Chronic recurrent osteomyelitis (CRO) is a rare disease characterised by unifocal or multifocal aseptic inflammatory bony lesions.
ObjectiveTo evaluate clinical features and response to treatment with non-steroidal anti-inflammatory drugs in patients with CRO.
Materials and methodsA retrospective assessment was conducted on 5 children with OCR over a period of 8 years. They had been diagnosed based on clinical, laboratory findings, histological study of injuries, and imaging test.
ResultsMultifocal disease was observed in 40% of cases, and unifocal in 60%. The large majority (80%) were male, with a mean age at diagnosis of 13 years (range: 11–15 years). The bones most frequently affected were the clavicle and tibia, representing 18.2%. The most common presenting symptom was pain in all patients, with fever being present in 20% of cases. Imaging studies such as CT and MRI were effective in 100%, and in all cases the biopsy reported a lymphoplasmacytic infiltrate. After a mean follow-up of 5.9 years, there was a good treatment response in 100%, with a mean recurrence at 5.25 months being observed.
ConclusionsThe anodyne results of most clinical studies to assess CRO, and the similarity in clinical presentation of this with many infectious or tumour diseases makes its diagnosis a real challenge. On the other hand treatment with NSAIDs can be considered a good initial therapeutic option.
La osteomielitis crónica recurrente (OCR) es una rara enfermedad caracterizada por lesiones óseas inflamatorias asépticas uni- o multifocales.
ObjetivoValorar características clínicas y la respuesta al tratamiento con AINE de los pacientes con OCR.
Materiales y métodosCinco niños con OCR valorados de forma retrospectiva por un periodo de 8 años, los cuales fueron diagnosticados basándose en los hallazgos clínicos, analíticos, estudio anatomopatológico de las lesiones y pruebas de imagen.
ResultadosEl 40% presentó afectación multifocal y el 60% unifocal. El 80% eran del sexo masculino (4/5), la edad media al momento del diagnóstico 13 años (r: 11-15 años), los huesos más frecuentemente afectados fueron la clavícula y la tibia representado el 18,2%, el síntoma más común fue el dolor presentándose en todos los pacientes, la fiebre apareció en el 20% de los casos. Los estudios de imagen como la TAC y la RM fueron eficaces en el 100% y en todos la biopsia objetivó infiltrado linfoplasmocitario. Después de un seguimiento medio de 5,9 años se observó una buena respuesta al tratamiento en el 100%, con una recurrencia media a los 5,25 meses.
ConclusionesLos resultados anodinos de la mayoría de los estudios clínicos para valorar OCR y la similitud en la presentación clínica de esta con muchas patologías infecciosas o tumorales hace que su diagnóstico represente un verdadero reto, por otra parte el tratamiento con AINE puede considerarse una buena opción terapéutica inicial.
Chronic recurrent osteomyelitis (CRO) is a rare clinical entity characterised by the presence of aseptic inflammatory foci in one (chronic recurrent unifocal osteomyelitis) or several bones (chronic recurrent multifocal osteomyelitis) which principally affects the long bone metaphysis and is considered the most severe form of non-bacterial bone inflammation in infancy and adolescence.
Although this disease has been known for more than 40 years, its pathogenesis has not been at all clarified. Currently the most accepted hypothesis is that it is a hereditary dysfunction of the immune system.
Diagnosis poses a real challenge because imaging techniques show non-specific lesions which suggest multiple diagnostic possibilities and furthermore, most analytical tests (acute phase reactants, serology and microbiological cultures) return negative.
The aim of the study is to present a case series of patients with chronic recurrent osteomyelitis, both unifocal and multifocal, treated in our unit to assess their clinical features and response to treatment with NSAIDs, and also present a review of the current references.
Patients and methodsBetween the years 2007 and 2015, 5 patients were diagnosed and treated in our hospital for non-bacterial osteomyelitis, reviewed retrospectively and classified into 2 groups. The first group comprised patients diagnosed with chronic recurrent unifocal osteomyelitis (CRUO) and the second comprised patients with chronic recurrent multifocal osteomyelitis (CRMO), there were 4 male patients and one female patient, aged between 11 and 15 years.
The patients had been referred to our centre with high initial clinical suspicion of neoplastic disease with bone involvement. The diagnosis of CRO was made after excluding other diseases such as infectious osteomyelitis, hypophosphatasia, histiocytosis, leukaemia, lymphoma, osteosarcoma, etc.
All the patients were assessed by means of laboratory tests: blood count, acute phase reactants, rheumatoid factor, hepatitis A and B serology, Salmonella typhi, Brucella, cytomegalovirus, HIV, Epstein–Barr virus, rubeola, Toxoplasma gondii, Treponema pallidum, Mycoplasma pneumoniae, Legionella, Chlamydia pneumoniae, Borrellia, varicella zoster.
The imaging tests performed were: plain X-rays, computerised axial tomography (CAT), magnetic nuclear resonance (MRI), bone gammagraphy and positron emission tomography (PET-CT) to assess the lesions causing these patients’ symptoms. Bone biopsies were also taken for anatomopathological and microbiological study.
Once diagnosis had been confirmed, the patients were treated with NSAIDs (naproxen and ibuprofen), the patients were followed -up for a mean of 5.9 years during which time the response to treatment and rate of recurrence were monitored. Both clinical and radiographic improvement represented by a diminution or disappearance of pain and improved bone lesions was considered a favourable response.
The Mann–Whitney U test was used for the statistical analysis to assess the clinical differences between the patients with CRMO and those with CRUO.
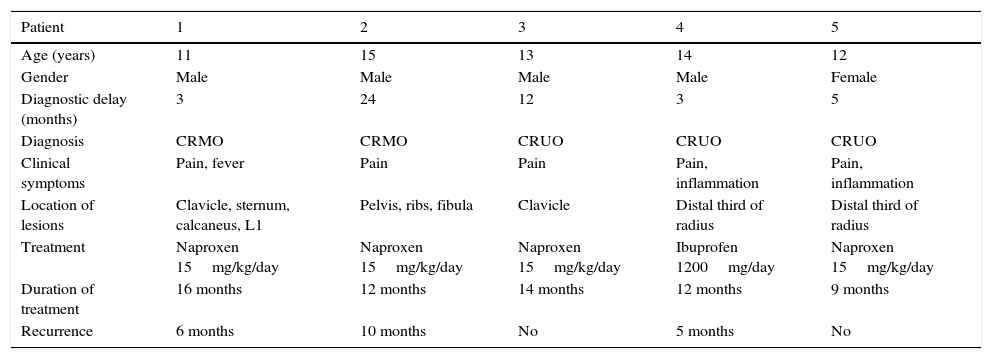
ResultsFour of the 5 patients in the series were male and there was one female, 3 of the patients had been diagnosed with CRUO and 2 with CRMO, the mean age of the onset of symptoms was 12 (r: 10–13 years) with a mean diagnostic delay of 9.4 months (r: 2–24 month), and a mean age at time of diagnosis of 13 years (r: 11–15 years). A total of 11 bones were affected with a mean of 2 bones per patient (r: 1–4 bones); the most frequently affected bones were the clavicle and the tibia in 2 cases (18.2%), followed by the distal radius, fibula, sternum, calcaneus, the lumbar vertebrae (L1), and pelvis; the ribs were affected on one occasion (Table 1).
Clinical characteristics of patients with CRO.
| Patient | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| Age (years) | 11 | 15 | 13 | 14 | 12 |
| Gender | Male | Male | Male | Male | Female |
| Diagnostic delay (months) | 3 | 24 | 12 | 3 | 5 |
| Diagnosis | CRMO | CRMO | CRUO | CRUO | CRUO |
| Clinical symptoms | Pain, fever | Pain | Pain | Pain, inflammation | Pain, inflammation |
| Location of lesions | Clavicle, sternum, calcaneus, L1 | Pelvis, ribs, fibula | Clavicle | Distal third of radius | Distal third of radius |
| Treatment | Naproxen 15mg/kg/day | Naproxen 15mg/kg/day | Naproxen 15mg/kg/day | Ibuprofen 1200mg/day | Naproxen 15mg/kg/day |
| Duration of treatment | 16 months | 12 months | 14 months | 12 months | 9 months |
| Recurrence | 6 months | 10 months | No | 5 months | No |
The most common symptom in the 5 patients in terms of clinical presentation was local pain which presented in all cases. Arthritis was also present in one patient adjacent to the affected bone observed with a lesion in the proximal tibia and ipsilateral knee inflammation, and also one patient presented fever (Table 1).
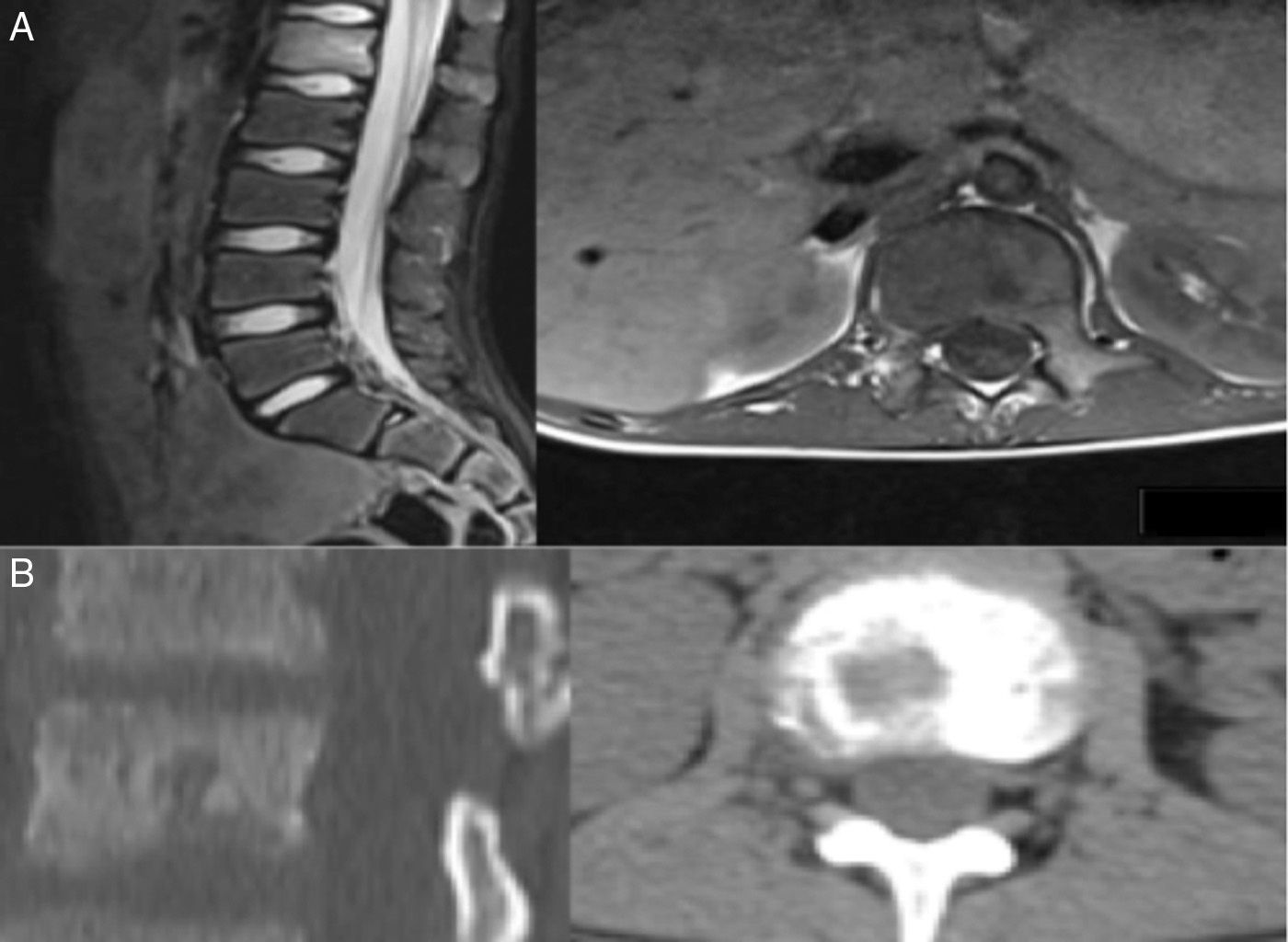
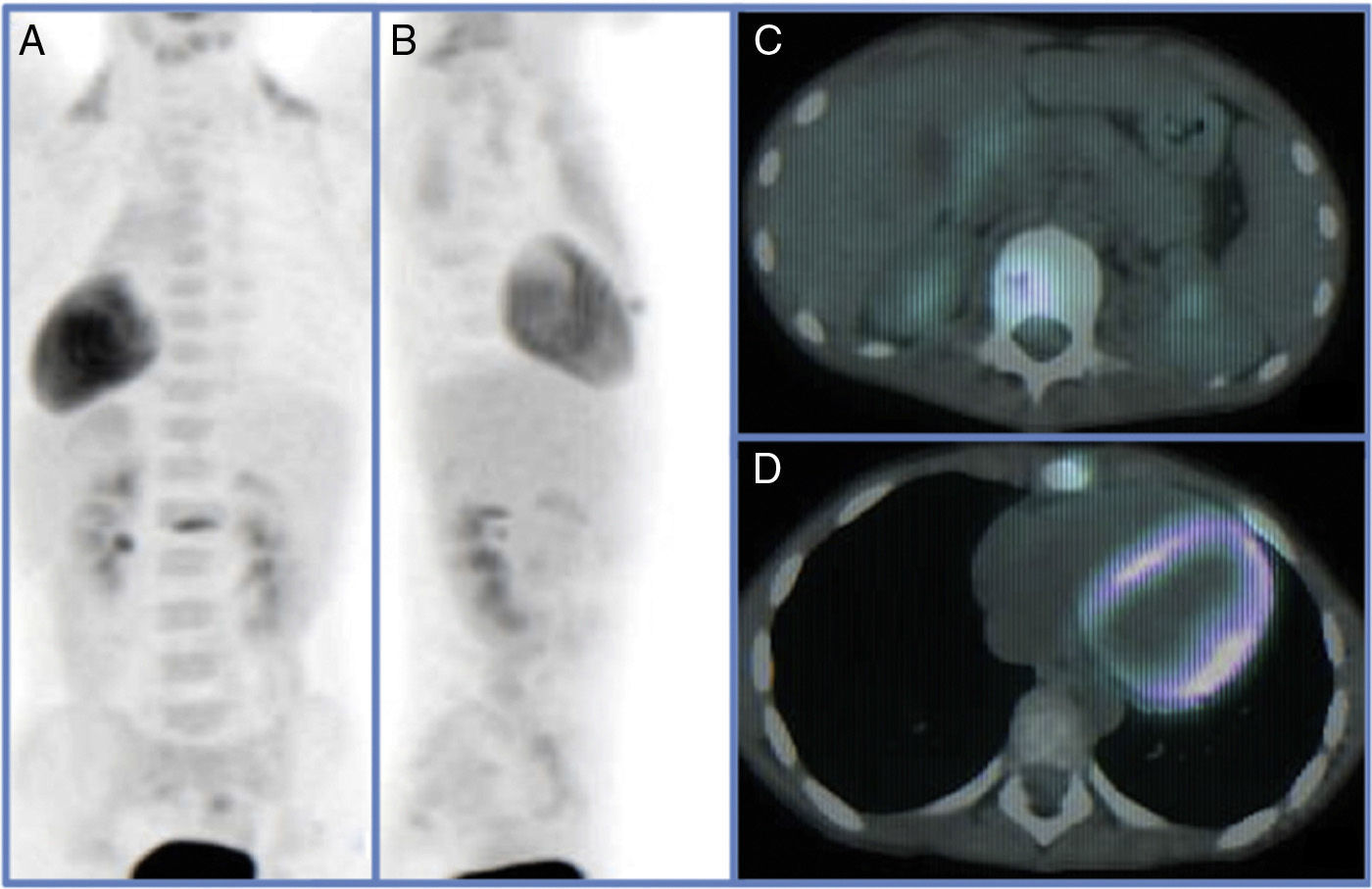
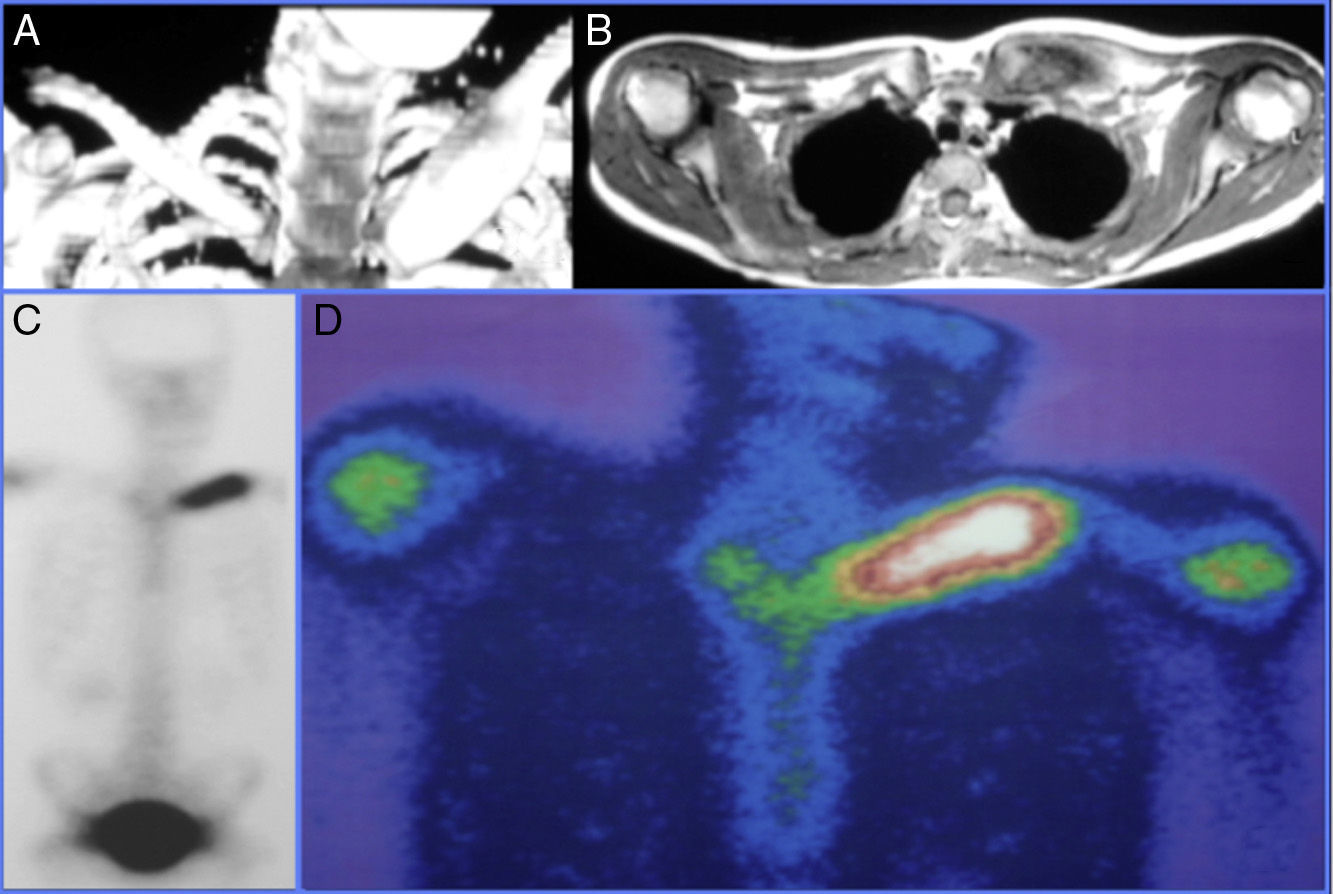
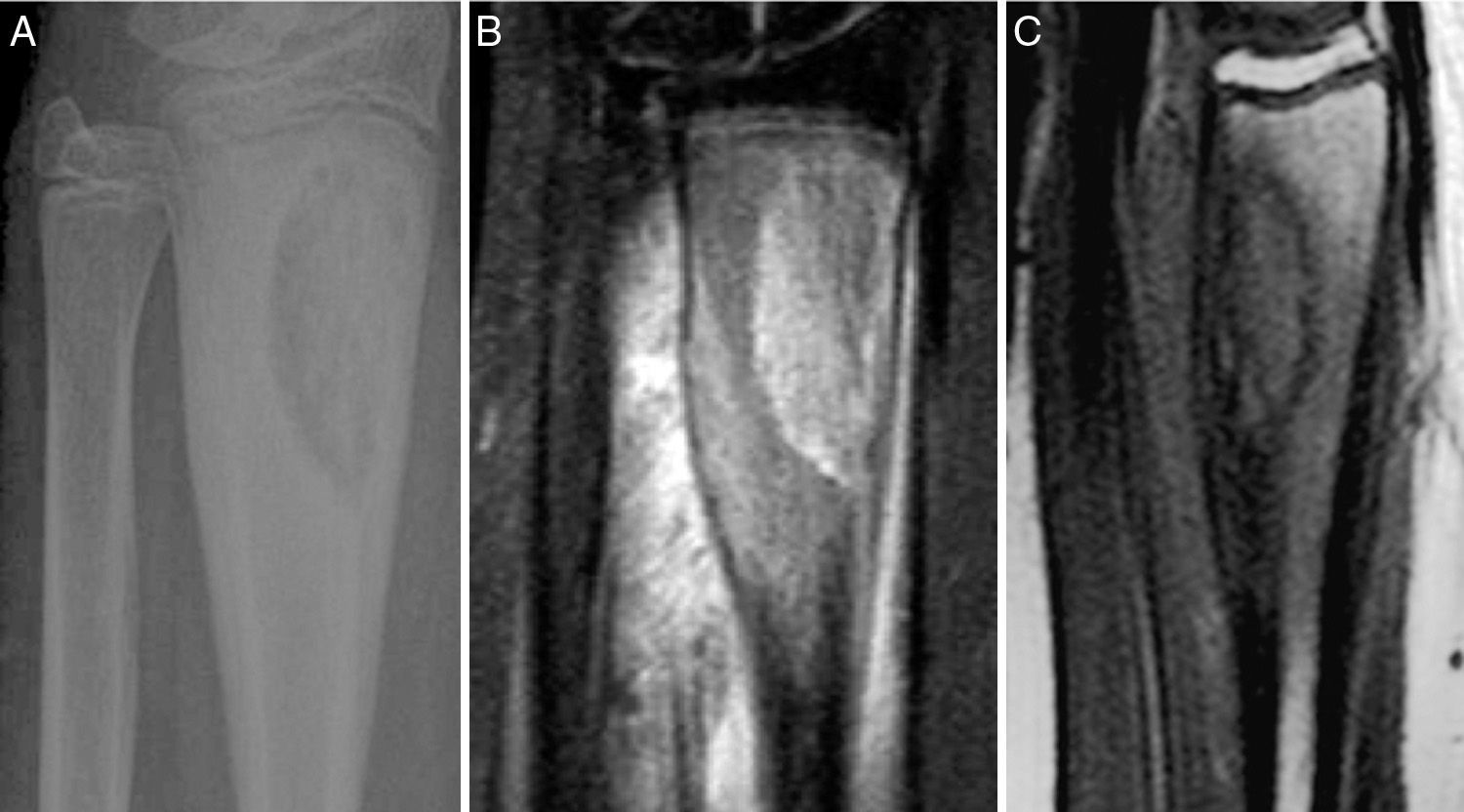
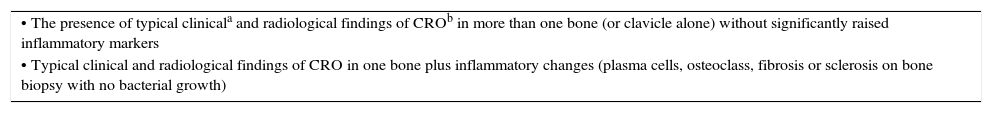
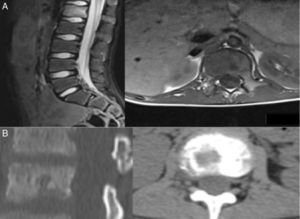
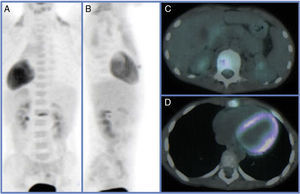
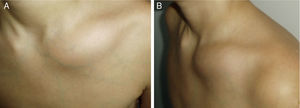
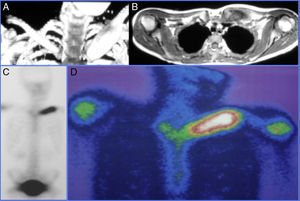
Various imaging tests were used for diagnosis including plain X-ray, CAT and MRI which showed lytic bone lesions with areas of sclerosis in 5/5 (100%) of the patients which suggested a neoplastic process to be evaluated. Gammagraphy was positive in the 3/4 patients on whom it was performed (75%) however; in the case where the gammagraphy was negative when the PET-CT scan was performed it reported an increase in metabolic activity in the first lumbar vertebra, and xiphoid process (Figs. 1 and 2).
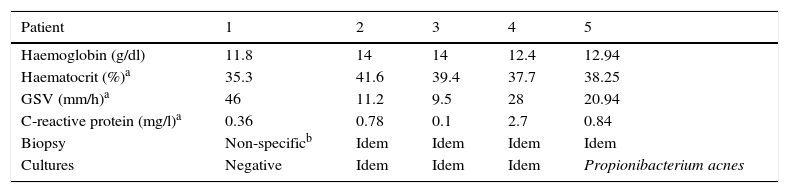
The laboratory tests showed the following mean results: haemoglobin 12.94g/dl (r: 11.8–14g/dl), haematocrit 38.25% (r: 35.3–41.6%) mean corpuscular volume 80.2 (r: 77.7–82.9fL); the serology was also negative, no change was observed in C-reactive protein, however, globular sedimentation velocity (GSV) levels were elevated to 46mm/h and 28mm/h in 2 patients respectively, the first with CRMO and the second with CRUO during the active period of the disease, the mean of the group assessed was 20.94mm/h. No significant differences were observed between the groups (CRUO and CRMO) in elevated GSV levels (Z=−0.57, p>0.05, Mann–Whitney U test) (Table 2).
Laboratory tests performed on patients with chronic recurring osteomyelitis.
The lesions of the 5 patients in the series were biopsied in order to take cultures which were negative in 4 of the 5 cases, and positive in the female patient with chronic recurrent unifocal osteomyelitis in whom a few colonies were isolated of Propionibacterium acnes (P. acnes). Similarly, histopathological analysis showed inflammation characterised by interstitial infiltrates of mononuclear cells with a predominance of plasma cells and the presence of abundant lymphocytes, and accompanying fibrosis and remodelling of the bone trabeculae in all of the cases.
On two occasions a subperisoteal resection of the lesions of 12cm and 14cm was performed on one of the patients with involvement of the tibia; the defect was reconstructed by bone transport surgery before the diagnosis of CRO had been reached. Despite these broad resections the lesion recurred on both occasions.
Empirical antibiotic therapy was started in 3 of the 5 cases studied before a diagnosis of CRO had been made (2 had CRUO and one had CRMO); once the diagnosis had been established all the patients were treated with nonsteroidal anti-inflammatory drugs. Four out of the 5 (3 with CRUO and one with CRMO) patients received naproxen 15mg/kg/weight in cycles of 3–4 months reducing the dose to 250mg every 12h, depending on the response to prolonged treatment, until treatment had been given for 12–16 months. The other patient (CRUO) was treated with 400mg of ibuprofen every 8h according to pain level for 12 months, relief and/or disappearance of pain was considered a good response with or without radiographic improvement of the osteomyelitic foci.
After a mean follow-up of 5.9 years recurrence of the lesions was observed in 3 patients with a mean recurrence at 7 months after discontinuing treatment with NSAIDs (2 with naproxen and one with ibuprofen); no recurrence of symptoms occurred in 2 of the 5 patients, these patients were in the CRUO group treated with naproxen, no statistical differences were observed in recurrence time of the disease between the 2 groups studied (Z=−0.28, p>0.05, Mann–Whitney U test).
DiscussionCRO was first described by Giedion et al.1 in 1972 and since then its aetiopathogenesis is yet to be established. It is believed that it might be a genetic condition which results in an autoimmune disorder in which the inflammatory response is altered.2
With regard to epidemiology, CRO presents in the paediatric ages especially in the age range between 8 and 14 years; however cases have been described in 6-month-old infants and in adults aged over 50. It predominates in females at a female to male ratio of 2:1.3,4 These data coincide with our series, except that the male gender predominates in our study.
The real prevalence of this disease is still unclear due to the few cases recorded in the literature, and the difficulty in diagnosis which might overlap with other autoimmune diseases.3,4
Recent studies suggest an imbalance between proinflammatory cytokines (interleukin-6 and tumour necrosis factor-alpha) and antiinflammatory cytokynes (interleukin-10) to the detriment of the latter, as the pathogenesis basis of CRO.5,6
This disorder can present in isolation or form part of other syndromes such as SAPHO (synovitis, acne, pustulosis, hyperostosis and osteitis) and Majeed syndrome (osteomyelitis, skin rash, dyserythropoietic microcytic anaemia).5–8 In our series, they presented in isolation and no skin lesions were observed. However, it is worth noting the positive cultures in one of the 5 patients in which a few colonies of P. acnes were isolated; this germ has been associated with other inflammatory syndromes such as SAPHO.
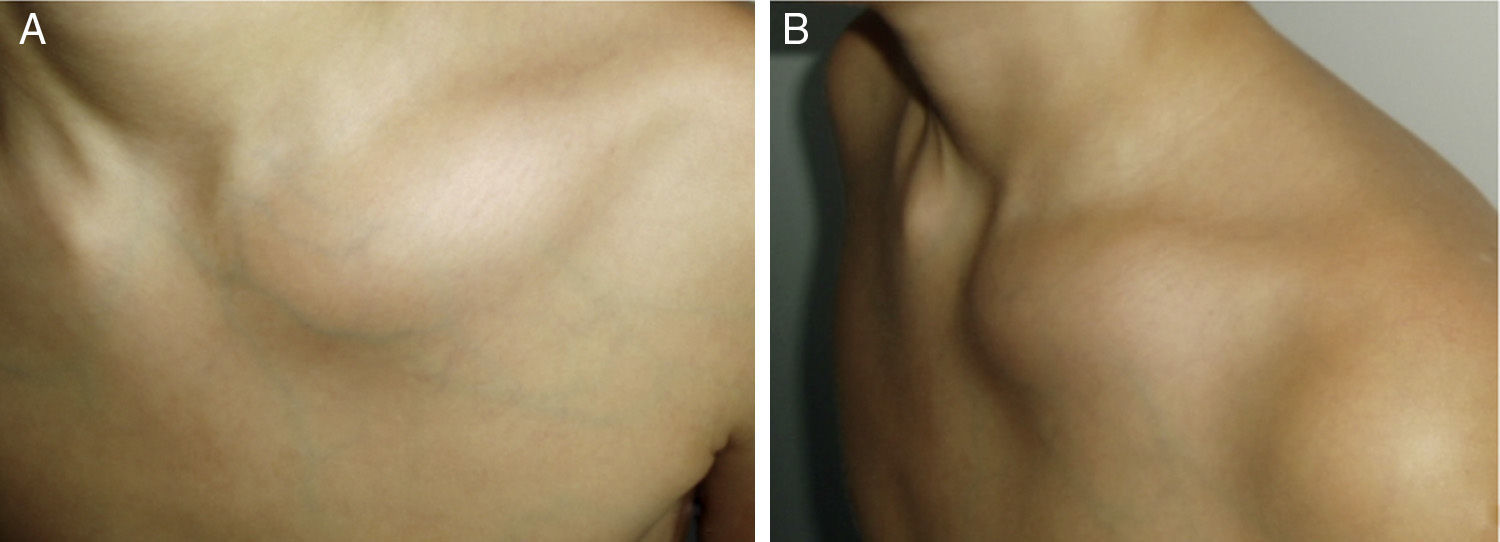
The clinical symptoms are insidious involving pain in the affected bones, mainly at night, accompanied or otherwise by spiking fever and local manifestations of inflammation. Occasionally skin lesions can be observed that present with periods of remission and exacerbation.4–7
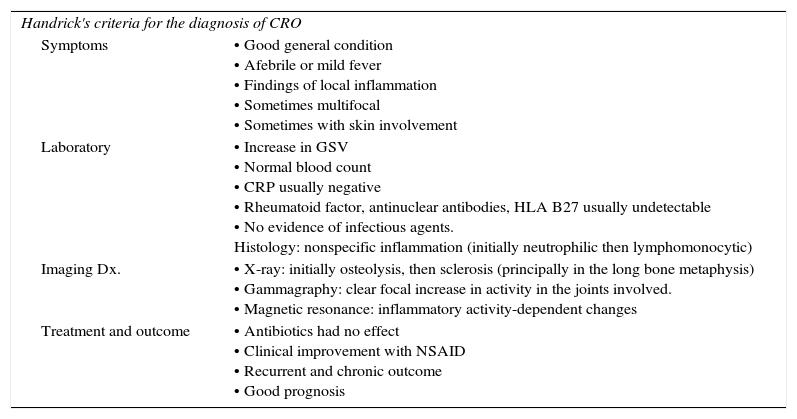
Diagnosis is principally based on clinical symptoms and a high degree of suspicion is required. Handrick9 in 1998 and then Ramanan10 in 2014 suggested criteria to serve as guidelines for diagnosis based on clinical-radiological findings (Tables 3 and 4).
Clinical and paraclinical findings that indicate the presence of CRO.
| Handrick's criteria for the diagnosis of CRO | |
| Symptoms | • Good general condition • Afebrile or mild fever • Findings of local inflammation • Sometimes multifocal • Sometimes with skin involvement |
| Laboratory | • Increase in GSV • Normal blood count • CRP usually negative • Rheumatoid factor, antinuclear antibodies, HLA B27 usually undetectable • No evidence of infectious agents. Histology: nonspecific inflammation (initially neutrophilic then lymphomonocytic) |
| Imaging Dx. | • X-ray: initially osteolysis, then sclerosis (principally in the long bone metaphysis) • Gammagraphy: clear focal increase in activity in the joints involved. • Magnetic resonance: inflammatory activity-dependent changes |
| Treatment and outcome | • Antibiotics had no effect • Clinical improvement with NSAID • Recurrent and chronic outcome • Good prognosis |
Source: Handrick et al.9
Bristol criteria for the diagnosis of CRO.
| • The presence of typical clinicala and radiological findings of CROb in more than one bone (or clavicle alone) without significantly raised inflammatory markers |
| • Typical clinical and radiological findings of CRO in one bone plus inflammatory changes (plasma cells, osteoclass, fibrosis or sclerosis on bone biopsy with no bacterial growth) |
Source: Ramanan et al.10
Laboratory tests only serve to rule out diseases with a similar clinical presentation but they do not provide a certain diagnosis since to date there are no genetic or analytical markers for CRO.
Blood count is usually normal in patients with CRO, although in some cases disturbances such as anaemia with microcytosis and dyserythropoiesis appear, as mentioned by Hendrich.5 These findings are similar to those observed in our series; the patient diagnosed with CRMO presented these changes in their blood count.
The inflammatory markers (GSV, CRP, IL6 and TFN alpha) are usually slightly elevated and tests such as serology and cultures to rule out infectious diseases caused by various germs (Borrelia burgdorferi, Salmonella enteritidis, Yersinia enterocolitica and Campylobacter jejuni) are usually anodyne since this is not an infectious condition.5–7
Imaging studies (X-rays, bone gammagraphy con Tc99, CAT, MRI and PET-CT) are very useful in diagnosis and for staging and follow-up of the bone lesion outcomes. These are initially lytic lesions which subsequently turn sclerotic, with signs of bone remodelling.3
In 1982, Roberts11 proposed a topo-radiographic classification for subacute haematogenous osteomyelitis (Table 5) comprising 4 types and 9 subtypes, which reflects the difficulty in differentiating some of these benign lesions with images of differing appearance from malignant lesions such as osteosarcoma, Ewing's sarcoma and other bone neoplasms, as in type IIB of this classification where the malignant radiographic appearance might lead to errors in deciding treatment and subjecting CRO patients to unnecessary interventions. In our series the patient underwent broad resection of the tibia on two occasions because it was uncertain whether the condition was of possible tumour or septic origin.
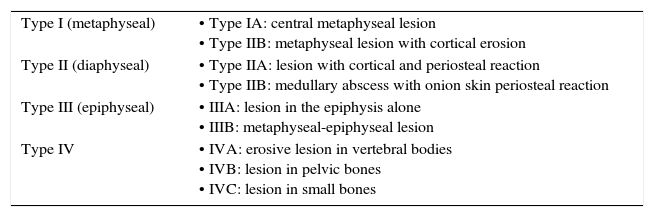
Robert's classification of subacute haematogenous osteomyelitis.
| Type I (metaphyseal) | • Type IA: central metaphyseal lesion • Type IIB: metaphyseal lesion with cortical erosion |
| Type II (diaphyseal) | • Type IIA: lesion with cortical and periosteal reaction • Type IIB: medullary abscess with onion skin periosteal reaction |
| Type III (epiphyseal) | • IIIA: lesion in the epiphysis alone • IIIB: metaphyseal-epiphyseal lesion |
| Type IV | • IVA: erosive lesion in vertebral bodies • IVB: lesion in pelvic bones • IVC: lesion in small bones |
Source: Roberts et al.11
Most of the patients in the series were referred to our centre to assess the initial diagnostic possibility of neoplastic disease with bone involvement. Anatomopathological studies are useful in ruling out other diseases, but the findings in CRO are no more than non-specific inflammatory changes such as lymphoplasmacytic infiltrates and fibrosis in advanced stages.5,7
A differential diagnosis should be made with other disorders of a similar clinical presentation such as infectious osteomyelitis, hypophosphatasia, histiocytosis, leukaemia, lymphoma, osteosarcoma, deficiency of the interleukin-1-receptor antagonist (DIRA), etc.5,7,12
With regard to treatment, the first therapeutic option should be nonsteroidal anti-inflammatory drugs administered over long periods (12–18 months) with excellent results, especially the naproxen we used in our series, although good results have been reported with indomethacin as an NSAID of choice for these lesions. Other treatments such as sulfasalazine, glucocorticoids, and bisphosphonates. Interferon-alpha and tumour necrosis factor-alpha inhibitors are considered a second choice and are generally used as coadjuvant treatment, they require more long term studies to assess their effectiveness in isolation compared to their use with NSAIDs.5–7,11–14
Girschick et al.,7 treated 27 patients with a dose of 15mg/kg/day of naproxen with good outcomes at 6 months in patients who had only had one relapse, recommending treatment up to 25 months for patients with multiple relapses, in 25% of the patients the treatment was not effective. Likewise, Beck12 observed in another cohort study that in 43% of 37 patients treated with naproxen alone the treatment was effective at 6 months after it had been started. In our study 100% of the patients had good outcomes after treatment with NSAIDs; however, in 3 of the 5 cases there was a recurrence of clinical symptoms.
With regard to the use of other NSAIDs such as indomethacin for the treatment CRO, Abril and Ramírez14 observed excellent outcomes with 100% clinical improvement in their series of 5 patients followed up over a period of 4 years, the bone lesions persisted in one of the 5 patients. These results are comparable with those achieved using naproxen in our series, demonstrating that NSAIDs are the first option in designing a therapeutic strategy to tackle this disease.
ConclusionsChronic recurrent osteomyelitis is a disease that poses a diagnostic challenge due to its natural history and clinical presentation which resembles other entities like infection or malignant disease such as Ewing's sarcoma, osteosarcoma or metastatic disease, amongst others. These factors in addition to most tests returning negative results often leads to an error in the initial diagnosis and consequently inappropriate treatment. For this reason, clinical suspicion is essential in order to guide diagnosis.
The long term prognosis for this disease is very good and NSAIDs are the drugs of choice. They require prolonged periods of treatment which have demonstrated good outcomes (Figs. 3–5).
Patient 5. Lesion in distal 1/3 of the radius. (A) X-ray showing well-defined radiolucent image in distal 1/3 of the radius with areas of sclerosis. (B) and (C) the MRI shows a lesion with a mixed-type intraosseous component, with lytic areas and other areas which seem to relate to bone formation, and adjacent soft tissue oedema.
Level of evidence IV.
Ethical disclosuresProtection of people and animalsThe authors declare that neither human nor animal testing have been carried out under this research.
Confidentiality of dataThe authors declare that they have complied with their work centre protocols for the publication of patient data.
Right to privacy and informed consentThe authors declare that no patients’ data appear in this article.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Rivas Felice J, González Herranz P, Mejía Casado A, Pérez Navarro R, Hernández Díaz R. Osteomielitis crónica recurrente: un reto diagnóstico y terapéutico. 2017;61:35–42.