Brown tumours are highly vascular lytic bone lesions found in primary and secondary hyperparathyroidism. The brown term is given due to the red-brown colour of the tissue, which is due to the accumulation of haemosiderin. The case is presented of a 29 year-old male with chronic renal failure, who had a mass in the tip of the ring finger after a trauma of 4 months onset, which had increased progressively in size and pain. He was treated surgically, by amputation, with no recurrence 10 months after the surgery.
Los tumores pardos son lesiones óseas líticas altamente vasculares encontradas en el hiperparatiroidismo primario y secundario. El término pardo se le da por el color rojo-marrón de los tejidos, dado por la acumulación de hemosiderina. En el siguiente caso clínico, presentamos a un paciente masculino de 29 años de edad, con insuficiencia renal crónica terminal, quien cursa con 4 meses de aparición de masa en punta del dedo anular derecho posterior a un trauma, que ha aumentado en tamaño y dolor de forma progresiva. Fue tratado de forma quirúrgica, mediante amputación, preservando márgenes sanos y, luego de 10 meses de la cirugía, no ha presentado recidiva.
Brown tumours (BT) are highly vascular lytic bone lesions found in primary and secondary hyperparathyroidism. Inside the tumour there is abundant fibrovascular tissue and giant cells similar to osteoclasts. The brown term is given due to the red-brown colour of the tissue, which is due to the accumulation of haemosiderin.1
Traditionally and historically, BT have been reported in patients of all ages, especially those with primary hyperparathyroidism. However, since this entity now being diagnosed in the early stages BT is less frequent in these patients. It is more common, and found in up to 13%, in patients with secondary hyperthyroidism.1,2
Hormonal and biochemical changes occur in chronic renal failure (CRF) that give rise to calcifications in the organism and changes in the osseous skeleton. This disease is known as renal osteodystrophy. Secondary hyperparathyroidism is a consequence of these changes and is found in most patients who require haemodialysis.
The pathophysiology of secondary hypoparathyoidism is reduced excretion of phosphorous due to renal failure, which generates a reduction in the active form of vitamin D (calcitriol) and serum calcium levels. In addition to hyperphosphataemia and hypocalcaemia, CRF causes decreased activity of 1-alpha-hydroxilase, which reduces intestinal absorption of calcium. Hypocalcaemia, therefore, causes an increase in parathormone secretion and in bone resorption. Some patients can present severe secondary hyperparathyroidism, with the consequent appearance of lytic bone lesions known as BT.3–6
BT can compromise the axial or appendicular skeleton. On X-ray they show up as cystic images since they generally do not compromise the cortical layers, however, they can resemble single or multiple lytic lesions as well. Generally when the lesions are small, in the initial stages, treating the hyperparathyroidism can cause involution of the tumour.
Presentation of a caseWe present the case of a 29-year-old male patient with a history of right nephrectomy, diagnosed with end-stage kidney disease, treated with haemodialysis 3 days a week, and presenting with clinical symptoms of 4 months’ onset that comprised the appearance of a mass at the tip of the right ring finger after trauma. The patient reported that the mass had been gradually increasing in size and pain and therefore he was admitted to our institution via the emergency department.
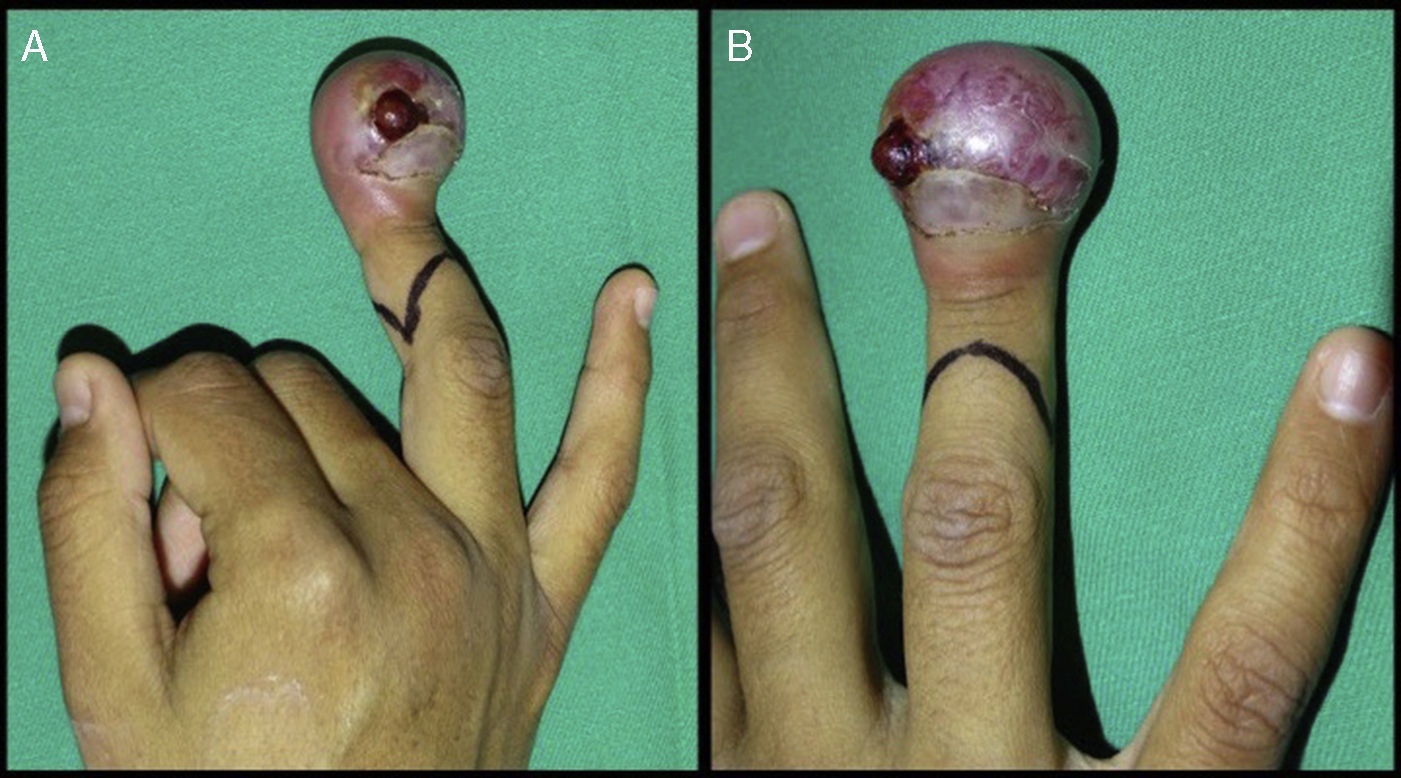
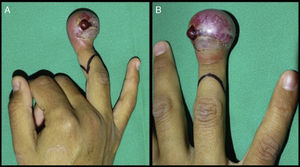
After a thorough physical examination, we found that the mass in the right ring finger measured approximately 3cm×3cm and was compromising the circumference of the finger tip deforming the nail plate (Fig. 1A and B).
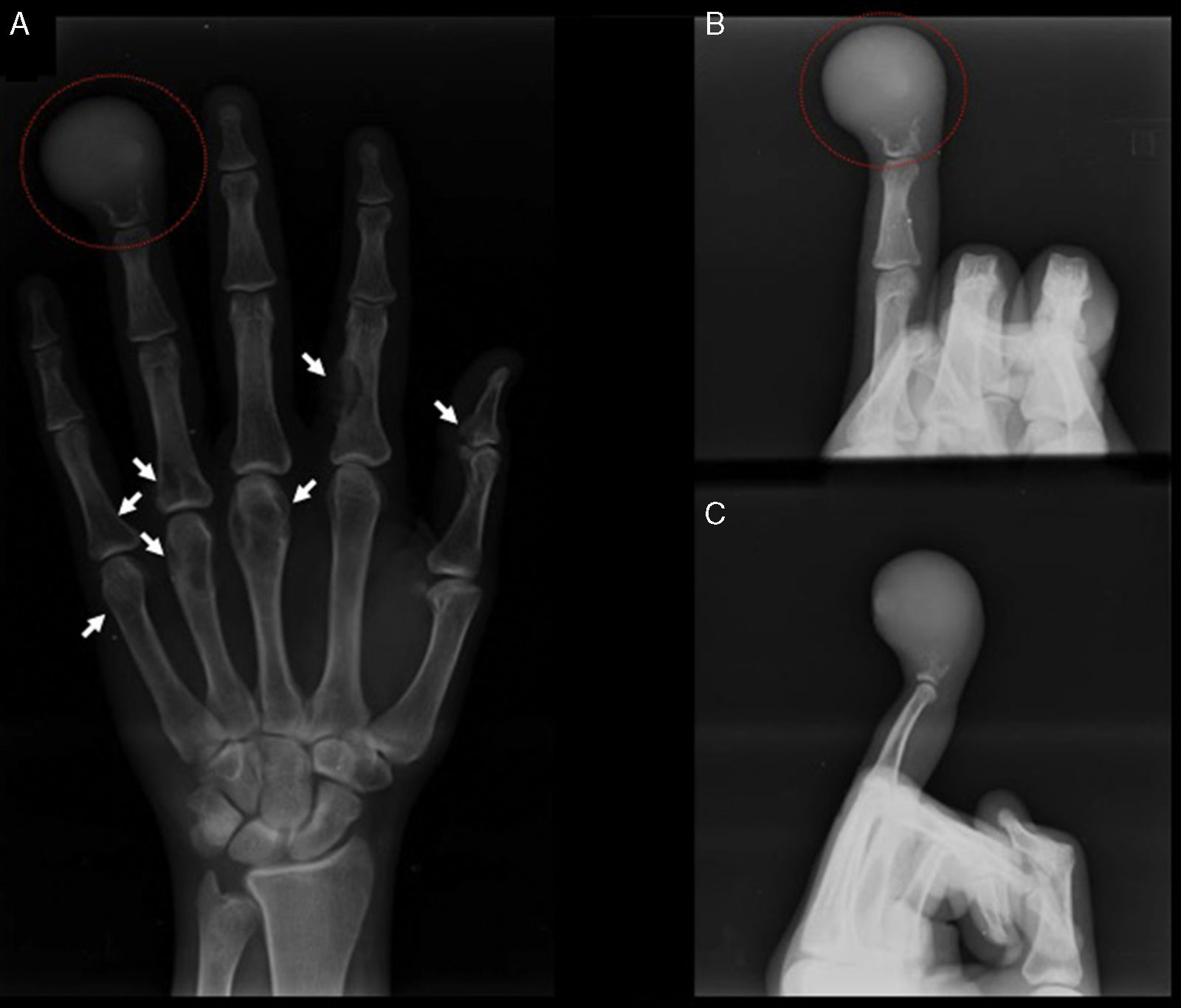
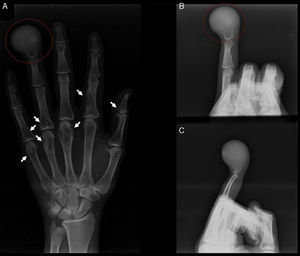
X-rays were then taken, which showed a lytic lesion almost completely compromising the distal phalanx of the ring ringer, partially respecting the joint surface of the distal interphalangeal joint and a small amount of the proximal part of the phalanx. Other less striking associated lesions were also observed in the phalanges and metacarpals (Fig. 2).
(A) The lytic image of the distal phalange of the right ring finger is shown in the red circle on an AP view. The white arrows indicate the other lesions in the phalanges and metacarpals. (B and C) Narrow oblique and lateral X-rays respectively of the right ring finger. The lytic image of the distal phalange of the right ring finger is shown in the red circle.
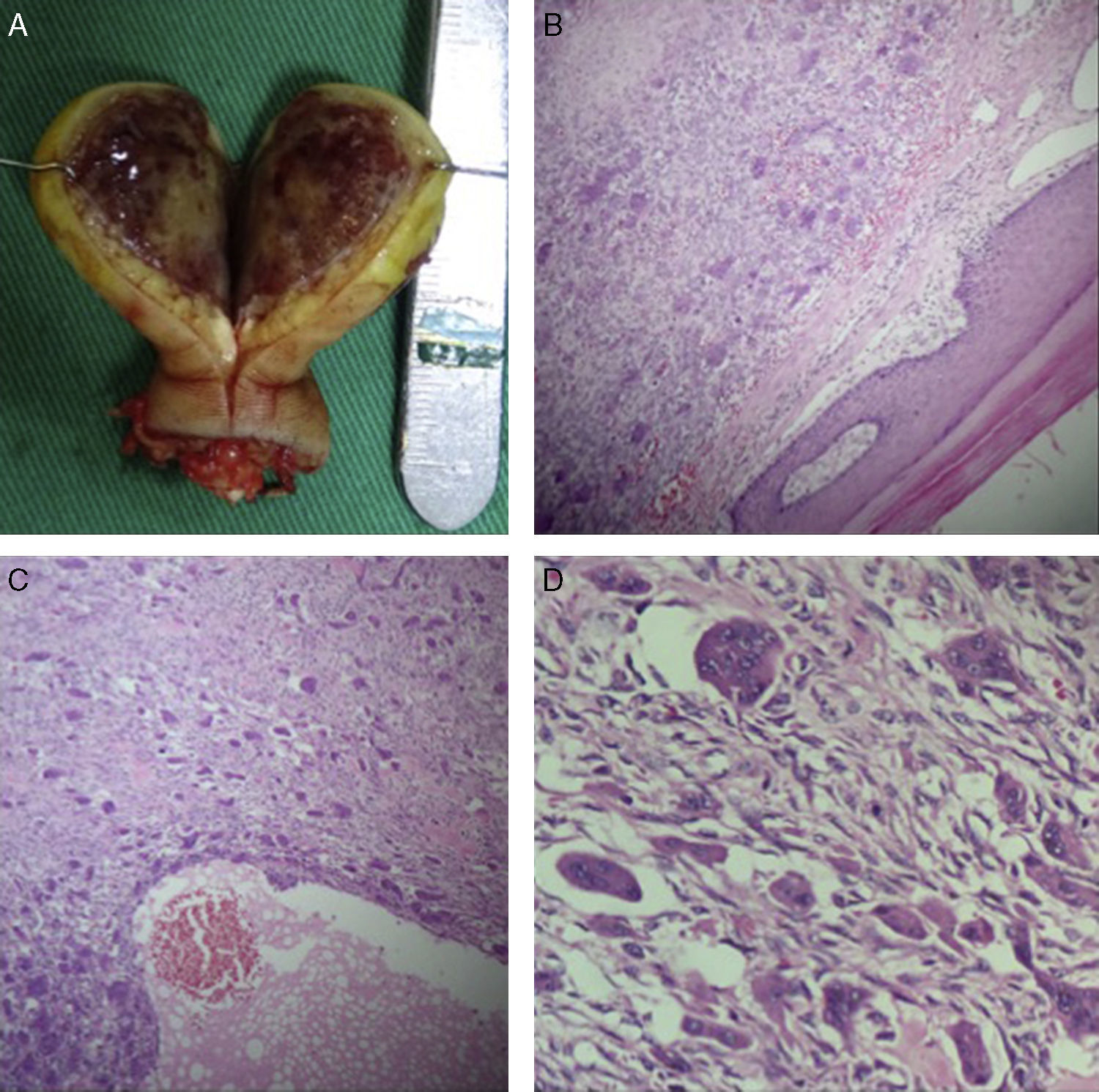
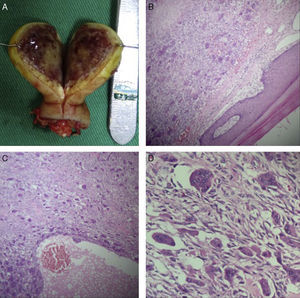
After assessing the patient clinically and radiographically, it was concluded that he presented a BT in the distal phalanx of the ring finger, for which the tip of the finger was amputated, preserving the healthy margins. Macroscopically, a mass of 2.5cm×3cm was confirmed, in which it was not possible to identify the distal phalanx (Fig. 3A). Histologically, our institution's Department of Pathology described a well-defined lesion, comprising fibroblast-rich stroma with red blood cell extravasation and abundant multinucleated giant cells arranged in lobules separated by reactive bone tissue, with cystic areas with haematic content, which confirmed the diagnosis (Fig. 3B–D).
(A) The content of the BT can be seen clinically, with absence of the distal phalange of the right ring finger. The typical colour of the tumour due to the accumulation of haemosiderin can also be seen. (B) Well-defined lesion surrounded by acral skin; stain: haematoxylin and eosin; 4×. (C) Lesion comprising fibroblast-rich stroma with red blood cell extravasion; stain: haematoxylin and eosin; 20×. (D) Multinucleated giant cells arranged in lobules; stain: haematoxylin and eosin; 40×.
The patient is undergoing treatment for CRF and secondary hyperparathyroidism in the nephrology and endocrinology departments and has not suffered a recurrence or further tumours to date.
DiscussionBrown tumours, also known as osteoclastomas, are the most common bone tumours in secondary hyperparathyroidism. Despite presenting as invasive lesions, they do not have the potential to turn malignant. They present most frequently in the jaw, sternum, pelvis, ribs and femur.2 They very rarely present in the hand and this is seldom reported.
We have various possible diagnoses when faced with a bone tumour with lytic characteristics. These include: giant cell tumour (GCT), aneurysmal bone cyst, chondroblastoma, nonossifying fibroma, simple bone cyst, osteosarcoma, BT due to hyperparathyroidism, enchondroma, metastases, chondrosarcoma and even giant cell granuloma.
Both GCT and BT derive from osteoclast precursor cells, with histological and radiological similarities. However, the latter is a primary tumour and BT is a consequence of hyperparathyroidism.5
Reichet et al.5 present the case of a 38-year-old woman, with an osteolytic tumour of the distal epiphysis of the fifth metacarpal, which was initially treated by curettage of the tumour and corticocancellous graft as it had been diagnosed a GCT. Because the tumour recurred, the tumour was controlled and the metacarpal remodelled with a subtotal parathyroidectomy, with no recurrence at the time of publication of the article. Similarly, Kao et al.7 report the case of a 32-year-old patient, with multiple osteolytic lesions in the tibia and left fibula and the fourth metacarpal of the left hand associated with reduced bone mineral density. It was mistakenly diagnosed as a multiple GCT. However, with further biochemical and diagnostic imaging tests they concluded that this was a BT due to primary hyperparathyroidism. After left parathyroidectomy the bone mineral density improved and the BT.
Franco et al. present a 46-year-old female patient, with a BT due to secondary hyperparathyroidism, which on X-rays presented an improvement 2.5 years after parathyroidectomy.8
Ertuk et al.6 present an atypical case of a 28-year-old woman, with a BT of the fourth metacarpal as a consequence of hyperparthyroidism secondary to dietary deficiency of vitamin D and poor exposure to sunlight. It was initially treated with curettage and biopsy, which confirmed the diagnosis histopathologically, and was later treated with vitamin D and calcium replacement, resulting in resolution of the tumour and bone remodelling.
The reports we outline show us that that there is a higher incidence of BT in young people. However, it is very seldom found in the hand, and even more rarely found in the fingers. Although the indication is to treat the underlying disease, in this case, secondary hypothyroidism, given the extensive soft tissue, nail plate and bone tissue compromise, we decided to treat the 29-year-old patient with end-stage kidney disease radically, aiming for the most rapid resolution for him. The report by Franco et al.8 indicates that it took 2.5 years to achieve an appropriate result after parathyroidectomy. We considered this a long time for a terminal patient. By amputating we managed to improve the patient's quality of life considerably and, above all, eliminate his pain.
At present the patient is alive, his underlying diseases are being treated by the nephrology and endocrinology services, and 10 months after the amputation, he has experienced no recurrence or growth in the size of his other lesions.
We consider this a very interesting case, since there are few reported cases of BT in the hand. It is the first to consider the chronic nature of the patient's underlying disease and condition in order to manage the tumour.
Level of evidenceLevel of evidence IV.
Ethical disclosuresProtection of humans and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their centre of work regarding the publication of patient data
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflicts of interests to declare.
Please cite this article as: Forigua V JE, Brunicardi H RA, Morales V CA, Archila MP, Chaparro Rivera DM. Tumor pardo en falange del dedo anular por insuficiencia renal crónica. Reporte de un caso. Rev Esp Cir Ortop Traumatol. 2017;61:349–353.