The association of ipsilateral tibia fractures has a low incidence, being up to 3.2% of total tibia fractures. Currently there is no gold standard regarding the ideal surgical treatment.
The objective of this study is to analyze the surgical treatment and the radiographic and functional results, as well as the associated complication rate of ipsilateral bifocal tibia fractures.
Material and methodsRetrospective observational study in our hospital from 2010 to 2022 of 24 patients who underwent bifocal fracture of the ipsilateral tibia. Demographic and surgical data and complications during follow-up were included.
ResultsThe 24 patients were classified into Group 1 when they presented a fracture of the plateau and distal tibia (25%), Group 2 with a fracture of the plateau and diaphysis (33%) and Group 3 with a fracture of the diaphysis and distal tibia (42%). Three patients underwent surgery with 1 implant and 21 patients with 2 implants. The average follow-up time in outpatient clinics was 2 and a half years. At one year, 22 patients (92%) had full weight bearing and 2 patients had partial weight bearing (8%) due to the sequelae of the fractures. The average time for consolidation of the diaphysis was 7.75±2 months, with no significant differences observed between Group 2 and Group 3 (p=0.06). The average time for consolidation of the metaphysis was 3.50±1.5 months, with no significant differences observed between Group 1 and Group 2 (p=0.065). Seven patients (30%) had complications during follow-up.
ConclusionsBifocal tibia fractures can be treated using a combination of intramedullary nailing and plate osteosynthesis with good long-term results, obtaining an optimal union rate and low complications. In addition, it facilitates the reduction of the fracture, thus facilitating the patient's recovery and obtaining good long-term functional results.
La asociación de fracturas ipsilaterales de tibia presenta una baja incidencia, siendo hasta el 3,2% de las fracturas totales de tibia. Actualmente no existe un patrón oro en cuanto al tratamiento quirúrgico idóneo.
El objetivo de este estudio es analizar el tratamiento quirúrgico y los resultados radiográficos, funcionales, así como la tasa asociada de complicaciones de las fracturas bifocales de tibia ipsilaterales.
Material y métodosEstudio retrospectivo observacional de 24 pacientes intervenidos de fractura bifocal de tibia ipsilateral en nuestro hospital desde 2010 hasta 2022. Se incluyeron datos demográficos, quirúrgicos y complicaciones durante el seguimiento.
ResultadosLos 24 pacientes se clasificaron en el grupo 1 cuando presentaban fractura de meseta y tibial distal (25%), en el grupo 2 con fractura de meseta y diáfisis (33%) y en el grupo 3 con fractura de diáfisis y tibia distal (42%). Tres pacientes fueron intervenidos mediante un implante y 21 pacientes mediante dos implantes. El tiempo medio de seguimiento en consultas externas fue de 2 años y medio; 22 pacientes (92%) presentaron al año carga completa y 2 pacientes, carga parcial (8%), debido a las secuelas de las fracturas. El tiempo medio de consolidación de la diáfisis fue de 7,75±2meses, sin observarse diferencias significativas entre el grupo 2 y el grupo 3 (p=0,06). El tiempo medio de consolidación de la metáfisis fue de 3,50±1,5meses, sin observarse diferencias significativas entre el grupo 1 y el grupo 2 (p=0,065); 7 pacientes (30%) tuvieron complicaciones durante el seguimiento.
ConclusionesLas fracturas bifocales de tibia son fracturas infrecuentes que en ocasiones requieren la combinación de varios tipos de osteosíntesis para obtener una reducción adecuada. En nuestra serie las fracturas más frecuentes fueron del tipo 3 (fractura de diáfisis y tibia distal). Cuando la diáfisis tibial estaba implicada se precisó de osteosíntesis combinada mediante clavo intramedular junto con placas y tornillos, obteniéndose unas tasas de consolidación, resultados funcionales a largo plazo y complicaciones similares a los descritos en la literatura.
Diaphyseal fractures of the tibia and fibula are the most frequent long bone fractures, accounting for up to 17% of all lower limb fractures.1 However, the association of ipsilateral tibia fractures is low in incidence, accounting for up to 3.2%2 of total tibia fractures. Specifically, the combination of ipsilateral tibia fractures is associated with high-energy mechanisms, and represents a therapeutic challenge due to the complexity of these injuries. The most frequent combination of fractures is of the posterior malleolus with a spiral fracture of the distal third of the tibia.3
Due to the low frequency of these fractures, there is no gold standard for the ideal surgical treatment. In the case of plate fixation, there are associated complications, such as the rate of secondary pseudoarthrosis or soft tissue involvement.4–6 For this reason, MIPO techniques have been developed to reduce the rate of soft tissue injury and infection. Some authors propose the association of plates with intramedullary nailing to facilitate fracture reduction and thus improve the patient's subsequent functionality, together with early weight bearing.7–9
The objective of this study was to analyse the surgical treatment, together with radiographic and functional results, and also the associated rate of complications of ipsilateral bifocal tibia fractures.
Material and methodsA retrospective observational study was conducted in our hospital from 2010 to 2022, in which approximately 450 tibial diaphyseal fractures were treated. Of this number of fractures, 24 patients had associated bifocal tibia fractures at different levels. The inclusion criteria were: that the patients were over 18 years old, that they had a minimum follow-up of one year, and that they had a bifocal fracture with a combination at the proximal-diaphysis, proximal-distal or diaphysis-distal level. Exclusion criteria were bifocal segmental fractures of the diaphysis, Gustilo and Anderson type IIIC fractures, and follow-up of under one year. Fractures were classified according to the AO system, according to the Gustilo and Anderson10 classification in the case of an open fracture, and by a combination of fractures according to the Keating et al.3 classification.
The fracture presented during a clinical session, and the surgeon decided, depending on the imaging tests, whether to perform osteosynthesis using cannulated screws, plates, or an intramedullary rod, as well as whether to perform osteosynthesis using one or two implants. A CT scan was requested for those patients who presented a tibial plateau fracture or a fracture at the distal level of the ankle or pilon to assess the joint. Normally, the intervention sequence would entail stabilisation of the plateau or the ankle or pilon before that of the diaphysis. If the intervention was performed using an intramedullary rod, the surgical technique of the milled suprapatellar nailing system was used.
The study was conducted in accordance with the ethical standards recognised by the Declaration of Helsinki and resolution 008430 of 1993 and was approved by the Institution's Ethics Committee. Informed consent was obtained from the patients who participated in the study.
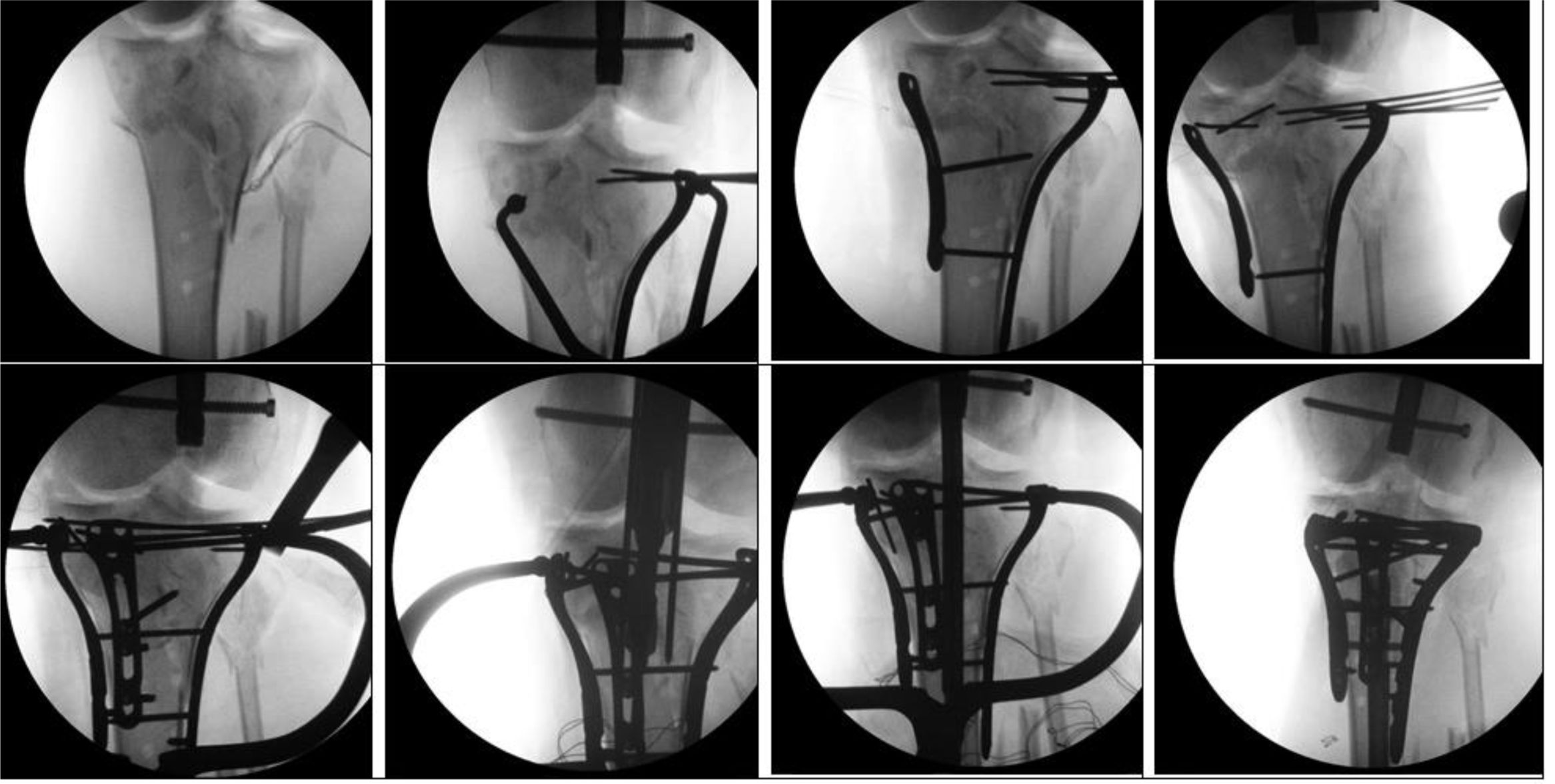
Surgical techniqueThe patient was placed supine on a conventional, radiolucent table. When the fracture involved the lateral area of the plateau, an anterolateral approach was performed, which did not interfere with the nail entry incision. When provisional joint reduction was achieved with K-wires, a LCP plate (locking proximal tibia plate or locking medial or anterolateral ankle plate if the ankle was approached first) was placed to temporarily stabilise the joint to maintain reduction while inserting the nail. Sheets were placed under the knee to maintain 10–30° knee flexion. Next, a 1cm suprapatellar incision of 2cm in length was made, with a subsequent transquadricipital incision for nail entry (Stryker T2 suprapatellar nail) and it was ensured that the nail entry did not go through the fracture area of the plateau if present. The guide was positioned and the canal was reamed to 1.5mm greater than the final desired nail thickness. The diaphyseal fracture was reduced by traction and manipulation to achieve correct alignment. When the nail was finally inserted and the distal locks were placed, the unicortical screws that held the plateau in provisional reduction were modified and changed to areas where bicortical screws could be used. In the case of a medial plateau fracture, a medial or posteromedial approach was used.
In cases of a nail-plate combination, the plate with joint reduction (plateau/pilon or distal tibia) was placed first, trying to leave the nail path free both in the anterior part of the plateau/centre of the ankle and with unicortical screws, or, if possible, anterior or posterior to the nail path in dialysis (Fig. 1).
In the case of patients with associated diaphysis and ankle-pilon, cannulated screws were sometimes used to obtain reduction of the fragments beforehand without interfering with the nail, or alternatively plates were used.
Post-operative period and follow-upAn early rehabilitation protocol was initiated, beginning with a range of motion of the knee after surgery, and the start of quadriceps strengthening. In all patients, full weight bearing was allowed from 2 months after surgery.
The patients were followed up in outpatient clinics, with assessment of clinical, radiographic and functional parameters. A control X-ray was performed with follow-up at 2 weeks, one and a half months, 3 months, 6 months, 9 months and 1 year. Radiographic alignment was determined in the lateral and anteroposterior projections. Malalignment was defined as a deformity of more than 5° in the coronal plane or more than 10° in the sagittal plane. Fracture consolidation was defined with serial radiographs requested by the presence of callus in 3 of 4 cortices on the radiographs, and if there was any doubt, a CT scan was requested to correctly assess the fracture callus. Fractures that did not meet these criteria after 9 months were defined as non-consolidated. The presence of infection was determined if there was the appearance of a fistula or persistent drainage through the surgical wound according to the criteria defined by IMC 2018.
The patient's functional abilities were determined by whether they used support products and the level of mobility they had in both the knee and ankle one year after the surgical intervention.
StatisticsThe statistical programme R-commander v 3.4.3 for Mac was used. First, the parameters were determined to follow a normal distribution using the Lilliefors test. The significance level was set at p<.05.
ResultsThere were 24 patients in total with bifocal tibial fractures, of whom 19 patients were male (79%) and 5 patients were female (21%). The mean age of the patients was 49 years (28–77 years); 17 patients had no relevant medical history. Of the remaining 6 patients, 2 patients had a history of neoplasia, one patient was a liver transplant recipient, 2 patients had diabetes mellitus, and one patient presented with alcoholism.
Regarding anaesthetic risk (ASA), 6 patients were ASA 1 (25%), 16 patients were ASA 2 (67%), and 2 patients were ASA 3 (8%). The mean BMI was 25. A total of 22 patients had a high-energy fracture and 2 patients a low-energy fracture. The fracture mechanism of 12 patients was a traffic accident, 6 patients had been run over, 2 patients had attempted suicide, 2 patients had an accidental fall and 2 patients had a fall from a scooter.
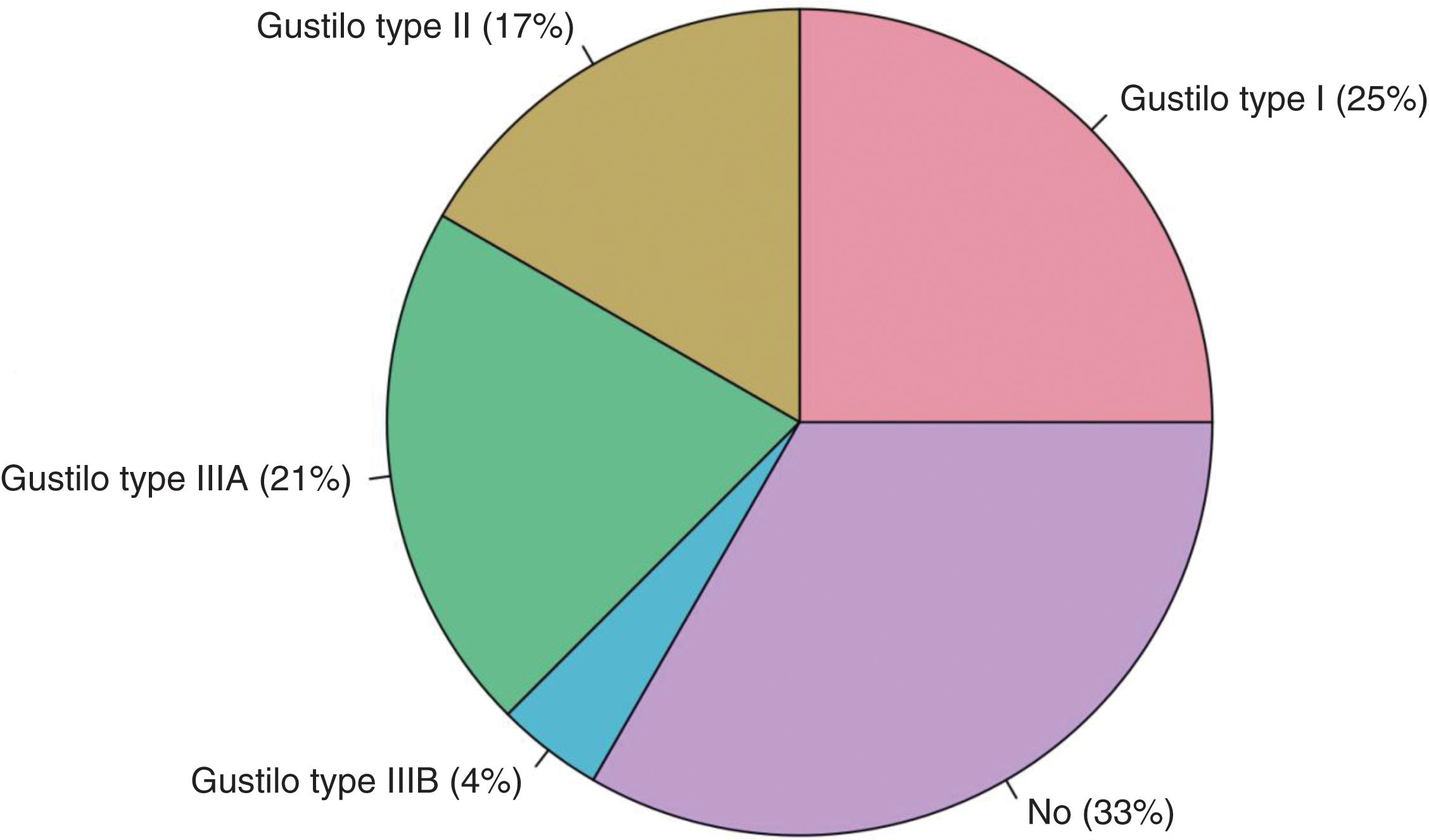
Eight patients had a closed fracture (33%), compared to 18 patients who had an open fracture (67%), with Gustilo type 1 in 6 patients (25%); Gustilo type 2 in 4 patients (17%); Gustilo type IIIA in 5 patients (21%) and Gustilo IIIB in one patient (4%) (Fig. 2). Ten patients also had associations with other organic injuries or fractures. Two patients died from causes unrelated to the trauma.
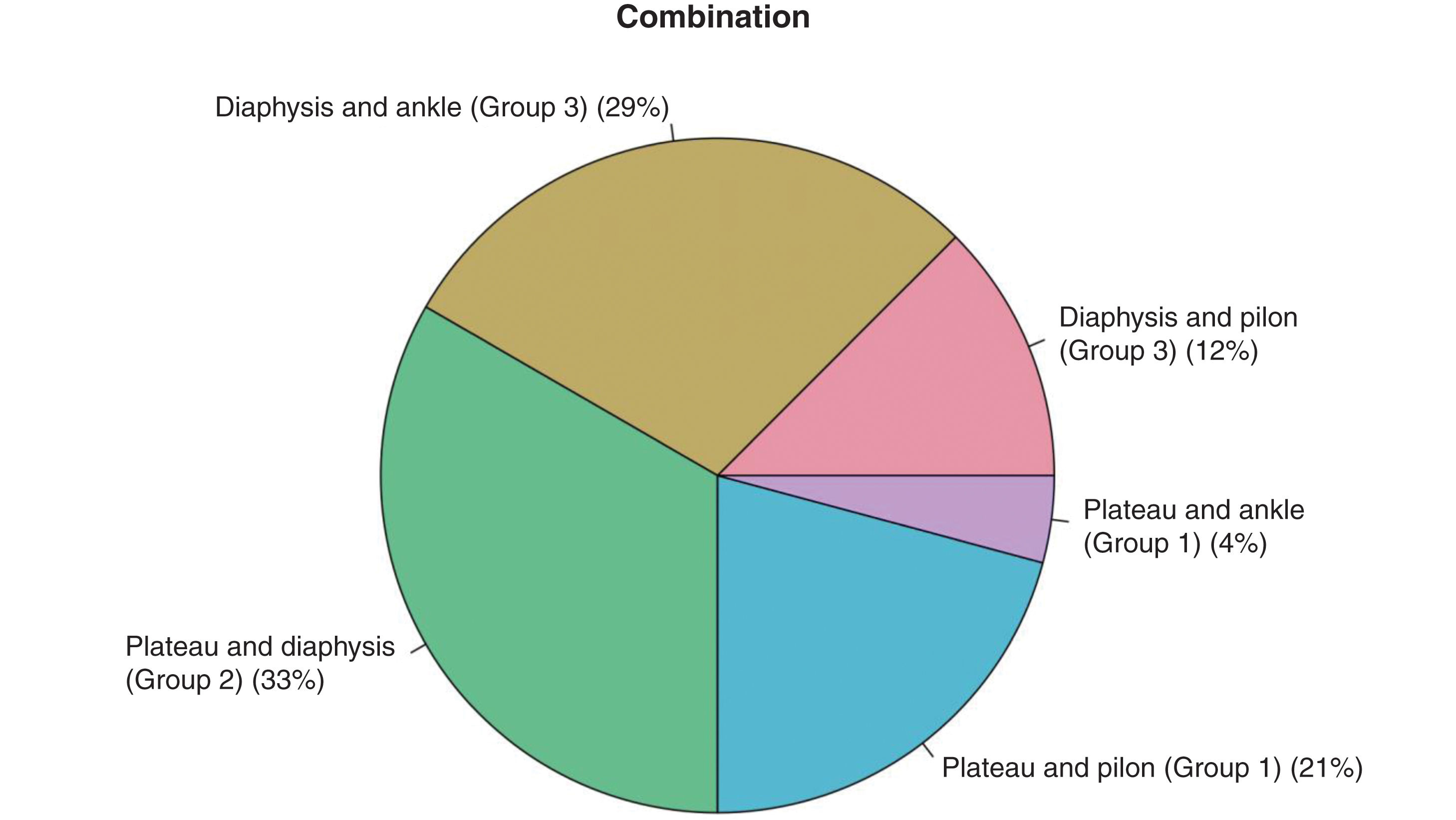
Regarding the type of bifocal fractures, 8 fractures (34%) were a combination of plateau and diaphysis, 5 patients (21%) a plateau with a pilon, 3 patients (12.5%) a diaphyseal fracture with a pilon, 7 patients (30%) a diaphyseal and ankle, and one patient (2.5%) a plateau and ankle. The number of implants required to reduce the fractures was one implant in 3 patients (12.5%) and 2 implants in 21 patients (87.5%). The fractures were studied and classified according to three large groups:
- -
Group 1: plateau fracture and distal tibia (ankle/pilon)
This group consisted of a combination of proximal and distal intra-articular fractures in 6 patients (25%) (Fig. 3), among which there are 5 patients with a plateau-pilon combination and one patient with a plateau-ankle combination. Two patients had a closed fracture, one patient a Gustilo and Anderson type 1 fracture, one patient a Gustilo and Anderson type II fracture, and two patients a Gustilo and Anderson type IIIA fracture. Three patients had a plateau fracture of type AO 41B1, two patients a AO 41C1 fracture, and one patient a AO41B3 fracture. Three patients had a distal pilon fracture of type AO 43A3, one patient a 43B1 fracture, and one patient a 43C2 fracture. Regarding the distal ankle fractures, the patient who presented this fracture had an AO 44A1 fracture of the ankle.
- -
Group 2: plateau and diaphyseal fracture
This group consisted of a combination of a tibial diaphyseal fracture with a tibial plateau fracture, and included 8 patients (33%). Five patients had a closed fracture, one Gustilo type I patient, one Gustilo type II patient, and one Gustilo type IIIB patient. Of plateau fractures, one patient had an AO 41B1 type, one patient an AO 41C3 type, one patient an AO 41C1 type, 2 patients an AO41A3 type and 3 patients an AO41A2 type. Of diaphyseal fractures, one patient had an AO 42C2 type fracture, 4 patients had AO 42A2 type, one patient a 42A3 type, one patient an AO42B2 type and one patient an AO42C3 type fracture.
- -
Group 3: Diaphyseal and distal tibia fracture (ankle/pilon)
This group consisted of the combination of diaphyseal and intra-articular distal fracture, which could either be a tibial pilon or an ankle, and included 10 patients (42%). Three patients had the diaphysis-pilon combination and 7 patients the combination of diaphysis and ankle. One patient had a closed fracture, 4 patients had a Gustilo type 1 fracture, 2 patients had a Gustilo type 2 fracture, and 3 patients had a Gustilo type 3A fracture. Regarding the type of diaphyseal fractures, 4 patients had an AO type 42A2, one patient had an AO type 42C2, one patient had an AO42B2, and 4 patients had an AOA3 type. Of the distal pilon fractures, one patient had a type 43B1 fracture, and 2 patients had an AO 43A1. Regarding the distal ankle fractures, 5 patients had an AO 44A1, one patient had an AO 44C1, and one patient had an AO44C3 (Table 1).
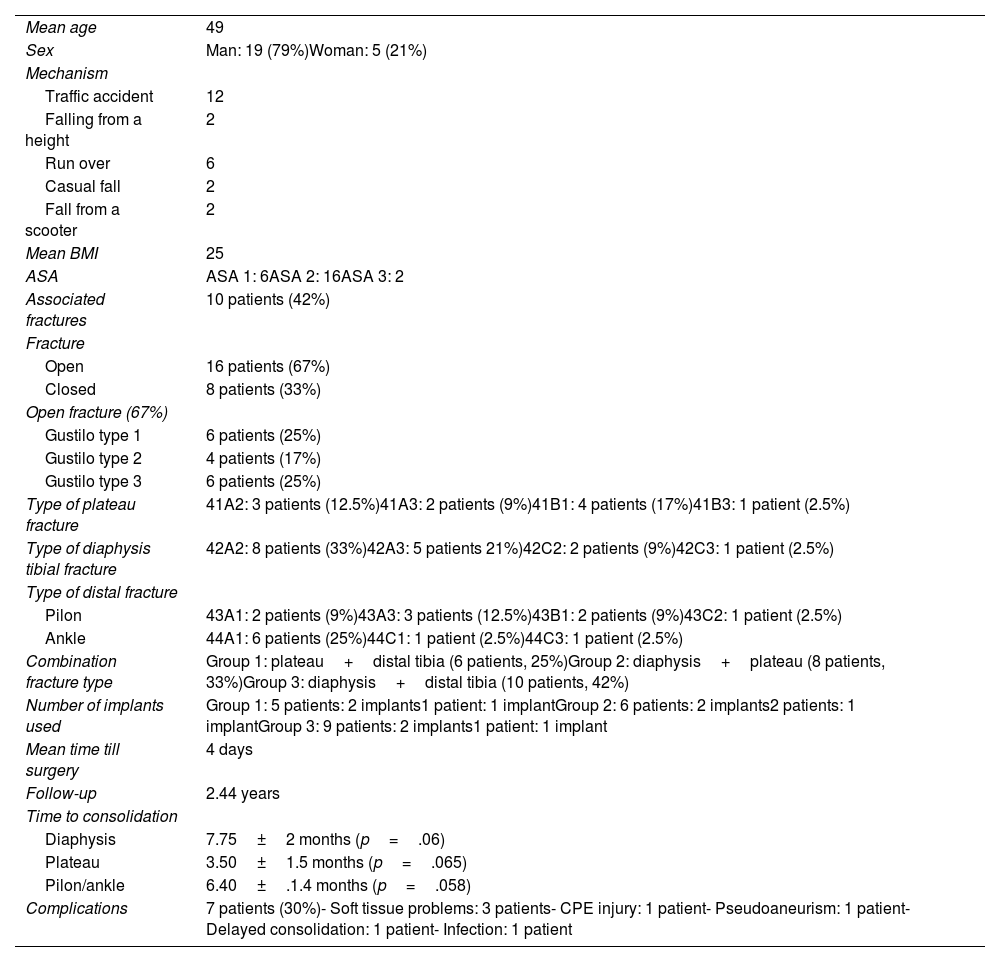
Summary of data included in our study.
| Mean age | 49 |
| Sex | Man: 19 (79%)Woman: 5 (21%) |
| Mechanism | |
| Traffic accident | 12 |
| Falling from a height | 2 |
| Run over | 6 |
| Casual fall | 2 |
| Fall from a scooter | 2 |
| Mean BMI | 25 |
| ASA | ASA 1: 6ASA 2: 16ASA 3: 2 |
| Associated fractures | 10 patients (42%) |
| Fracture | |
| Open | 16 patients (67%) |
| Closed | 8 patients (33%) |
| Open fracture (67%) | |
| Gustilo type 1 | 6 patients (25%) |
| Gustilo type 2 | 4 patients (17%) |
| Gustilo type 3 | 6 patients (25%) |
| Type of plateau fracture | 41A2: 3 patients (12.5%)41A3: 2 patients (9%)41B1: 4 patients (17%)41B3: 1 patient (2.5%) |
| Type of diaphysis tibial fracture | 42A2: 8 patients (33%)42A3: 5 patients 21%)42C2: 2 patients (9%)42C3: 1 patient (2.5%) |
| Type of distal fracture | |
| Pilon | 43A1: 2 patients (9%)43A3: 3 patients (12.5%)43B1: 2 patients (9%)43C2: 1 patient (2.5%) |
| Ankle | 44A1: 6 patients (25%)44C1: 1 patient (2.5%)44C3: 1 patient (2.5%) |
| Combination fracture type | Group 1: plateau+distal tibia (6 patients, 25%)Group 2: diaphysis+plateau (8 patients, 33%)Group 3: diaphysis+distal tibia (10 patients, 42%) |
| Number of implants used | Group 1: 5 patients: 2 implants1 patient: 1 implantGroup 2: 6 patients: 2 implants2 patients: 1 implantGroup 3: 9 patients: 2 implants1 patient: 1 implant |
| Mean time till surgery | 4 days |
| Follow-up | 2.44 years |
| Time to consolidation | |
| Diaphysis | 7.75±2 months (p=.06) |
| Plateau | 3.50±1.5 months (p=.065) |
| Pilon/ankle | 6.40±.1.4 months (p=.058) |
| Complications | 7 patients (30%)- Soft tissue problems: 3 patients- CPE injury: 1 patient- Pseudoaneurism: 1 patient- Delayed consolidation: 1 patient- Infection: 1 patient |
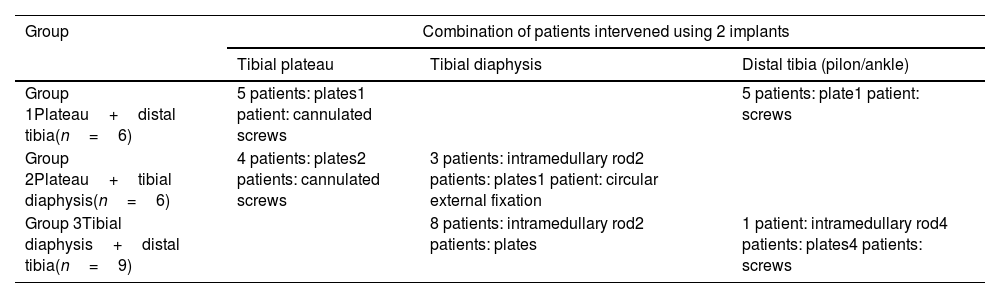
Group 1 (n=6. 25%): Five patients underwent surgery on the plateau using plates, and one patient was treated with cannulated screws. At the distal level, of the 5 patients with a pilon, 4 were treated with a plate and one with screws, specifically, the patient with the association of plateau and ankle (Fig. 4).
Group 2 (n=8. 33%): Two patients underwent surgery for both fractures using a single implant; an intramedullary nail. The remaining 6 patients underwent surgery using a combination of different implants. Four patients were treated at the level of the tibial plateau with plates and 2 patients with cannulated screws. At the level of the diaphysis, 3 patients were treated with an intramedullary rod, 3 patients with plates and one patient with a circular external fixator (Fig. 5).
Group 3 (n=10. 42%): Nine patients underwent surgery for both fractures using 2 implants and one patient underwent surgery using one implant. Eight patients underwent surgery using a T2 intramedullary rod at the diaphysis level and 2 patients underwent surgery using plates. At the distal level for the pilon (3 patients), one patient underwent surgery using a T2 and 2 patients underwent surgery using plates. At the ankle level (7 patients), 4 patients underwent surgery using cannulated screws, 2 patients underwent surgery using plates and one patient had conservative treatment (Table 2 and Fig. 6).
Combination of patients intervened using 2 implants.
| Group | Combination of patients intervened using 2 implants | ||
|---|---|---|---|
| Tibial plateau | Tibial diaphysis | Distal tibia (pilon/ankle) | |
| Group 1Plateau+distal tibia(n=6) | 5 patients: plates1 patient: cannulated screws | 5 patients: plate1 patient: screws | |
| Group 2Plateau+tibial diaphysis(n=6) | 4 patients: plates2 patients: cannulated screws | 3 patients: intramedullary rod2 patients: plates1 patient: circular external fixation | |
| Group 3Tibial diaphysis+distal tibia(n=9) | 8 patients: intramedullary rod2 patients: plates | 1 patient: intramedullary rod4 patients: plates4 patients: screws | |
The average follow-up time in outpatient clinics was two and a half years. A total of 22 patients (92%) were fully weight bearing at one year and 2 patients were partially weight bearing (8%). The mean consolidation time of the diaphysis was 7.75±2 months, with no significant differences between Group 2 and Group 3 (p=0.06). The mean consolidation time of the metaphysis was 3.50±1.5 months, with no significant differences between Group 1 and Group 2 (p=.065). The mean consolidation time of the pilon/ankle was 6.40±1.4 months, with no significant differences between Groups 1 and 3 (p=.058).
Regarding knee mobility, 5 patients (21%) had decreased range of flexion–extension, of which 3 patients were from Group 3, 2 patients were from Group 2 and one patient from Group 1. Regarding ankle mobility, 8 patients (34%) had full ankle mobility sequelae, of whom 3 patients were from Group 1, one patient from Group 2 and 4 patients were from Group 3.
Regarding complications, 7 patients (30%) had complications during follow-up: one patient had a pseudoaneurysm of the popliteal trunk, one patient had paralysis of the EPSN, 2 patients required a flap for posterior coverage, one patient had a skin graft, one patient had an infection from the osteosynthesis material and one patient had delayed consolidation that ended up consolidating.
There were two deaths which were unrelated to the fractures.
DiscussionBifocal tibial fractures are rare, but they pose a therapeutic challenge for the surgeon due to the increased complexity of their treatment. Due to their low frequency, there is no consensus as to the ideal treatment for them. Usually, when these types of fractures occur, they are associated with young patients and high-energy mechanisms. Our study shows that, despite their low frequency, they are more frequent in normal practice than expected, accounting for up to 5% of all tibial fractures. There is usually a high rate of open fractures, up to 54.2% of the total according to the literature.3,5,11 These data are lower than those found in our study, where open fractures accounted for 67% of all the fractures.
Few studies address this combination of fractures. Keating et al.3 classified fractures into three large groups, depending on the combinations to which they were associated. In our case, the most frequent combination was Group number 3, corresponding to the combination of a diaphyseal tibial fracture together with a distal fracture (42%), either of the ankle or the tibial pilon, also corresponding to what Keating et al. observed in their study.
Optimal stabilisation of these fractures is essential and requires meticulous surgical planning, especially if the use of nailing is combined with plates at the proximal or distal level. In most cases, fracture reduction is started at the joint level to reduce the fragments and stabilise it, giving priority to an anatomical reduction.12,13 In our case, we first performed provisional fixation of the joint fracture, with definitive fixation of the diaphyseal segment and subsequently definitive fixation of the joint segment, often modifying the unicortical screws for bicortical ones at the plateau level. In some studies, such as that of Vendeuvre and Gayet,14 a percutaneous reduction for the plateau is proposed in order to try to maintain periosteal vascularisation and reduce the infection rate. This has also been observed in other studies, in which Schatzker type I, II and III fractures have good results with percutaneous reduction.15,16 In our case, 2 patients were able to undergo surgery using percutaneous screws. However, the complexity of the fractures required the use of plates or even a rod.
In some patients, the fracture reduction was possible using the same implant, this being the case in those patients who had a metaphyseal fracture without joint involvement, or in which the plates could also be used to resolve the diaphyseal fragment. It must be taken into account that the resolution of a bifocal focus with an implant requires that it can be performed following the fracture pattern and with a high level of demand from the surgeon for an optimal fracture reduction. There are studies showing that the use of rods in Schatzker type V and VI fractures, together with fixation with cannulated screws can be used with satisfactory long-term functional results,17–20 thanks to the role of ligamentotaxis in realigning the limb in the axis and reducing the fragments.
One of the advantages of the intramedullary rod is that through a suprapatellar or infrapatellar incision, far from the fracture site, in many cases relative stability can be obtained without having to access the fracture site and respecting soft tissues.21–23 It must be taken into account that a poor state of the soft tissues often determines the time and the decision of the type of implant to be chosen. Respecting the state of the soft tissues is essential, since it reduces the rate of complications, such as infection of the osteosynthesis material, or the need for plastic surgery.24
Regarding the consolidation rate, in our study the mean was 7.75±2 months for the diaphyseal area and 3.50±1.5 months for the plateau. These data are quite similar to those found in the literature, in which the mean consolidation rate varies between 3 and 4 months for the plateau21,25,26 and 8 months for the tibial diaphysis.21,26,27 We did not find any significant differences in the consolidation of the metaphyseal or diaphyseal fracture, regardless of the type of group to which the fracture belonged.
A limitation of this study is that it was a retrospective review of the patients and there was no control group in which to make an adequate comparison. Although the inclusion and exclusion criteria were carefully chosen, some fracture heterogeneity existed. It should be noted that the pattern of this type of fracture, excluding bifocal tibial diaphyseal fractures, is rare and therefore it is difficult to obtain a larger sample.
ConclusionsBifocal tibial fractures are rare fractures that sometimes require the combination of several types of osteosynthesis to obtain adequate reduction. In our series, the most frequent fractures were type 3 (fracture of the diaphysis and distal tibia). When the tibial diaphysis was involved, combined osteosynthesis was required using an intramedullary rod together with plates and screws, obtaining consolidation rates, long-term functional results and complications similar to those described in the literature.
Level of evidenceLevel of evidence IV.
Ethical considerationsNone declared.
FundingNone declared.
Conflict of interestsNone declared.