Osteoporosis, and the consequences derived from it, such as fragility fractures, constitute a growing public health problem. Suffering from a fracture of this nature is the main risk factor for suffering a new fracture.
It is documented that vertebral compression fractures lead to significant morbidity and mortality, in the short and long term, as well as other complications, such as sagittal imbalance and hyperkyphosis of the segment. However, we have not found documentation that analyzes the medium and long-term consequences of these injuries, assessing the type of treatment used, and the economic impact they represent.
The purpose of this review is to analyse the main recent literature on the subject and make a breakdown of the consequences of these fractures in various spheres, such as economic, quality of life, sagittal balance and radiographic parameters, pain or mortality; as well as a brief analysis of epidemiology and natural history.
ConclusionOsteoporotic fractures constitute an emerging problem, both in the medical and economic fields. The consequences and sequelae on the patient are multiple and although surgical options offer good long-term results, it is necessary to properly select the patient, through multidisciplinary teams, to try to minimise potential complications.
La osteoporosis, y las consecuencias derivadas de la misma, como las fracturas por fragilidad, constituyen un problema creciente de salud pública. Padecer una fractura de esta índole es el principal factor de riesgo para sufrir una nueva fractura.
Está documentado que las fracturas vertebrales por compresión conllevan una importante morbimortalidad, a corto y largo plazo, así como otras complicaciones, como un disbalance sagital y una hipercifosis del segmento. Sin embargo, no hemos encontrado documentación que analice las consecuencias a medio y largo plazo de estas lesiones, valorando el tipo de tratamiento empleado, y el impacto económico que suponen.
El objeto de esta revisión es analizar la principal literatura reciente sobre el tema y hacer un desglose de las consecuencias de estas fracturas en varias esferas, como la económica, la calidad de vida, el balance sagital y los parámetros radiográficos, el dolor o la mortalidad; así como un breve análisis de la epidemiología y la historia natural.
ConclusiónLas fracturas osteoporóticas constituyen un problema emergente, tanto en el ámbito médico como económico. Las consecuencias y secuelas sobre el paciente son múltiples y aunque las opciones quirúrgicas plantean buenos resultados a largo plazo, es necesario seleccionar adecuadamente al paciente, mediante equipos multidisciplinares, para tratar de minimizar las potenciales complicaciones.
Bone fragility fractures can result from a fall from standing height or be diagnosed without a history of trauma. In this group, we distinguish low energy fractures (falls on level ground or similar) as fractures with an osteoporotic profile which occur in people over 50 years of age, excluding other bone pathologies which cause bone fragility.1 This type of fracture is caused by ‘normal’ loads on a bone with low bone strength. Osteoporotic bones under specific loading conditions subjected to a ‘physiological’ force fail biomechanically.1
Vertebral fractures are one of the most frequent skeletal fractures, usually due to bone fragility.2 However, unlike other fractures, between two thirds and three quarters of these fractures go unnoticed clinically,2,3 in most cases the diagnosis being made later by imaging.4 Therefore epidemiological studies of these fractures are complicated to conduct. Biological studies of vertebral fractures have focused mainly on symptomatic vertebral fractures which, as is well known, are the least frequent of the fractures.
EpidemiologyOsteoporosis is the most prevalent metabolic bone disease in the world, this is especially due to the increase in life expectancy.5–8 The WHO estimates that osteoporosis affects 3.5 million people in Spain.5 The consequences of osteoporotic fractures not only affect health, per se, but also quality of life.6,7
In the United States, an estimated 1.5 million people with osteoporosis will suffer a fracture, 50% of which are vertebral fractures, twice as many as hip fractures.8,9 The incidence of these injuries is expected to continue to rise, due to the ageing population and increased survival.7
The osteoporotic vertebral fracture, as the most frequent of all osteoporotic fractures—although many cases, being oligosymptomatic, go unnoticed6,7,10—, has an incidence estimated by the European Prospective Osteoporosis Study at 1,400,000fractures/year, equivalent to 20–25% of postmenopausal women over 50 years of age.5 Its prevalence in Europe is between 18% and 26%, generally in older women.10
Vertebral fractures in people under 50 years of age are more frequent in men. However, from the age of 60 years and especially from the age of 70 years onwards, the risk of fracture is higher in women.2,5,11 The incidence of new vertebral fractures in people over 50 years of age is 10.7/1000 population in women and 5.7/1000 in men, respectively.5,6 The prevalence increases from 3% in women under 60 years of age to 20% in those over 70 years of age, and from 7.5% to 20% in men in the same age range.5–7 Overall, the prevalence of vertebral fracture increases with age with no distinction in terms of race or sex in the population studied.2
Furthermore, the presence of a vertebral fracture is compatible with a diagnosis of osteoporosis, even in the absence of bone densitometry, and therefore indicates pharmacological treatment.2,5,10
PathogenesisA distinction must be made between the variables of bone quantity and bone quality. While the quantity of bone depends directly on its mineral density (BMD), its quality depends on variables such as the chemical composition of the organic and inorganic materials that make up its matrix and how the spatial structuring of these materials occurs, all of which are dependent on bone remodelling.12 A normal biomechanical pattern is characterised by normal BMD, by normal structural and material quality and, above all, by bone strength that is adequate for the mechanical function that the bone has to perform. Alterations in these variables increase the risk of fragility fractures.
In postmenopausal osteoporosis, bone remodelling is accelerated leading to a decrease in BMD and an alteration in the structural and material quality of the bone.13 This phenomenon is also present, but with a different intensity, in healthy elderly people: the older they get, the lower the bone resistance and the greater the risk of fracture. As age increases, the intensity of trauma required to produce a fracture decreases.5,14 Other factors, such as female sex, diabetes, smoking, or use of corticoids further increase this risk.14
Low-energy trauma is the most common cause of fracture. Fracture occurs when the energy applied exceeds the elastic and plastic modulus of the bone and, therefore, its capacity for deformation.15,16 This energy is generally provided by an external agent, but in the case of vertebral fractures, just the weight of the body or a muscle contraction is sufficient,17 and on other occasions it is related to a banal fall. Falls from standing height are responsible for 90% of fragility fractures in the elderly.18
The vertebrae, as well as being bones with an important load-bearing component, are greatly compromised by osteoporosis, which reduces the thickness of their cortices and reduces the number of bone trabeculae,2,19 increasing fragility. These fractures occur most frequently between levels D4-L5, but particularly those levels around the thoracolumbar hinge which transitions between the thoracic spine (more rigid) and the lumbar spine (more mobile).2 In patients with osteoporotic bones, these vertebrae can fracture simply by gestures involving a slight increase in axial load,2 especially in the lumbar spine. However, at the thoracic level, they are usually seen in the D7–D9 vertebrae, because they tend to have the greatest thoracic kyphosis, and are therefore the region with the greatest axial load.
There is a correlation between the standard deviation (SD) of BMD on DEXA and the odds ratio (OR) of fracture incidence at the lumbar level, which changes between 1.4 and 2.1 for each SD, while it is lower in other locations, such as the femoral neck or calcaneus (1.6–1.9), or the forearm (1.4–1.6).2
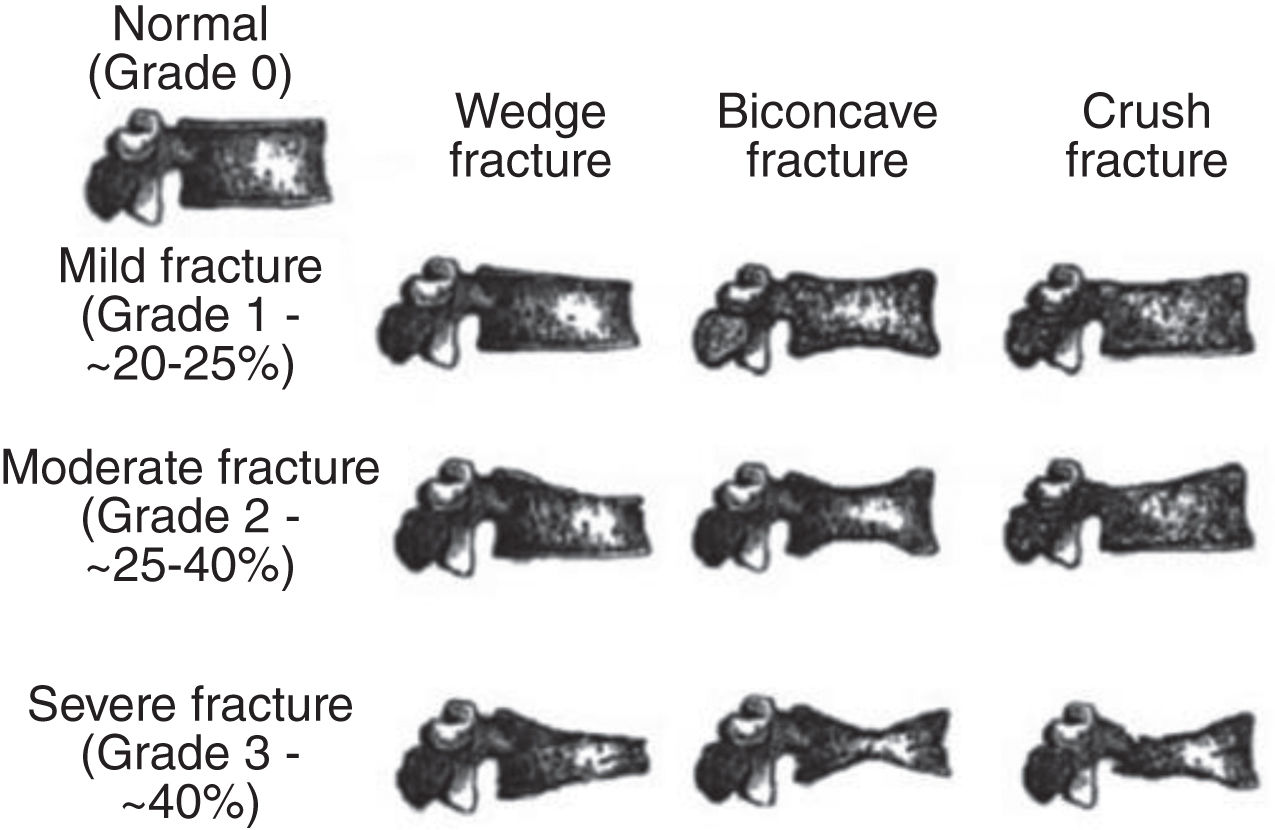
DiagnosisThe definition of vertebral fracture should be based on morphometric criteria. A vertebral fracture is considered when a decrease in vertebral height of more than 20% is identified,20,21 or a decrease of 4mm from a previous baseline X-ray. There are many morphometric assessment methods; most are based on measurements of the height of the suspected fractured vertebra in its anterior, middle, and posterior portions compared to adjacent healthy vertebrae. “Wedge”, “biconcave”, or “pancake” shapes are classically recognised as radiological signs of osteoporosis. In the dorsal area, the subsidence usually occurs in the anterior part of the vertebral body, while in the lumbar area, which supports more load, there may be wedging in the anterior and posterior part. It is rare for the posterior wall to be affected, which is typical of other processes, and rarer still for neurological symptoms to be caused, although there are documented cases.22–24
These fractures generally occur in the spinal segment between D4 and L5 and, more frequently, in the most biomechanically compromised regions D11 and L1.25,26 It is rare for them to occur at higher dorsal levels, and therefore if they do, an aetiology other than osteoporotic must be considered.
Different imaging tests must be conducted to make the diagnosis and then to assist in making therapeutic decisions.
Two-plane radiography is the first line technique, the cheapest and simplest to detect these fractures,5,10,27 but it has its limitations; poor obliquity, for example, could create false images or a mild fracture could go undetected. Retrospective studies of lateral chest X-rays report a detection rate of only 50%.5,6 Furthermore, taking X-rays in a standing position or teleradiography10,28 would provide much more information because, as well as being useful for diagnosing the fracture, this could flag up sagittal or coronal profile imbalances which could determine the choice of treatment.
Vertebral morphometry (vertebral fracture assessment) has proved to be a cost-effective technique, with a sensitivity of 70–93% and a specificity of 95% in the diagnosis of moderate-severe fractures, especially of D4-L4. Vertebral morphometry allows us to diagnose 94% of grade 2 and 3 fractures.5
Computed tomography should not be widely used as a first diagnostic test. Some studies show that many mild vertebral fractures were not diagnosed by radiologists when performing chest and abdominal CT scans5 although they could be of interest after diagnosis for surgical planning or to assess retropulsion to the spinal canal.28
MRI and bone scan can be useful in the initial stages, especially in the case of fractures that are not visible on X-rays.5,10 They make it possible to estimate progression time, especially when there is no associated blunt trauma.5 MRI is the technique that shows the earliest changes,5,10 while bone scan can take up to 7 days to show changes.5 MRI also provides more information if occupancy of the spinal is suspected.27
FDG-PET can help to differentiate between insufficiency fractures and pathological fractures, due to the high uptake of FDG in the latter.5,27
In addition to those mentioned above, DEXA densitometry and the FRAX tools can help determine the risk of new fractures6,19 so that pharmacological treatment can be initiated to prevent them.
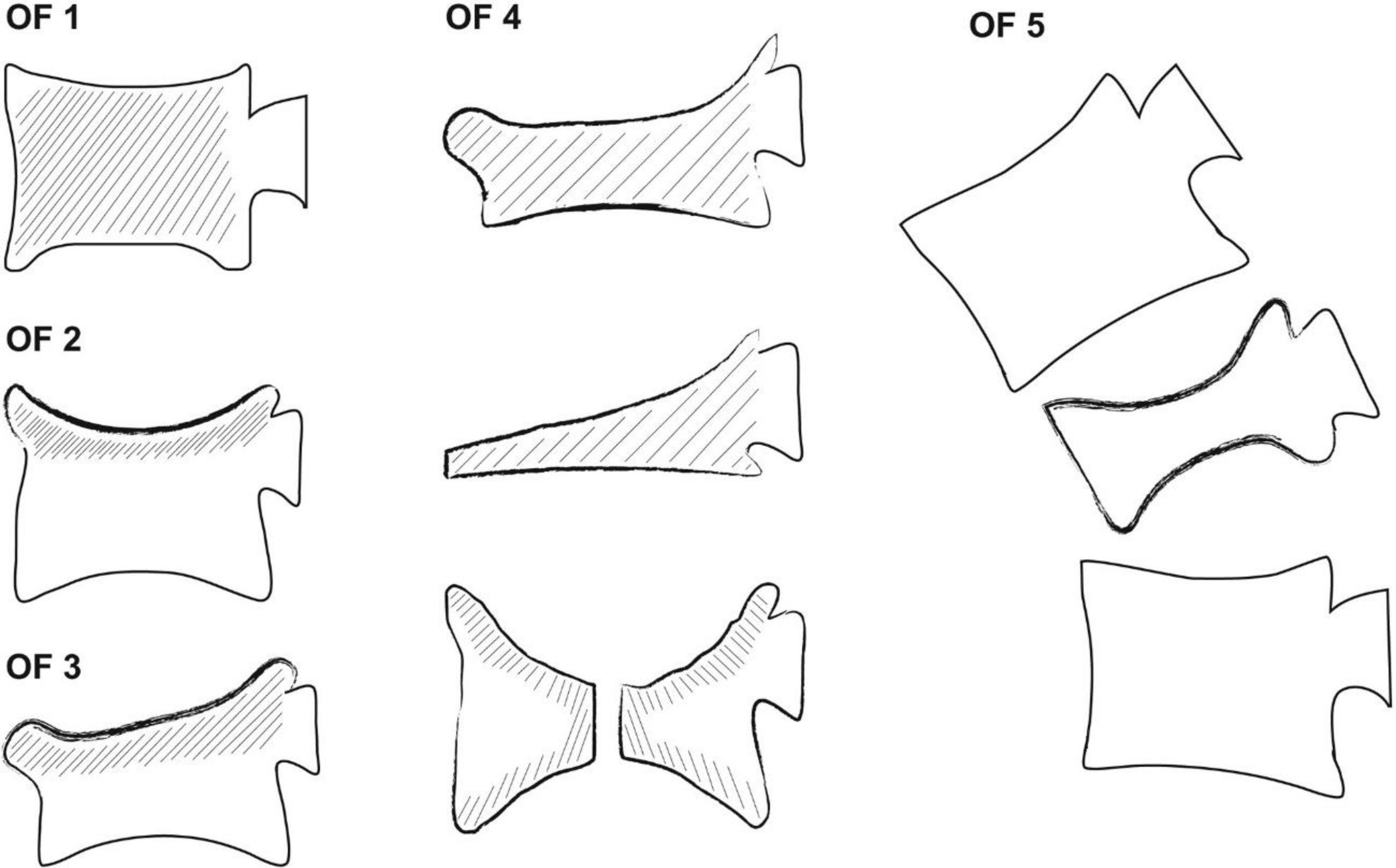
These tests, undoubtedly, in addition to diagnosis, will allow us to classify these lesions morphometrically.2,10,27–29 The Genant classification5,27 is based on the morphology of the fracture and the degree of height loss (Fig. 1). The classification of vertebral fractures proposed more recently by the German Society10,28,29 takes into account the morphology of the injury and the causative mechanism, the oedema in tests such as magnetic resonance imaging, and also provides guidance on the treatment approach (Fig. 2).
The Genant classification of osteoporotic fractures.5
Classification of osteoporotic fractures proposed by the DGOU.28
The natural history of a patient experiencing a fragility fracture, vertebral or not, is to suffer further fractures, including the dreaded hip fracture.2,5,6,10,30–35 All patients with this type of fracture have low bone density by definition. A vertebral fracture quadruples the risk of a new vertebral fracture, and doubles it for a hip fracture.2,5,19 The risk of new fractures is 7–10% in the first year and up to 18% in the first 2 years.5 If the patient is over 75 years of age, the 2-year risk increases to 25%.5,14 Other factors, such as female sex, diabetes, smoking, or corticosteroid use further increase this risk.14
It is the obligatory task of the traumatologist, and the multidisciplinary teams dealing with these injuries, to initiate treatment for osteoporosis with the aim of preventing new insufficiency fractures2,5,6,10,19,27,30–34 and to rule out other underlying endocrine disorders, such as hyperparathyroidism.36 There are various algorithms for the management of bone fragility and prevention of fractures, with various different pharmacological alternatives, depending on bone density and analytical parameters, such as calcium, renal function, or vitamin D.19 It is not the purpose of this review to describe in detail the pharmacological treatment options.
However, the sagittal profile of these patients is compromised, to a greater extent the more vertebral compression fractures they suffer or the more severe they are,2,7,10 which will have a negative impact on their quality of life and survival. The hyperkyphosis caused by the fractures, especially in the thoracic segment, alters sagittal balance, reduces the space between the ribs and the iliac blades, which leads to reduced respiratory capacity, deterioration of pulmonary function with volumetric restriction, imbalance, gastro-oesophageal reflux disease, a tendency to depression, limits quality of life, and predisposes to falls. Taken together, these changes result in increased mortality from these fractures.2,6,7,10
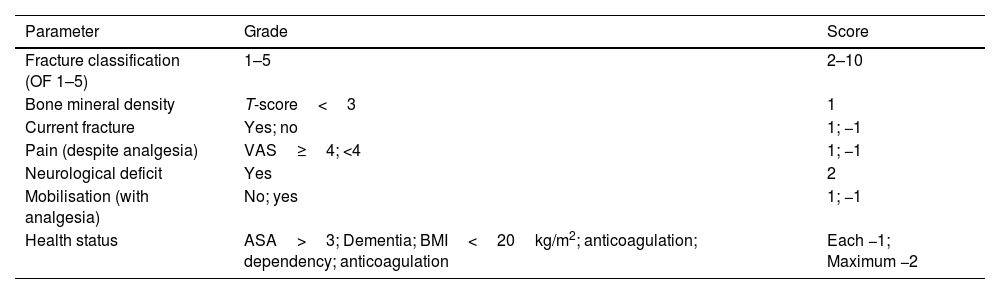
The main objective of any treatment should be the rapid mobilisation of the patient, as well as optimal pain control.28 Other aspects to consider would be the restoration of stability, correction of the kyphotic deformity, and decompression of the neural canal.29 In 2018, the Spine Section of the German Society for Orthopaedics and Trauma28 defined the treatment of choice for osteoporotic compression fractures based on OF classification, BMD, radiographic progression (preferably X-rays taken in standing position), pain, presence or absence of neurological deficits, mobilisation, and general health status, according to the ASA anaesthetic risk. Thus, a decision algorithm was established that has subsequently been used by other studies, such as Burguet Girona et al.29 in 2021. A score of less than 5 points indicated conservative treatment, while radiographic progression, or a score of more than 6, recommended surgical treatment.
The proposed score is shown in Table 1.
German Society for Orthopaedics and Trauma score.
| Parameter | Grade | Score |
|---|---|---|
| Fracture classification (OF 1–5) | 1–5 | 2–10 |
| Bone mineral density | T-score<3 | 1 |
| Current fracture | Yes; no | 1; −1 |
| Pain (despite analgesia) | VAS≥4; <4 | 1; −1 |
| Neurological deficit | Yes | 2 |
| Mobilisation (with analgesia) | No; yes | 1; −1 |
| Health status | ASA>3; Dementia; BMI<20kg/m2; anticoagulation; dependency; anticoagulation | Each −1; Maximum −2 |
ASA: American Society of Anaesthesiologists Risk Classification; BMI: body mass index; VAS: Visual Analogue Scale.
0–5 points=conservative; 6 points=surgical or not; >6 points=surgical.
Orthopaedic treatment brings together a wide range of therapeutic alternatives which, according to the literature, could include initial bed rest, analgesic medication, physiotherapy and rehabilitation, and immobilisation with bracing.8,10,27,29,32,35,37
It is recommended that bedrest should be as short as possible.28 Regarding bracing, there is controversy as to which brace would be the most appropriate or whether or not it is strictly necessary.10,28,34 In fact, the 2010 AAOS guidelines35 cannot establish sufficient evidence for or against the use of bracing in patients with compression fractures treated conservatively. If used, it would be recommended for about 6–8 weeks, until pain has resolved.10 Zileli et al.36 suggest that all patients would notice analgesic improvement with the conservative approach within 3 months. However, at the end of the first year of treatment, up to 40% of them would still be in pain.
Surgical treatment, however, should be indicated to improve gait biomechanics, when pain is refractory to medical management, when there is great retropulsion of the fragments, when there is neurological deficit, and to reconstruct the sagittal and coronal profile,28,36 when these are altered, generally with a kyphotic tendency and a positive sagittal imbalance. To that end, the German Society28 recommends X-rays, preferably in standing position to obtain more mechanical information on the spine and to be able to define the surgical indication. It is important to specify that these injuries in patients with these characteristics of fragility require a specialist multidisciplinary team. The characteristics of bone fragility in these patients often make it necessary to use augmentation techniques on the screws, such as cementing28,31,38,39 to increase the pull-out strength of the screw, which in some series is estimated at 278%.30 The delicate medical situation of these patients, who usually have different comorbidities, has resulted in increasing use of percutaneous fixation techniques, which is expected to continue in the coming years as they are managing to reduce morbidity.29
However, if the sagittal profile is satisfactory, or shows little alteration, and we only want to manage refractory pain, simple cementation techniques such as vertebroplasty or kyphoplasty are valid alternatives, although not free of complications.29,40 The AAOS,35 on the other hand, gives a strong recommendation against vertebroplasty and a weak recommendation in favour of kyphoplasty for the treatment of osteoporotic fractures. Nevertheless, there are subsequent studies, albeit with less power, which do recommend these procedures, contradicting the above.37
The therapeutic decision will undoubtedly influence the results in the short and medium term and may have consequences for the impact and sequelae in the long term. It should be borne in mind that patients with fractures with stability parameters such as to consider orthopaedic treatment can undergo cementing techniques for pain control27,37,40; while complex fractures, which require surgery, may have to be treated with less aggressive procedures if the patient's circumstances do not allow for them to be managed differently.
There is unequivocal consensus in all the studies reviewed that vertebral compression fractures increase morbidity and mortality,2,5,6,10,19,32,35 regardless of the therapeutic approach taken. Schousboe in 2015 concluded that vertebral fractures can have as much morbidity as hip fractures, although between 25% and 30% are not diagnosed at the acute moment.2,5 Schousboe2 states that a vertebral fracture increases the risk of mortality 2–8-fold, the greater the number of fractures. The highest mortality is recorded at the acute moment, and then gradually decreases over the first 2 years. The greatest immediate increase is associated with the fracture per se, while in the long term it is linked to the patient's previous morbidities. This mortality appears to be higher in men than in women.2
Some studies32 state that fracture patients who undergo some type of surgical procedure presented lower mortality in the long term than those managed orthopaedically. Authors such as Burget Girona et al.29 conclude that surgical management, compared to conservative management, seems to provide better correction of the residual deformity and offer better long-term results, although they do not assess quality of life scales. Others, such as Imamudeen et al. in 2021,19 note that kyphoplasty, in addition to the evident pain relief, reduces mortality by up to 22% at 10 years versus patients with fractures managed conservatively.
Functionality, pain, and quality of lifeSchousboe2 in 2015 estimated that the average time of disability after a fracture is 158 days for lumbar fractures and 74 days for thoracic fractures, compared to 101 days for a hip fracture. He did not specify whether these times varied according to the treatment used.
The improvement in pain occurs mainly during the first 3 months, although it can last up to 6 months. However, even when the fracture consolidates satisfactorily, some of these patients may end up with chronic pain,2,9,36 some studies such as that by Zileli et al.,36 put this at 40%.
A 2016 meta-analysis by Mattie et al.9 demonstrated not only the superiority of kyphoplasty over conservative treatment in pain management, but also reported that this difference is most pronounced during the first 2 weeks after the procedure and is maintained throughout the first year. Other studies seem to support these results.41 Some, such as Wen et al. in 2021,39 even claim that kyphoplasty is superior to percutaneous fixation in pain control and functional recovery in the immediate postoperative period, probably because of the magnitude of the surgical procedure. Other percutaneous techniques, such as vertebroplasty, appear equal to kyphoplasty in pain control and, although they involve shorter operating time, achieve less radiographic improvement and have more complications such as cement leakage.37
Although not always specifically mentioned, the literature concludes that these injuries have a long-term negative impact on the patient's quality of life.6,7,31 Having one or more of these fractures reduces spinal mobility, leading to disturbances in gait mechanics, a predisposition to falls, and an increased tendency to depression.6,7 In general terms, it is estimated that these fractures compromise quality of life in more than 20% of patients over the age of 70.31
Sagittal profile, surgery, and complications arising from surgerySurgery is indicated when pain is refractory to analgesic medication, when there is great retropulsion of the fragments and/or neurological symptoms, and when gait biomechanics are abnormal and there is coronal and sagittal imbalance.28,36
The very fact of ageing deteriorates sagittal balance, increasing thoracic kyphosis and lumbar lordosis, which is undoubtedly accentuated in the presence of vertebral compression fractures.7 When the spine is affected by kyphosis, to compensate for sagittal balance, gluteal contracture and pelvic retroversion occur, which eventually prove to be insufficient. The subsequent compensatory mechanisms would involve flexion of the knees, shortening of the hamstrings, and dorsal flexion of the ankles. All of this would result in impaired gait mechanics.7
Conservative treatment of a compression fracture is a significant contributor to sagittal imbalance.7 In this regard, surgical treatment leads to an improvement in radiographic parameters compared to orthopaedic treatment.32,39,41
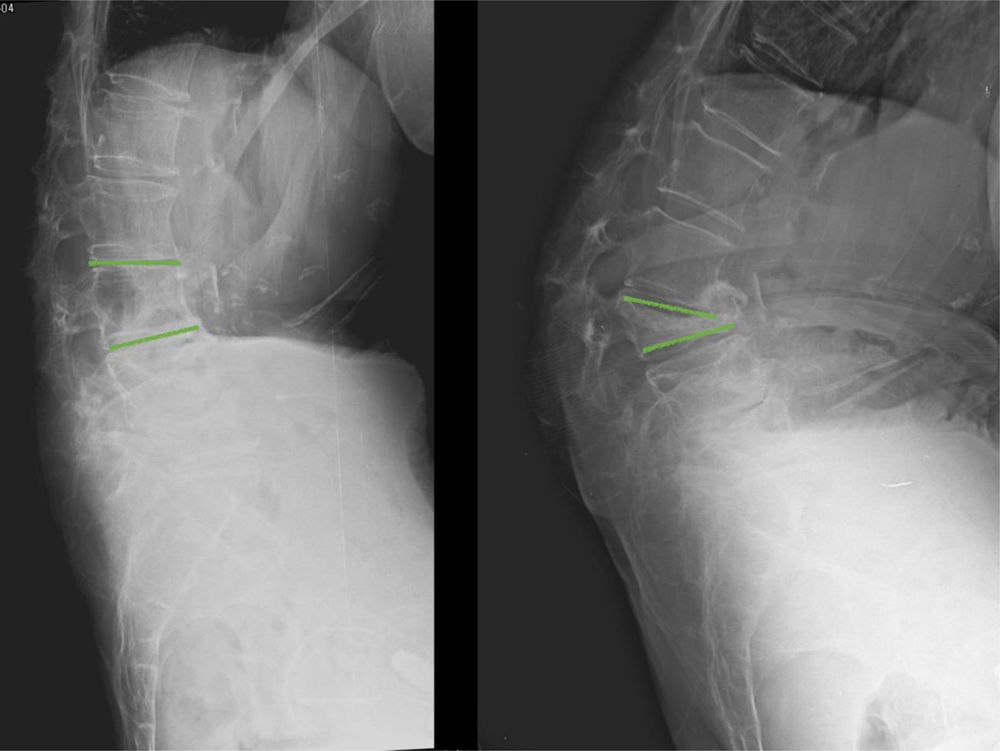
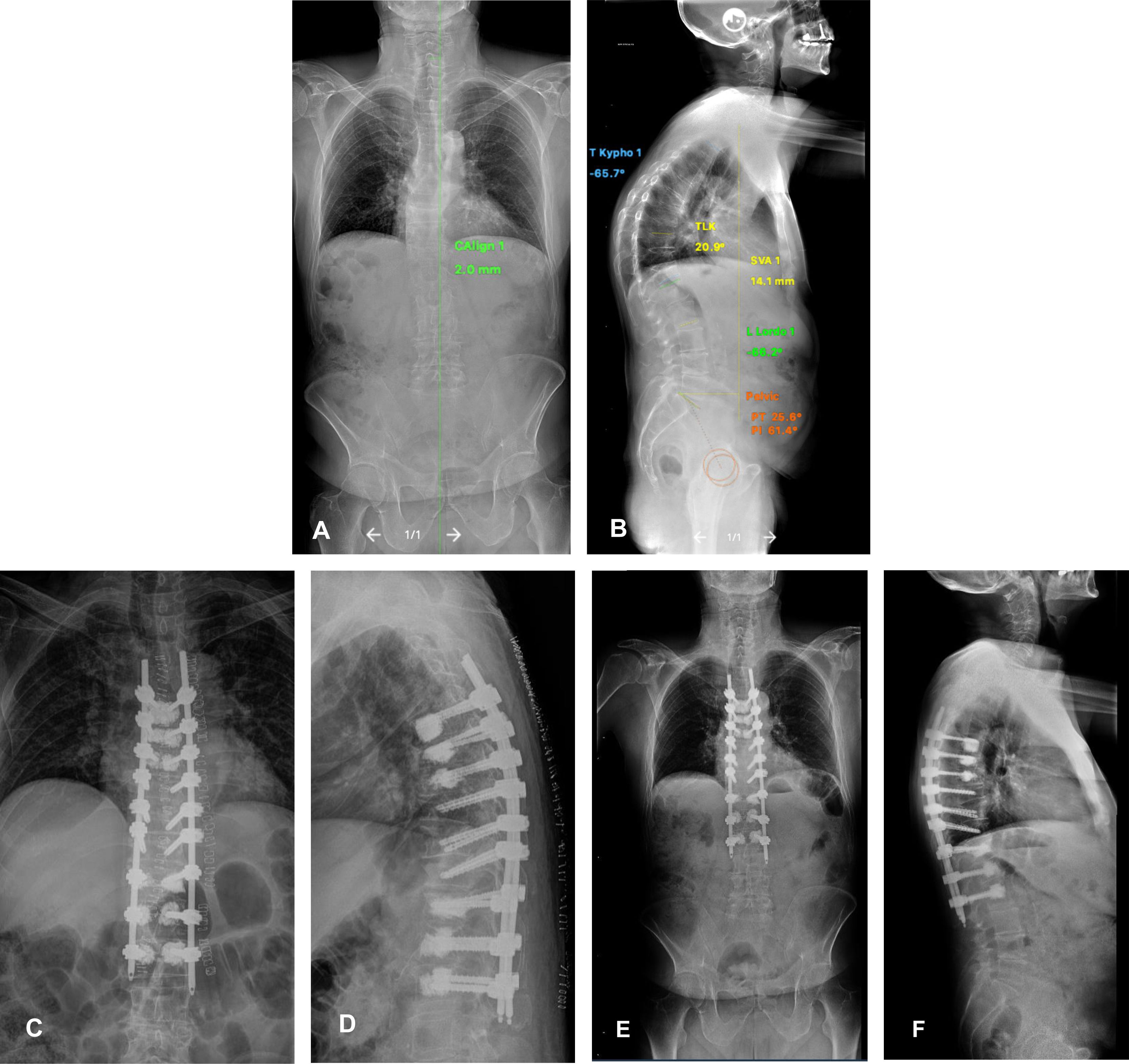
Fig. 3 shows the case of an insufficiency fracture, managed orthopaedically, which progresses to sagittal imbalance.
However, surgical treatment is also highly variable. Thus, in our therapeutic arsenal, we could use cementing techniques alone, whose main function is not so much stabilisation or improvement of the profile as pain control. Mechanically stable fractures could undergo cementation for analgesic control, if required by the patient.27,37,40 At the same time, a mechanically unstable fracture located in the thoracolumbar hinge region may require instrumentation (open or percutaneous) to stabilise the segment and restore kyphosis. The number of levels to be instrumented will depend on the location of the injury, the profile, and other parameters suggestive of instability.7,29–31,38 In this regard, the German Society28 suggests a treatment algorithm according to the fracture pattern, which can serve as a decision guide for the reader.
A retrospective study from 202332 and another study from 202139 report that surgery using vertebral instrumentation offers better results in terms of restoring vertebral height, regional kyphosis angle, and sagittal balance than kyphoplasty or vertebroplasty. In turn, kyphoplasty improves vertebral height and local kyphosis angle compared to conservative treatment.41 In the case of vertebroplasty, although it may offer symptomatic relief compared to conservative treatment, it does not differ in terms of recovery of vertebral height.32
Fig. 4 shows a clinical case of MIS instrumentation of a patient with sagittal imbalance due to vertebral fractures. Note the cement augmentation of the screws to increase screw strength.
Male, 71 years old, who suffered a fall from standing height in January 2023. Since then, he has presented with dorsolumbar pain. Images A and B show a teleradiograph showing the significant sagittal imbalance caused by multiple vertebral fractures, resulting in hyperkyphosis. Images C and D show the first postoperative X-ray. Long posterior instrumentation was performed, with minimally invasive techniques and cement augmentation of the most cranial and caudal screws. Images E and F show the first postoperative teleradiograph, at one month, where the restoration of sagittal balance is evident.
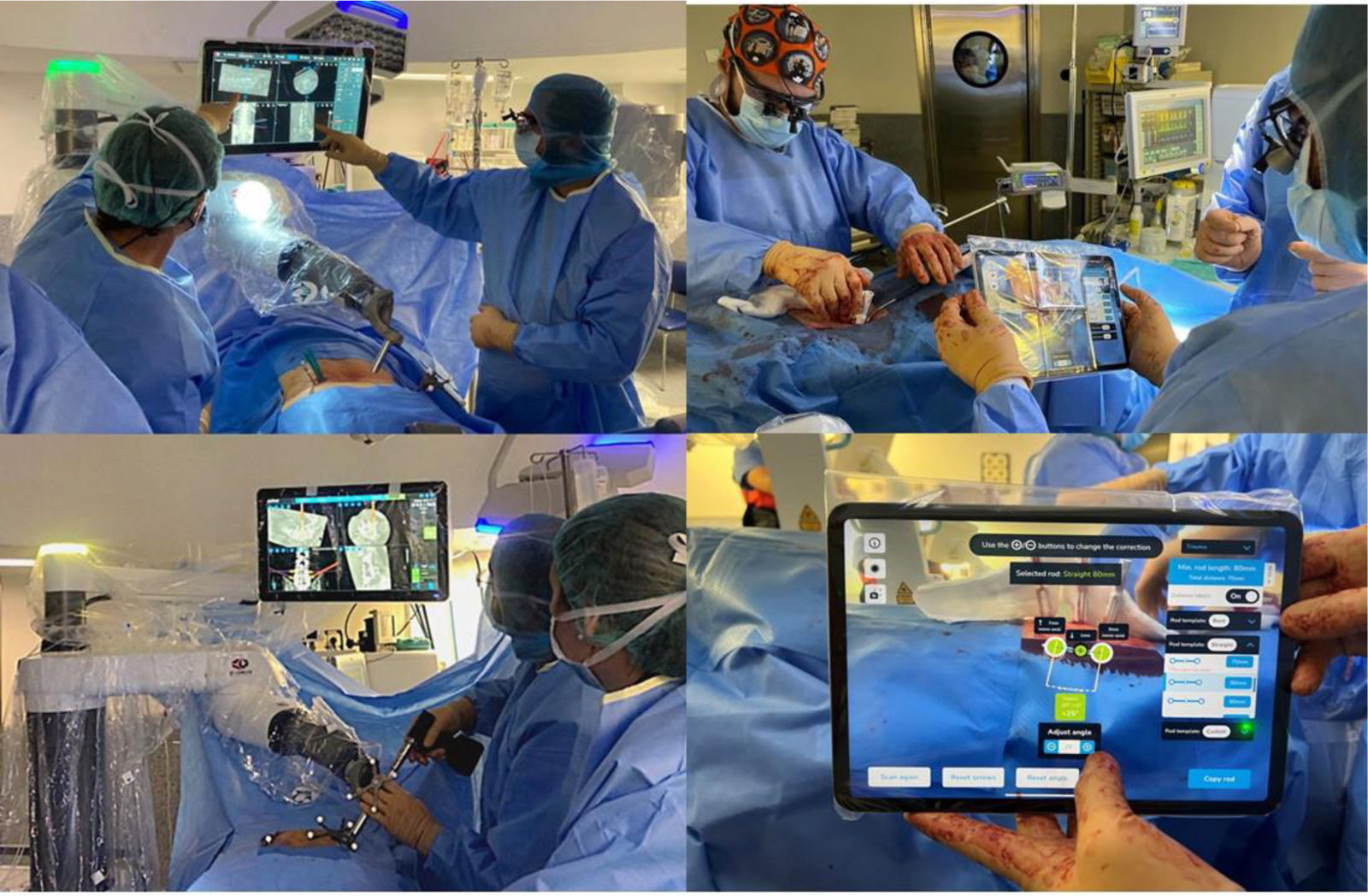
In cases with fractures requiring surgical treatment, the development of minimally invasive techniques assisted by navigation or robotic systems42 can increase the accuracy of pedicle screw placement. In addition, there are technologies based on artificial intelligence or augmented reality with which it is possible to improve the classic surgical result by intraoperative measurement of the deformity and moulding of the rod to correct the fracture.43
Fig. 5 shows the application of new technologies to these procedures.
While surgery undoubtedly improves radiographic parameters and, in the long term, also survival, it is not without risk. Appropriate preoperative selection is required of patients suffering from these fractures, who often have significant morbidities.
There are several possible complications, such as neurological injuries, cement leakage, cement embolisation in the venous drainage systems, perforation of the anterior part of the vertebral body and injury to visceral structures, haematomas, contrast leakage, etc.28
It is well known that in poor quality trabecular bone, screw loosening and implant failure is significantly higher.38,39
The fragile bone characteristics of these patients often make it necessary to use screw augmentation techniques, such as cementing28,31,38,39 to increase the pull-out strength of the screw, which in some series is estimated to be as high as 278%.30 However, one of the most reported complications, also present in isolated augmentation techniques, is cement leakage, which in this osteoporotic bone can be as high as 21.8% (6–43.1%),9,29–31,37,41 and is greater the more cement used.38 In techniques without instrumentation, vertebroplasty is associated with greater cement leakage than kyphoplasty.37 Fortunately, most of these cement leaks are asymptomatic.31 Zhang et al.14 found symptoms from leakage in only 1.2% (.2–1.9%).
Pulmonary embolism when using cement techniques is reported in 3% (.5–6.8%), while symptoms from them, or long-term sequelae, occur in only .8% (.2–1.5%).30
Another possible long-term negative impact of cementation is fracture of adjacent vertebral segments, which remains a controversial issue to this day.19 Some studies highlight an increased risk of fracture at adjacent levels2,14,29 while others state the opposite.33
The delicate medical situation of these patients, who usually have different comorbidities, has increased the use of percutaneous fixation techniques, which is expected to continue in the coming years, as they manage to reduce morbidity29 by reducing bleeding, the need for transfusion, operating times, and hospital stay without altering the functional results.
Economic impactFinally, although it is not the main objective of this work, these fragility fractures and osteoporosis clearly carry a significant economic burden for society and are a real public health problem.7 The AAOS35 states that in 2005, the economic impact of osteoporotic fractures was estimated at 17,000 million USD. In the USA, the annual expenditure directly related to vertebral fractures amounts to 1billion dollars,27 accounting for up to 5% of all economic expenditure attributed to osteoporosis.2
Vertebral fractures, unlike hip fractures, do not always require hospitalisation, and are therefore less costly to the system, accounting for 30–50% of the economic expenditure that could be attributed to them.2 It is estimated that around 40% of patients who suffer vertebral fractures will require some form of hospitalisation or residential care.2 Schousboe2 states that a vertebral fracture increases health expenditure for the 5 years following onset.
In 2021, Wen et al.39 concluded in a cost-effectiveness analysis that kyphoplasty is the best treatment for osteoporotic compression fractures.
ConclusionsVertebral compression fractures have a severe impact on all spheres, including a significant economic burden on healthcare systems. As sequelae, patients may experience chronic pain, sagittal imbalance, gait disturbance, and increased mortality. Furthermore, suffering one fragility fracture predisposes to more.
Surgical techniques appear to improve survival, quality of life, and sagittal balance in these patients, although multidisciplinary approaches are required because they are not without complications.
Level of evidenceLevel of evidence iii.
Ethical considerationsProtection of humans and animalsN/A. The authors declare that no experiments on humans or animals were performed for this research.
Data confidentialityN/A. The authors declare that no patient data appear in this article.
Right to privacy and informed consentN/A. The authors declare that no patient data appear in this article.
FundingThe authors declare that they had no funding or relationship that may have influenced the results reported in this scientific paper.
Conflict of interestThe authors have no conflict of interest to declare.