the medial genicular artery in its most proximal segment.
The aim of this study is to demonstrate the therapeutic efficacy of the medial tab flap in soft tissue reconstruction of the leg compared to other conventional flaps (sural, soleus, gastrocnemius).
Patients and methodsAnalytical study of a matched cohort of patients with soft tissue defects in the anterior aspect of the leg, who underwent reconstruction using flaps in a specialist trauma centre, with an average of 2000 trauma and orthopaedic emergencies per month (overall, with different locations and severity), in Barranquilla, Colombia, between 2019 and 2022.
A total of 216 patients with soft tissue defects on the anterior aspect of the leg underwent surgery during the study period; of these, 18 patients were treated with medial fasciocutaneous flaps and constituted the intervention group. The remaining 198 were treated with conventional flaps, of which 46 patients were randomly selected to form the control group by propensity score matching (PSM) and matched for age. In terms of types of flap, there were 15 cases with sural flap, 18 with soleus flap, and 13 with gastrocnemius flap.
Patients with tibial defects were specifically identified and those meeting the inclusion criteria for medial tab flaps were selected. These were subjects between 18 and 70 years of age with a diagnosis of soft tissue defects in the leg due to grade IIIB open fractures, or due to infection, and in whom conventional flaps were contraindicated due to soft tissue injury to the island flap area, injury to the flap vascular bed, or injury to the flap structure (fascia, skin, or muscle).
Patients with a history of free flaps and whose clinical follow-up could not be completed to assess outcomes, patients whose soft tissue damage was located in the anatomical area of the perforator peroneal artery, and those with non-traumatic injuries or who refused the proposed treatment were excluded.
The outcome variables were surgical time measured in minutes from surgical incision to closure (the entire surgical procedure, including bone reconstruction surgeries, removal of osteosynthesis material, etc.), healing (taking into account tissue integrity, vascularisation, flap colour, and vitality as assessed by the surgeon in charge),9 healing time measured in days from immediate postoperative period to wound epithelialisation, and complications (necrosis, suture dehiscence, fistula, foreign body granuloma, defect enlargement).
The independent variables considered were age, sex, comorbidities, diagnosis, laterality, and anatomical location of the soft tissue defect in the leg.
Ethical aspectsThe institutional ethics committee approved this research study according to the ethical standards recognised by the Declaration of Helsinki, classified as ‘no risk’ research as per Resolution 8430 of 1993 of the Colombian Ministry of Health. Informed consent was obtained from all patients who participated in the study. The information collected was handled solely for the purposes of this study, protecting the confidentiality of the identification data of the patients involved.
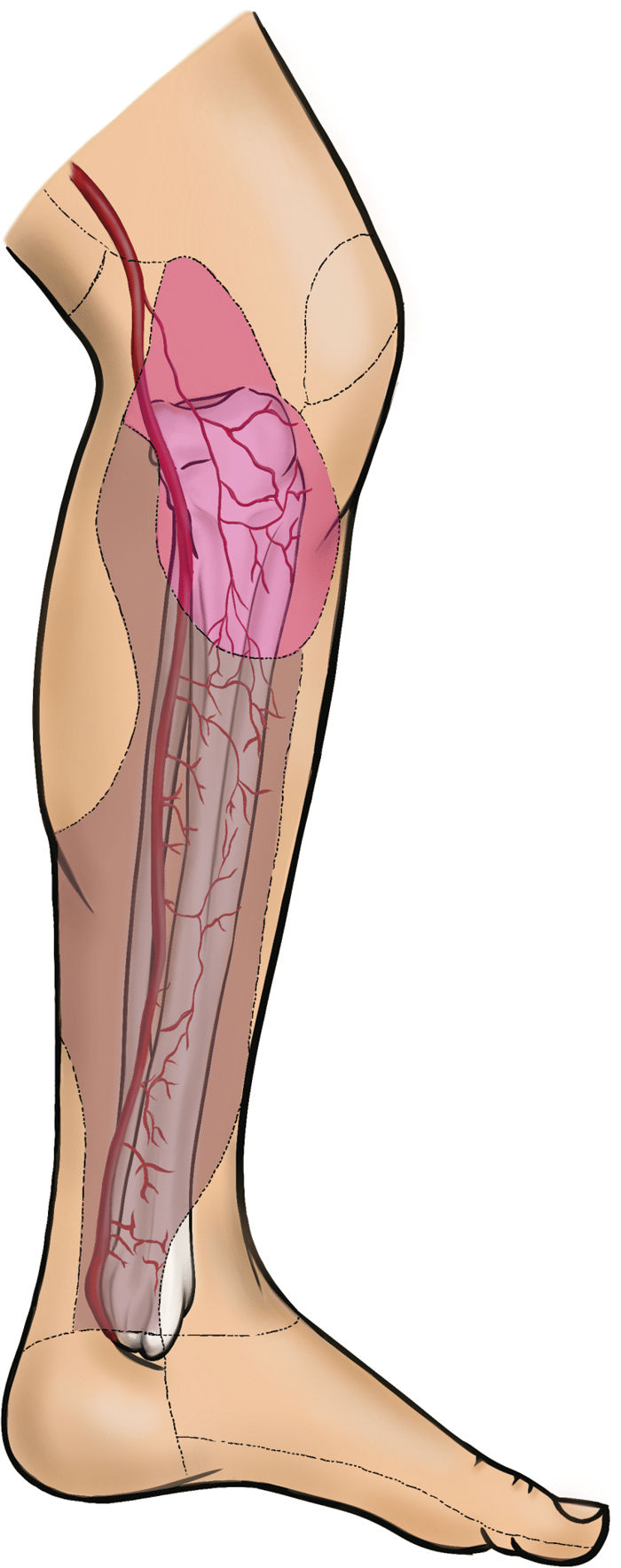
Anatomical bases of the flapThe medial tab flap is supplied by a source artery (posterior tibial), constant cutaneous perforators that are direct branches of the source artery and perforate the fascia (septocutaneous); in addition to the cutaneous perforating arteries (musculocutaneous) that come from the branches of the source artery, all based on the angiosome of the posterior tibial artery, it also receives shock anastomoses in its proximal part that come from the angiosome of the descending genicular artery (Fig. 1).
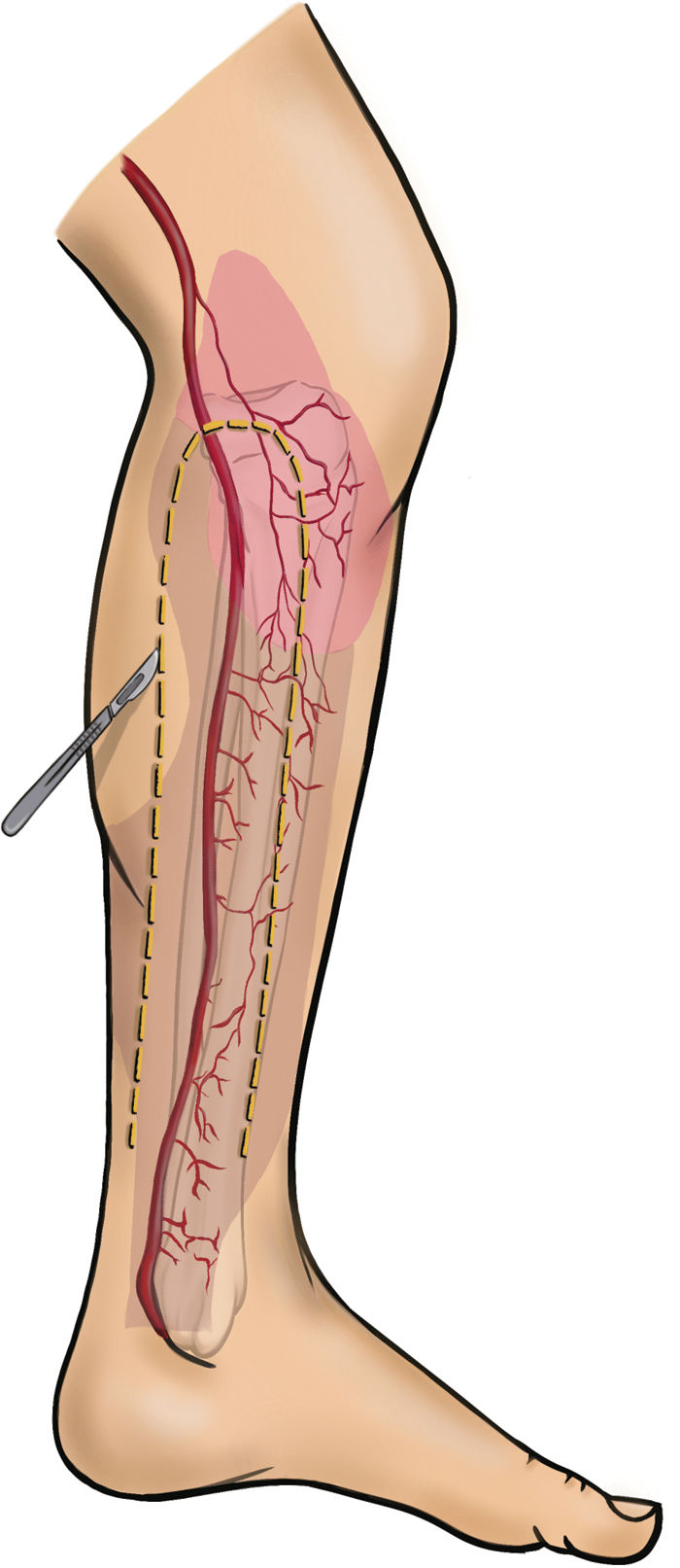
It is a subdermal flow based flap, and therefore care must always be taken to keep the fasciocutaneous plane intact; the size depends entirely on the angiosome described as posterior tibial and is useful for covering defects on the anterior aspect, which do not exceed the size of the angiosome, and is not useful for defects on the lateral or posterior aspect of the leg. As with all flaps, markings and measurements should be made prior to incision to plan for complete coverage of the defect. If the defect is located in the medial or proximal third, the flap should be distally based, without going beyond the junction of the medial and distal third to avoid injury to the vessels; if the defect is distal, the flap should be proximally based, without going beyond the junction with the medial or proximal third.
Surgeon's detailThis surgical technique was performed by a specialist in orthopaedics and traumatology, familiar with the basic principles of flaps and angiosomes and with knowledge of the surgical technique.
Quality controlA single surgeon performed this surgical technique, with knowledge of the posterior tibial angiosome, following the surgical technique step by step and taking into account the location of the soft tissue defect, the landmarks described in the paper, and the illustrations.
A surgical checklist was made, ensuring that all steps for the flap were followed.
Surgical review was performed 48h after the procedure to verify the vitality of the flap.
Pre-intervention considerations- •
This surgery is performed in patients with acute trauma. If the patient is diabetic, glycaemia is controlled.
- •
Antibiotics in open fractures, thorough pre-flap debridement, optimisation of haemoglobin levels greater than 10g/dl, co-operative management with pain clinic, culture-directed antibiotic management in case of infection.
- •
Prophylactic antibiotic 2g IV cefazolin 1h prior to the procedure.
Anaesthesia is delivered according to the anaesthesiologist's criteria, with the patient in supine decubitus; no augmentation equipment is required, a routine tourniquet is not used, because the posterior tibial pulse should be checked or a vascular study performed to demonstrate vessel patency, avoid intraoperative use of tranexamic acid and peripheral vasoconstrictors, maintain mean arterial pressure greater than 80mmHg during the surgical procedure; surgical time varies, because reconstruction and fixation of bone lesions are performed at the same time.
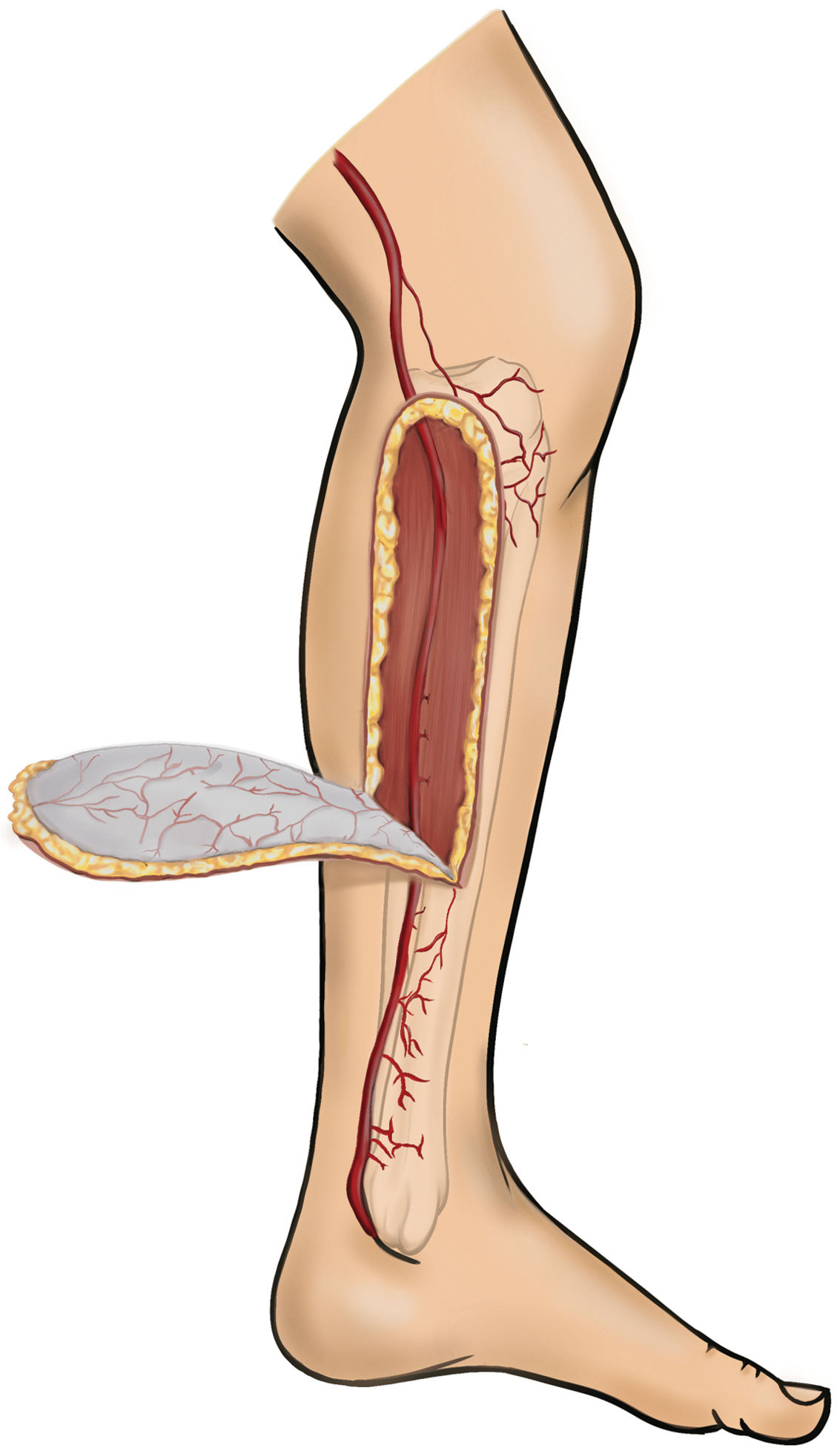
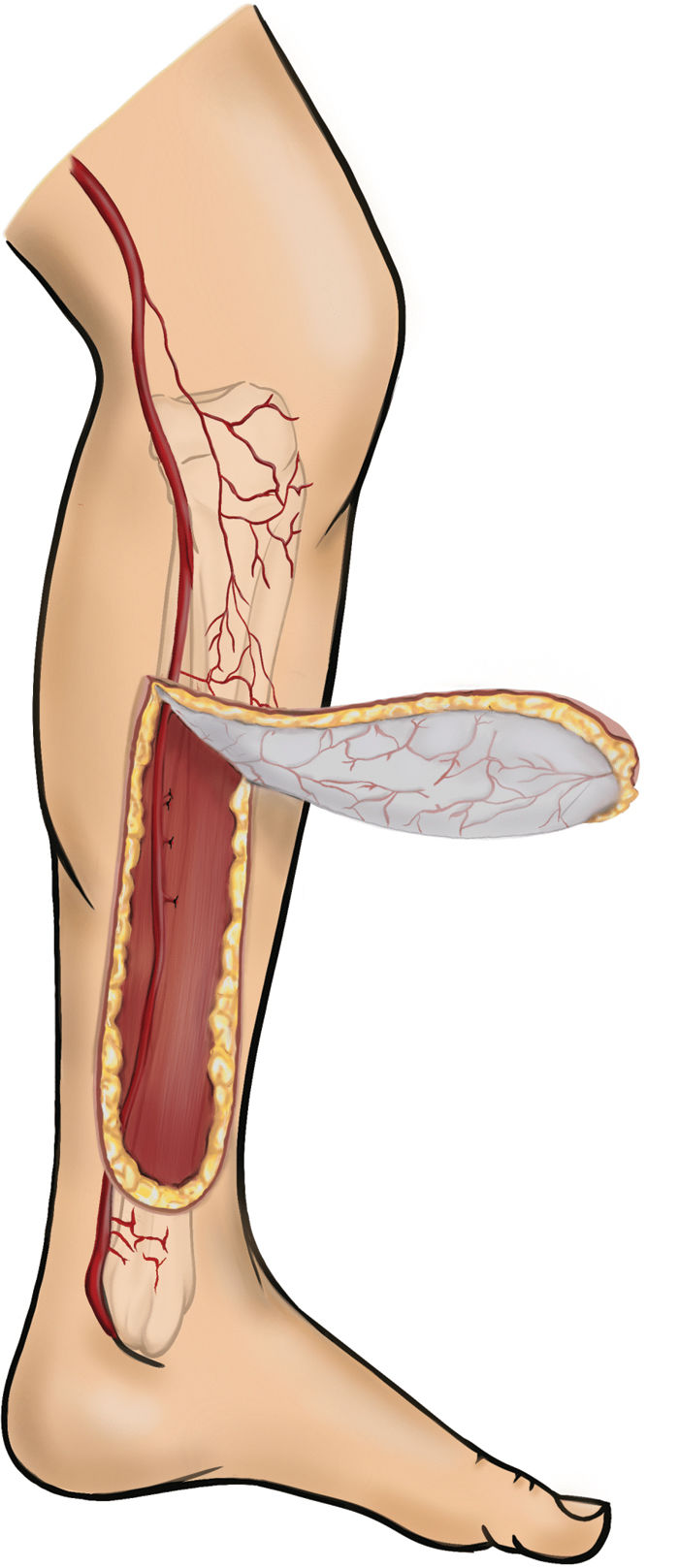
Once adequate perfusion of the angiosome of the posterior tibial artery has been verified, an additional Doppler study of the perforators is not mandatory, although it is considered a valuable tool, because the anatomy of the perforating branches supplying the angiosome of the posterior tibial artery is constant10,11 and this resource is not widely available in Latin America.7 In cases in which a decrease or loss of posterior tibial pulse is suspected, CT angiography may be useful. The flap can be taken in different ways, depending on the defect: it can be a flap with distal-based main perforators, which is ideal for defects of the proximal or medial third of the tibia (Fig. 2), or it can be with proximal-based main perforators, ideal for distal tibial defects (Fig. 3).
Once the base of the flap has been identified, the main point, which is the posterior border of the tibia, is taken as a landmark; the flap is marked considering that the posterior incision is located 5cm from the posterior border of the tibia and the anterior incision is located longitudinally with respect to the medial region of the tibial diaphysis; the extent of the incision depends on the base of the flap and the size of the defect (Fig. 4).
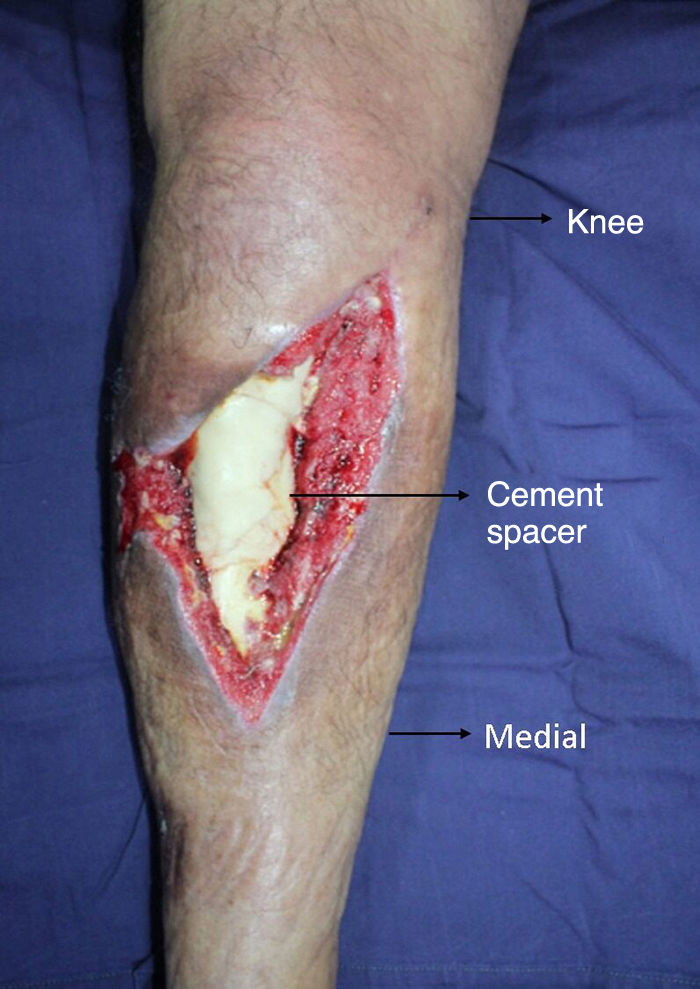
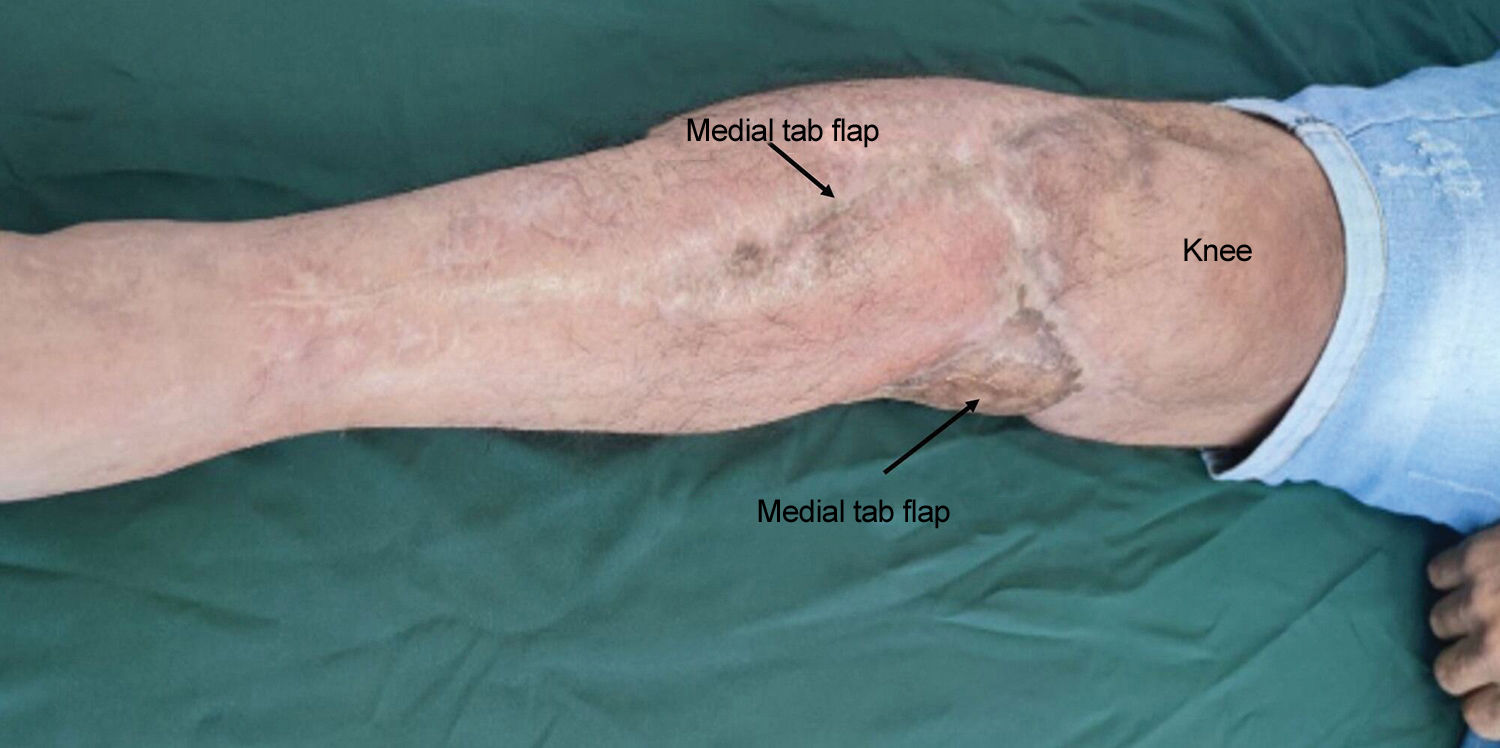
First the posterior skin incision is made and the subcutaneous cellular tissue is identified down to the fascia; the subfascial flap is dissected to avoid injury to the perforators, the dissection is completed to the anterior edge of the flap, the direct cutaneous perforators are ligated if necessary; once the subfascial plane has been identified and dissected, the flap is completed in its proximal or distal portion, according to the previous surgical planning. The tab is then rotated towards the anterior region of the tibia to cover the soft tissue defect (Figs. 5 and 6).
It is important to note that all patients underwent bone and soft tissue reconstruction in the same surgical procedure, so no immobilisation was used to protect the flap; all donor sites were covered with skin flaps, with no donor site morbidity.
Post-intervention considerations- •
The flap is covered with sterile dressings and the donor site is covered with sterile gauze soaked in petroleum jelly. It is not routinely immobilised with a splint because bone reconstruction is always performed during the same surgical procedure.
- •
Weightbearing as tolerated as well as active and passive mobility of the joint are started from the first day; ambulation is indicated.
- •
The flaps and skin grafts in the donor area are checked 48h postoperatively.
- •
Control at 2 weeks, 3 months, and 6 months.
- •
Imaging of the fracture. Clinical monitoring of the healing process.
Follow-up information for each patient was recorded directly by the orthopaedists in the Excel database.
Statistical analysis was performed using SPSS version 28 software (IBM Corp., Armonk, NY, USA), which consisted of univariate analysis using absolute and relative frequency measures for qualitative variables and measures of central tendency for quantitative variables. A bivariate analysis was then performed, comparing groups using χ2 to establish differences in categorical variables and mean differences using Student's t-test for quantitative variables. Regression analysis adjusted for variables matched through PSM was used to determine differences in outcome results between cohorts. A significance level <.05 was used.
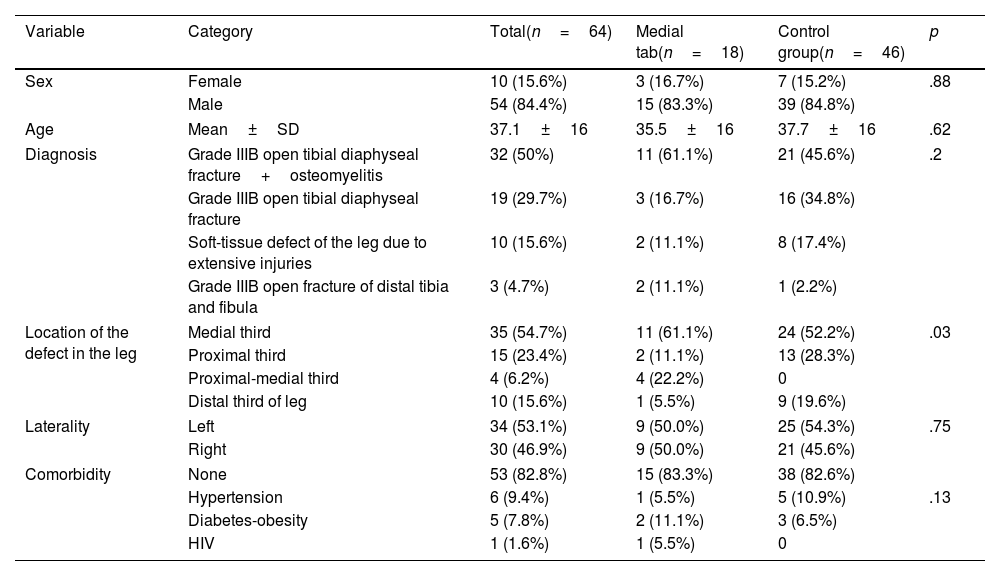
ResultsSocio-demographic and clinical characteristicsTable 1 shows the homogeneity in the comparison groups. Most of the patients analysed were male (54 cases [84.4%]), the mean age was 37.1±16 years, mainly with a diagnosis of open tibial diaphyseal fracture grade IIIB+osteomyelitis (32 cases [50%]), and 53 (82.8%) patients had no associated comorbidities. Regarding the location of the defect, it was recorded that in most (35 cases [54.7%]) it was in the medial third of the leg, followed by the proximal third (15 cases [23.4%]), and the distal third (10 cases [15.6%]). A higher proportion of defects in the distal third was found in the control group flaps (9 cases [19.6%]) than in the medial tab flap group (1 case [5.5%]) (p=.03).
Sociodemographic and clinical characteristics.
| Variable | Category | Total(n=64) | Medial tab(n=18) | Control group(n=46) | p |
|---|---|---|---|---|---|
| Sex | Female | 10 (15.6%) | 3 (16.7%) | 7 (15.2%) | .88 |
| Male | 54 (84.4%) | 15 (83.3%) | 39 (84.8%) | ||
| Age | Mean±SD | 37.1±16 | 35.5±16 | 37.7±16 | .62 |
| Diagnosis | Grade IIIB open tibial diaphyseal fracture+osteomyelitis | 32 (50%) | 11 (61.1%) | 21 (45.6%) | .2 |
| Grade IIIB open tibial diaphyseal fracture | 19 (29.7%) | 3 (16.7%) | 16 (34.8%) | ||
| Soft-tissue defect of the leg due to extensive injuries | 10 (15.6%) | 2 (11.1%) | 8 (17.4%) | ||
| Grade IIIB open fracture of distal tibia and fibula | 3 (4.7%) | 2 (11.1%) | 1 (2.2%) | ||
| Location of the defect in the leg | Medial third | 35 (54.7%) | 11 (61.1%) | 24 (52.2%) | .03 |
| Proximal third | 15 (23.4%) | 2 (11.1%) | 13 (28.3%) | ||
| Proximal-medial third | 4 (6.2%) | 4 (22.2%) | 0 | ||
| Distal third of leg | 10 (15.6%) | 1 (5.5%) | 9 (19.6%) | ||
| Laterality | Left | 34 (53.1%) | 9 (50.0%) | 25 (54.3%) | .75 |
| Right | 30 (46.9%) | 9 (50.0%) | 21 (45.6%) | ||
| Comorbidity | None | 53 (82.8%) | 15 (83.3%) | 38 (82.6%) | |
| Hypertension | 6 (9.4%) | 1 (5.5%) | 5 (10.9%) | .13 | |
| Diabetes-obesity | 5 (7.8%) | 2 (11.1%) | 3 (6.5%) | ||
| HIV | 1 (1.6%) | 1 (5.5%) | 0 | ||
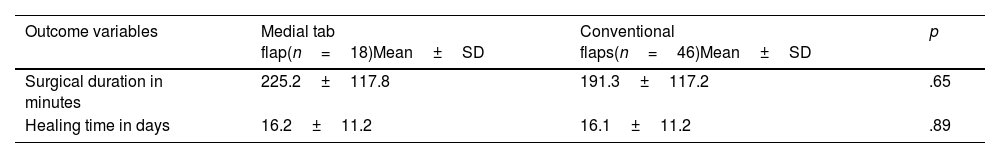
Surgical time. Comparing the surgical time used in the groups, the average time for tab flap was 225.2±117.8min, and for the other flaps it was 191.3±117min (p=.65), showing that there was no statistically significant difference between the groups (Table 2).
Healing. Complete healing was achieved in 100% of the flaps in both groups, adequately covering the soft tissue defects on the anterior aspect of the leg.
Healing time. Regarding healing time, both groups took an average of 16±11.2 days to achieve healing, and no statistically significant differences were found between the groups (p=.89) (Table 2).
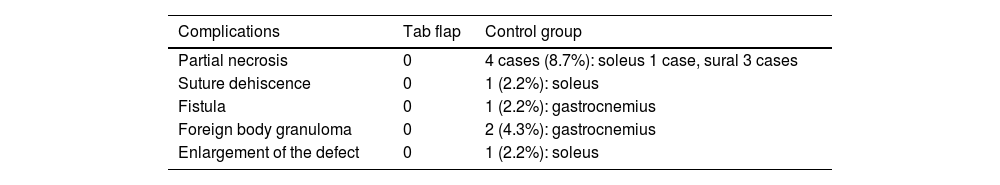
ComplicationsNo complications were found in the medial tab flap group. In the control group, 4 subjects (8.7%) had partial flap necrosis, of which 3 corresponded to sural flap and one case to soleus flap; the location of the defect was in the proximal third in 2 cases, and in the distal third in the other 2 cases. One patient with a soleus flap developed dehiscence, and in one case an additional flap needed to be implanted due to enlargement of the defect in the medial third of the leg. In the gastrocnemius flap, one fistula and two granulomas occurred at the surgical site (Table 3).
No patient required reintervention due to aesthetic problems related to the fold at the base of the flap.
DiscussionReconstruction of soft tissue defects at the level of the anterior aspect of the leg poses a challenge for surgeons. Therapeutic options vary according to the patient's needs, ranging from muscle, or fasciocutaneous, flaps to free flaps; the latter have revolutionised the treatment of soft tissue defects. However, free flaps involve complex procedures that require mastery of microsurgical techniques, demanding subspecialist training and advanced technology in magnification skills, which are not available in all therapeutic centres.2,6,12
Therefore, it is important to note that muscle and fasciocutaneous flaps are also an excellent option that can be implemented by any orthopaedic surgeon.
Sociodemographic and clinical characteristics were homogeneous between the comparison groups, mostly young adults (37.7±16 mean), 54 males (85%) and 53 patients without comorbidities (82.8%). It is important to note that these sociodemographic and clinical conditions are key elements for prognosis and achieving a successful response in soft tissue defect coverage11; in particular, a history of diabetes, smoking, and peripheral vascular disease have been associated with worse healing and a higher rate of complications,13–15 and even considered contraindications for local flaps.16 Similar data were found in studies by Akhtar and Hameed,16 Luo et al.,17 Economides et al.,18 and Zweifel-Schlatter et al.,19 in which most were male, young adults with a mean age of 31, 41.9, 49.9, and 51.7 years, respectively.
All flaps in both the tab and the control group survived and achieved complete healing; however, a low percentage of 9% (1 case of soleus and 3 of sural) in the controls had partial necrosis, which subsequently healed. These outcomes can be attributed to multiple factors,20 including comorbidities, local vascular disturbances,16 patient anatomy, mechanism of trauma, and previous soft tissue injury, including muscle, with evidence of the efficacy of the medial tab flap in resolving soft tissue defects in the anterior aspect of the leg, as a result of the high irrigation that anastomoses (vessels of the same calibre) of adjacent territories provide to the fasciocutaneous flaps.10 The medial tab flap is based on the angiosomes of the posterior tibial artery and receives important anastomoses from the territory of the descending genicular artery in its proximal portion and from the territory of the peroneal artery in its distal portion, which must be taken into account when designing the flap, seeking to preserve them to achieve adequate healing and vitality of the flap. Similar data to those of this study were reported by Roberts and Desilva,9 where 94% of their retrograde sural fasciocutaneous flaps survived with 100% viability; one flap had skin necrosis of 30%, but subsequently healed with epithelialisation on the intact fascia.16 In the study by Akhtar and Hameed,16 who used a distally based sural artery fasciocutaneous flap in 84 patients with soft tissue defects, only 78.5% (66 flaps) survived completely, 7% (6 flaps) had marginal necrosis, 9.5% (8 flaps) had complete necrosis, and 4.8% (4 flaps) had infections.
The mean healing time for the two groups was 16 days, with no significant differences between the flaps. Other studies, such as that by Dhamangaonkar and Patankar,21 reported a mean healing time of 20.88±6.71 days among their population operated with a sural fasciocutaneous flap, in contrast to the study by Friedrich et al.,5 in whose population operated using a fasciocutaneous flap with upper base, they recorded healing of the flap over the defect at 6 weeks postoperatively. Wider intervals were found between the patients of Donski and Fogdestam,22 with a distally based fasciocutaneous flap from the sural region, and those of Wee,23with a reverse pedicle anterior tibial flap, with healing times of 10 days to 3 months and 2 weeks to 3 months, respectively. The differences recorded between the healing times in our study population and those reported by other authors may be related to the reconstructions performed at the time of surgery and the presence of comorbidities that affect healing, such as diabetes mellitus and smoking.
The average surgical time for medial tab flaps and conventional flaps did not show statistically significant differences. However, the times taken to perform the flaps for the patients in this study were longer than those reported in other studies, such as that of Dhamangaonkar and Patankar,21 who found that the average duration of surgery for reverse sural fasciocutaneous flaps was 121.29±31min in total; Erdmann et al.24 reported an average duration of 1.7h for their population treated by islanded distally based fasciocutaneous flap, and Bullocks et al.15 reported an average of 287min (range 211–347min) for the reverse fasciocutaneous flap, similar to the surgical time in this study.
No complications were found in the medial flap group: in the soleus flap group there were 2 cases (4%), one with suture dehiscence and one requiring additional flap placement due to an increase in defect size. In the gastrocnemius flap group, there was one case (2%) with fistula and 2 cases (4%) with foreign body granuloma. However, the complications were not major and did not hinder the healing process. Other authors have reported various complications, such as Wee,23 who applied an anterior tibial flap with reverse pedicle and recorded venous congestion in 50% of cases (3 patients) and marginal necrosis in 33.3% (2 cases); Dhamangaonkar and Patankar21 reported 8.8% (9 cases) of marginal necrosis among their population treated with a reverse sural fasciocutaneous flap with skin pedicle, while Concha et al.12 recorded 7.7% (one case) of complete flap loss and 15.4% (2 cases) of epidermolysis, caused by deep venous congestion, in their patients treated with a lateral supramalleolar flap.
It is important to note that there may be difficulties in salvaging the flap we investigated, being fasciocutaneous, given the impossibility of visually evidencing compromised vascularisation of the artery that nourishes the flap, and that tissue is dissected according to the anatomical knowledge of the area, which in this case consists of numerous anastomoses. To address these obstacles, we implemented measures and precautions during the surgical process. Failure of fasciocutaneous flaps may be due to factors such as recurrence of infections,25 venous insufficiency, errors in technique, and diabetes mellitus.16
The results described in this study demonstrate that this type of flap is effective due to the subdermal flow with abundant vessels, which favours its viability as long as there are no traumatic lesions in the angiosome pathway.
LimitationsA larger number of cases operated on using a medial tab flap has been considered for future studies, which will allow more accurate population-based inferences to be made.
The surgical times recorded in the population studied included not only the time for dissection and coverage with the flaps, but also included the time for bone reconstruction, increasing the average duration of the operations. For future work, only surgical time relating to the flap will be taken into account.
It should be noted that, although more complications were reported in the control group, a bias may have occurred, as the location of soft tissue defects in the distal area increases the risk of complications.
We consider it appropriate to compare the results of this procedure with other types of flaps, such as the propeller.
Furthermore, including the variable of the size of the soft tissue defect and the size of the flap should also be considered.
ConclusionThe medial tab flap technique is as effective as the conventional sural, soleus, and gastrocnemius flap technique, with a high survival rate, complete healing, similar healing time, and absence of major complications in this study group. This technique, despite its limitations, can be performed by an orthopaedic surgeon who is not trained in microsurgical techniques, which enables problems to be solved in any hospital with an orthopaedic service. This option also improves the quality of life of patients with soft tissue defects in the leg, and by providing timely therapeutic options reduces the risk of long-term bone exposure complications, such as infection, and decreases the possibility of catastrophic outcomes, such as amputation.
Level of evidenceLevel of evidence ii.
Ethical considerationsThis research was approved by the institutional ethics committee in accordance with the ethical standards recognised by the Declaration of Helsinki, classified as ‘no risk’ research as per Resolution 8430 of 1993 of the Colombian Ministry of Health. Informed consent was obtained from all patients who participated in the study. The information collected was handled solely for the purposes of this study, protecting the confidentiality of the identification data of the patients involved.
FundingNo specific support from public sector agencies, commercial sector, or not-for-profit organisations was received for this research.
Conflict of interestsThe authors have no conflict of interest to declare.
The authors would like to thank Andrea Pilar Arévalo for the illustrations of the medial tab flap, which allow a graphic understanding of the anatomical principle of the intervention in this study.