The treatment of 3 and 4 part proximal humeral fractures in elderly patients is still controversial. The frequent co-existence of poor quality bone and rotator cuff abnormalities in patients with multiple clinical conditions and with difficulties for physical rehabilitation leads to disappointing clinical results, even when the radiological images are acceptable.
ObjectiveTo evaluate the clinical, radiological, and functional results in patients over 65 years old with complex proximal humerus fractures treated with reverse shoulder arthroplasty.
Material and methodsA prospective review was carried out on 30 patients (26 women and 4 men) with proximal humeral fractures treated with reverse shoulder arthroplasty in our department. The mean age was 74.9 years (SD=6.3), and the mean follow-up was 34.5 months (SD=19.3).
ResultsClinical and functional results were acceptable, with a mean forward flexion of 124° and a mean external rotation of 13°. The mean abbreviated Constant abbreviated score was 49.1 (SD=14.1), 27 (SD=6.3) in the UCLA scale, and 32.2 (SD=19.2) in the QuickDASH questionnaire. The large majority (80%) of the patients are pain free, and they do not need medication to do daily activities. The complication rate was 13.3%.
ConclusionsWe consider that reverse shoulder arthroplasty is a valid option to treat 3 and 4 part proximal humeral fractures in elderly patients. The surgical goals should include the anatomical reconstruction of the tuberosities, avoiding enlargement of the operated arm greater than 2cm.
El tratamiento de las fracturas en 3 y 4 fragmentos de húmero proximal en el paciente anciano resulta controvertido. La frecuente coexistencia de un hueso de mala calidad y la afección del manguito rotador con dificultades para el tratamiento rehabilitador en pacientes pluripatológicos conlleva, en muchas ocasiones, resultados clínicos decepcionantes, aun cuando el resultado radiológico sea aceptable.
ObjetivoEvaluar los resultados clínicos, radiológicos y funcionales obtenidos en el tratamiento de las fracturas de húmero proximal complejas con prótesis inversa en pacientes mayores de 65 años de nuestro servicio.
Material y métodosRevisión prospectiva en la que incluimos a 30 pacientes con fractura de húmero proximal intervenidos en nuestro servicio con prótesis total inversa de hombro. De ellos, 26 eran mujeres y 4 hombres. La edad media fue de 74,9 años (DE=6,6). El seguimiento medio fue de 34,5 meses (DE=19,3).
ResultadosEl resultado clínico y funcional ha sido aceptable, con una antepulsión activa media de 124° y una rotación externa media de 13°. La puntuación media en la escala abreviada de Constant fue de 49,1 puntos (DE=14,1), en la escala UCLA fue de 27 puntos (SD=6,3) y en el cuestionario QuickDASH de 32,2 puntos (DE=19,2). El 80% de los pacientes están libres de dolor sin precisar analgesia para la realización de sus actividades habituales. El 95% de los pacientes estaban satisfechos o muy satisfechos tras la intervención. La tasa de complicaciones fue del 13,3%.
ConclusionesConsideramos la artroplastia total inversa como una opción válida en el tratamiento de las fracturas en 3 y 4 fragmentos de húmero proximal en pacientes mayores de 65 años. Los objetivos de la cirugía deben incluir la reconstrucción anatómica de las tuberosidades, evitando incrementos de la longitud del miembro intervenido superiores a 2cm.
Proximal humeral fracture ranks third as the most common type of fracture in the elderly, only behind distal radius and hip fracture. They comprise almost 10% of all fractures,1 their incidence is greater in women and increases with age, reaching their maximum their peak in the eighth decade of life.1,2
Between 50% and 80% are fractures that are barely or not at all displaced2 for which orthopaedic treatment achieves good functional outcomes and union rates close to 100%.3 By contrast, conservative treatment of displaced or comminuted fractures is associated with complication rates of 48%,4 such as varus collapse or necrosis of the humeral head. Therefore, surgery should be considered for active elderly patients with fractures in 3 and 4 fragments.
The association with osteoporosis, previous involvement of the rotator cuff and multiple comorbidities makes surgical treatment complex in these patients. Recent studies highlight the lack of consensus on the management of these types of patients, there being no clear differences between conservative treatment or surgery.5,6 Open reduction and internal fixation obtain inconsistent results in terms of function, articular range and postoperative pain. Even since the introduction of locking plates, complications such as loss of reduction and screw penetration vary between 21% and 43%, with published reoperation rates of up to 19%.7
Neer2 proposed hemiarthroplasty when reconstruction by osteosynthesis is not possible or the affected area of the humeral head articular surface is very extensive. This provides pain relief for most patients, but recovery of mobility and degree of satisfaction relate directly to the union of tuberosities. It is essential that they are anatomically reconstructed and rehabilitation must be delayed until there is radiographic evidence of union.8 Some studies report migration rates of 50%,9 lack of union in 46% of cases10 and worse outcomes in women aged over 75 years.9
Total reverse shoulder arthroplasty was initially conceived for the treatment of rotator cuff arthropathy, but problems associated with hemiarthroplasty have widened its indications for treating proximal humeral fractures in elderly patients.
The objective of this study is to assess the clinical, radiological and functional outcomes achieved after treatment of complex humeral fractures with reverse prosthesis in patients aged over 65 years in our department.
Material and methodsWith the approval of our hospital's Ethics Committee we undertook a descriptive, prospective study that included 30 consecutive patients, aged over 65 years, treated by total reverse shoulder arthroplasty for proximal humeral fracture during the period between December 2008 and June 2014. All the patients gave their consent to participate in the study.
The mean age of the patients treated was 74.9 years (SD=6.3). Of the total number of patients, 26 were female (87%) and 4 male (13%) and the fracture type, according to Neer's2 classification, was 3 fragments in 27% of the subjects and 4 in 73%.
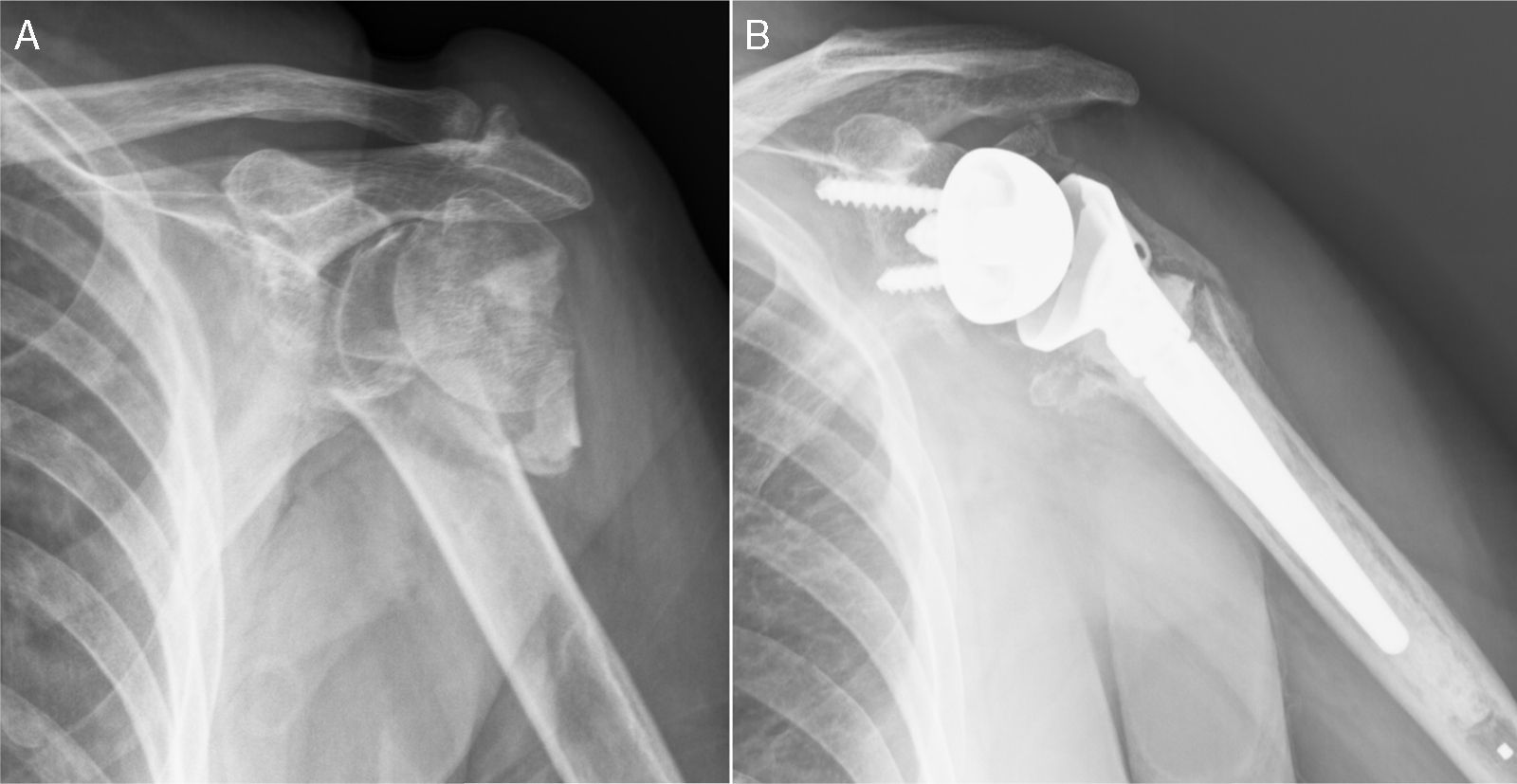
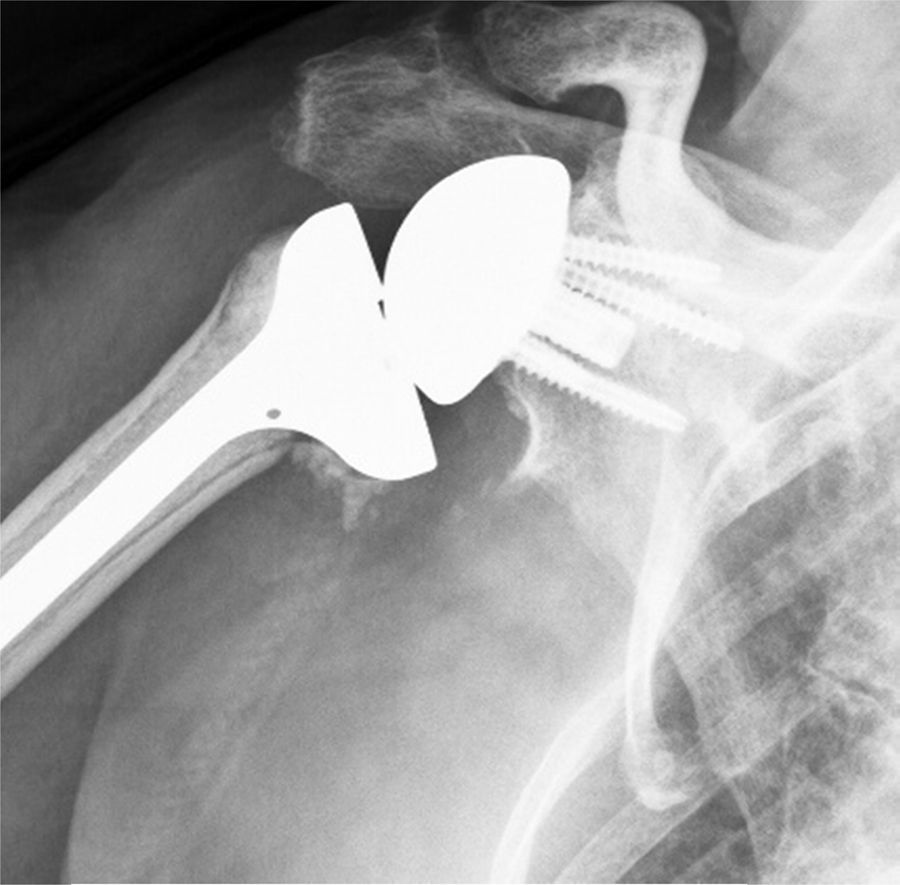
Patients aged over 65 years with proximal humeral fractures in 3 and 4 fragments were included in the study, with risk factors that could compromise the outcome of treatment with osteosynthesis or hemiarthroplasty: unreconstructable fractures, high risk of avascular necrosis, severe osteoporosis and prior rotator cuff injury (Fig. 1). Patients with permanent injury to the axillary nerve or all of the brachial plexus, with disease that might associate severe dysfunction of the deltoid muscle or with glenoid fractures which would hinder correct anchoring of the metaglene were excluded from the study.
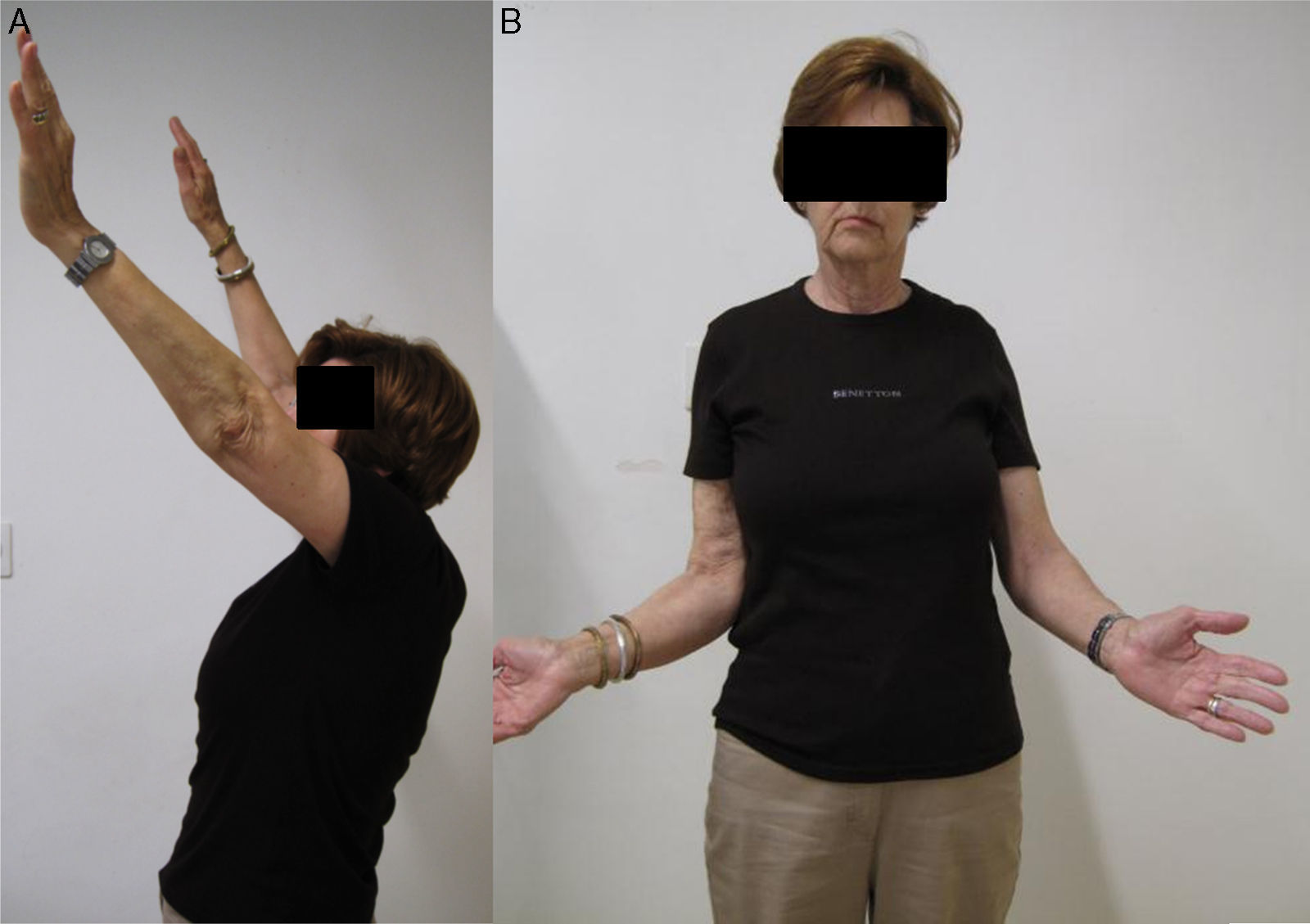
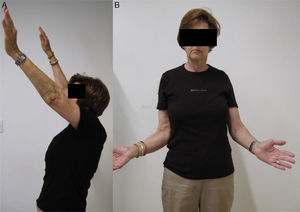
All the patients were followed up clinically and radiologically in our centre's outpatient department at 1 month, 6 months and annually (Fig. 2). We used scores from the abbreviated Constant scale11 (which leaves out measurement of strength, with a maximum possible score of 75 points), the Disabilities of the Arm, Shoulder and Hand questionnaire (QuickDASH)12 and the UCLA scale13 to evaluate the clinical outcomes.
Internal, external and axillary rotation anteroposterior views were taken at all follow-up visits to assess the radiographic outcomes. We recorded scapular neck notching according to the classification by Sirveaux et al.,14 loosening of the glenoid component according to the classification by Cuff et al.15 and signs of humeral component loosening using the criteria proposed by Sperling et al.16 We considered that the tuberosities had healed anatomically when, on the anteroposterior view in neutral position, the distance between the tubercle and the proximal edge of the prosthesis was from 5mm to 20mm below the proximal end of the prosthesis.8
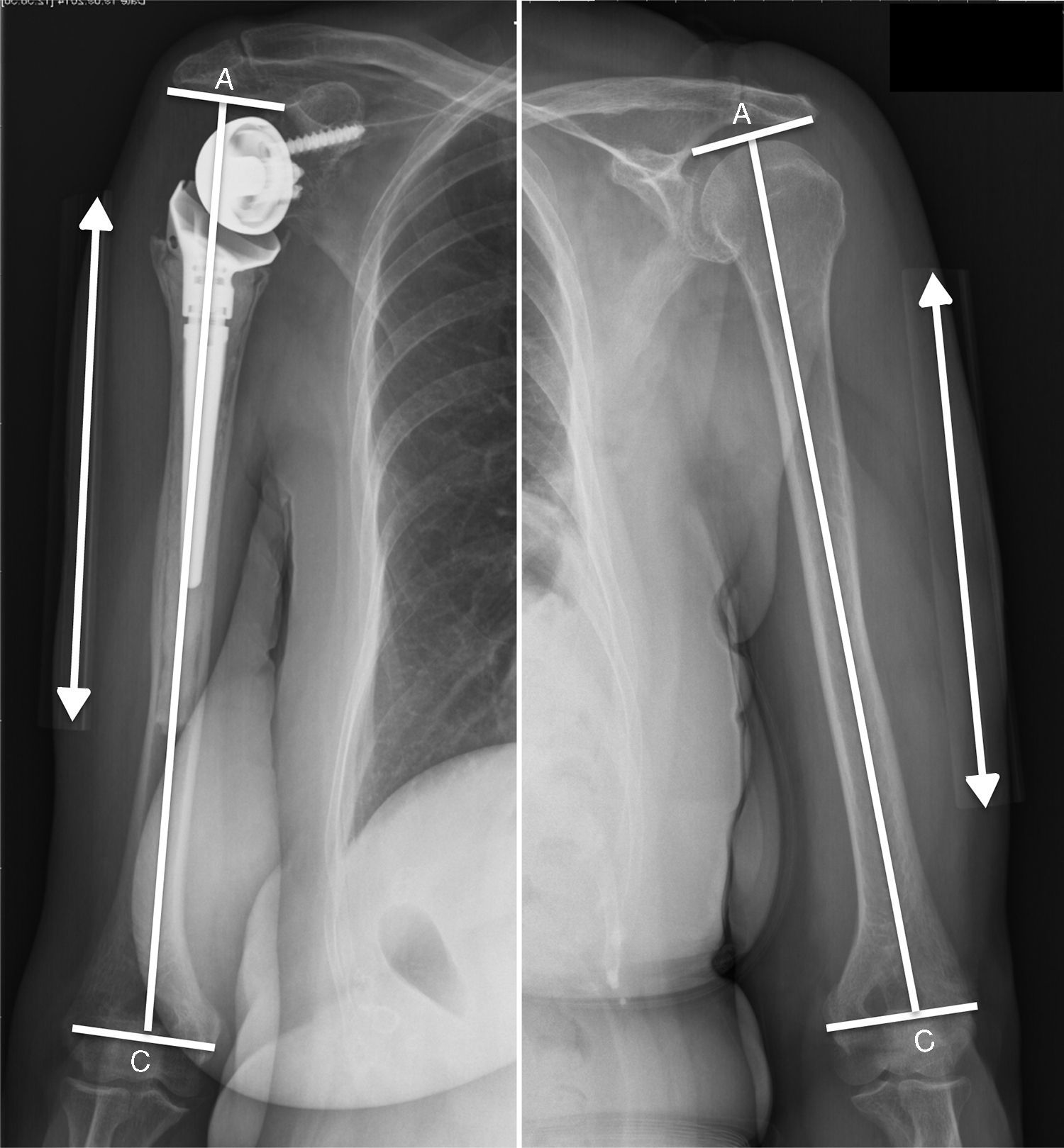
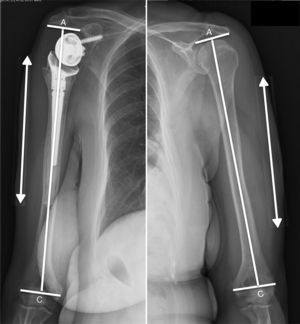
As an objective measurement of the restoration of appropriate tension of the deltoid, we measured the lengthening caused to the operated arm using the method proposed by Läderman.17 To that end, anteroposterior X-rays of the operated and the contralateral arm were taken with the limb in the neutral position and with the patient in the standing position. We placed a graduated ruler to adhere to the skin of the mid lateral area of the arm to correct the magnification caused by the X-ray machine, which has to focus its beam on the middle third of the humeral diaphysis. We measured the difference in the acromion–epicondyle distance (distance A–C) in the radiographic checks of the operated arm and the contralateral arm (Fig. 3).
Method proposed by Lädermann et al.17 for measuring the lengthening caused in the operated arm. Three main lines are used to determine the relative lengthening caused in the operated arm, the epicondylar line, the diaphyseal axis line and a third line, perpendicular to the diaphyseal axis, which crosses the most lateral and lower point of the acromion. Lengthening is determined by the difference in the acromion–epicondyle distance (A–C) between the operated arm and the contralateral arm.
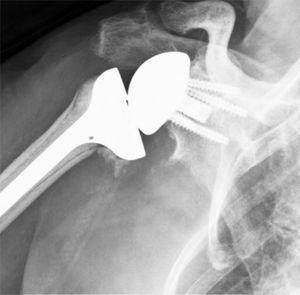
All the cases were operated by 2 surgeons specifically trained in reconstructive shoulder surgery. A deltopectoral approach was used. We used the Lima SMR model as the prosthetic implant, and we opted for cemented humeral stem fixation, with 30° retroversion in all of the operations. The glenosphere size was 36mm in 82% of the cases and 40mm in the remaining 18%. The tuberosities were reconstructed in all of the operations, with nonresorbable material (Ethibond No. 5) using horizontal sutures, vertical to the diaphysis and cerclage to the calcar, and the addition of a humeral head autograft and exeresis of the supraspinatus tendon remnant. The mean surgery time was 90.2min (SD=12.2).
After surgery, the shoulder was immobilised using a sling for 3 weeks after which pendular exercises that the patients had been taught during admission, and passive abduction and antepulsion to 90° were allowed. Rehabilitation was delayed until the sixth postoperative week.
Statistical analysisData analysis was carried out using the statistical software STATA version 12. A descriptive analysis was undertaken, expressing the quantitative variables as means or medians according to the symmetry of the distribution and the qualitative variables as absolute and relative frequencies. The analytical results were undertaken using bivariate techniques: Student's t-Fisher test (quantitative variables) and X2 (qualitative variables), assuming a statistical significance of p<0.05. The ANOVA test was used with Bonferroni correction for multiple comparisons, with a 95% significance limit.
ResultsThe mean follow-up time of the patients was 34.5 months (SD=19.3). The mean articular balance after surgery was 124° (SD=30.3) anterior flexion, 95° (SD=34.7) abduction, 13° (SD=28) external rotation with the arm in abduction and L5 was the anatomic region most frequently reached on internal rotation.
The mean score on the abbreviated Constant scale11 was 49.1 points (SD=14.1) out of 75 possible scores. The mean score on the UCLA scale13 was 27 points (SD=6.3) and on the QuickDASH14 questionnaire it was 32.2 points (SD=19.2). Eighty percent of the operated patients had no pain or mild pain, which was relieved with occasional analgesia. The level of satisfaction was very high, 95% of the patients were satisfied or very satisfied with the outcome of the operation. One hundred percent would undergo the operation again using the same technique if they were to sustain a fracture to the contralateral shoulder.
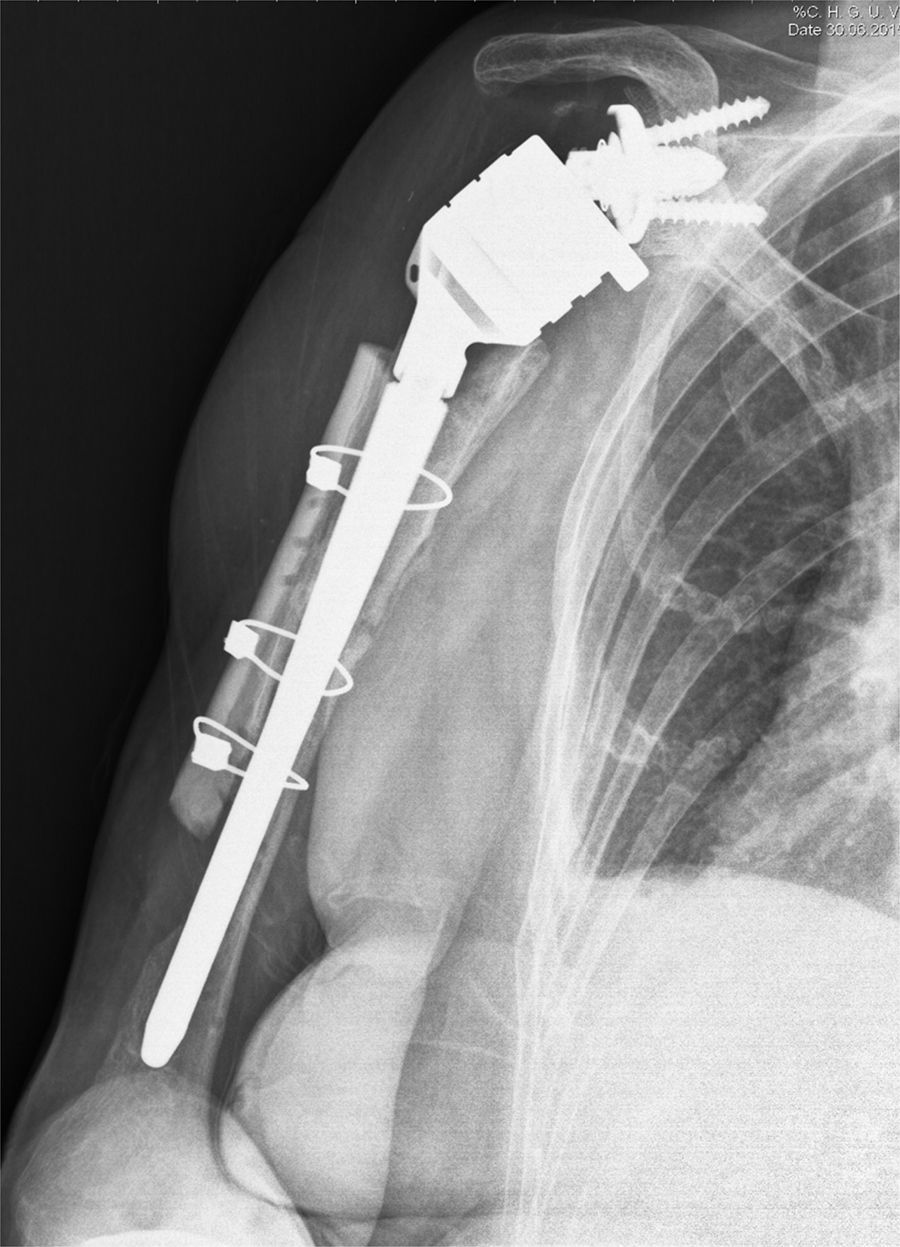
The rate of complications was 13.3% (4 patients). An intraoperative fracture of the humerus occurred in 2 cases, treated using cerclages and humeral head autograft. The same patient sustained 3 postoperative periprosthetic fractures, after 3 successive episodes of accidental trauma. The first 2, in whom the fracture line was located around the tip of the stem, were treated with osteosynthesis with a plate, cerclages and structural allograft (cortical table). In the latter case, with a fracture line distal to the tip of the stem, we opted for long stem replacement, cerclages and the addition of a structural allograft and bone morphogenic protein due to poor bone stock (Fig. 4). The patient is currently pain free with a score of 40 on the abbreviated Constant scale. Finally, one patient presented a deep Sf. epidermidis infection treated by resection arthroplasty. We had no cases of luxation, neurological complications, acromion fracture or component loosening.
Radiographic follow-up at 6 months after surgery due to a third periprosthetic fracture after 3 different and successive falls in the same patient. A lateral cortical defect can be observed in the distal third of the humerus. A cortical allograft was not added in this area due to the risk of causing too much tension on the radial nerve.
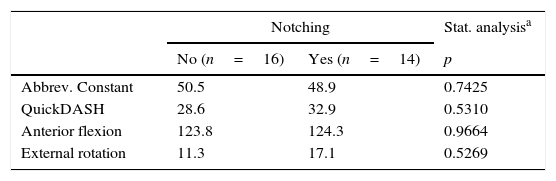
With regard to radiographic findings, 14 patients (46%) presented scapular notching in the anteroposterior view. According to Sirveaux’9 classification, 11 patients had grade i notching and 3 patients grade ii (Fig. 5). We found no association between the presence of scapular notching in the radiographic checks and the onset of pain, abbreviated Constant score11 or QuickDASH12 questionnaire score (Table 1).
Type II scapular notching according to Sirveaux’14 classification (reaches the lower screw). Most of the patients did not present notching or presented type I notching.
Influence of the onset of scapular notching on outcomes (mean scores) in the abbreviated Constant and QuickDASH and mobility in anterior flexion and external rotation functional scores.
| Notching | Stat. analysisa | ||
|---|---|---|---|
| No (n=16) | Yes (n=14) | p | |
| Abbrev. Constant | 50.5 | 48.9 | 0.7425 |
| QuickDASH | 28.6 | 32.9 | 0.5310 |
| Anterior flexion | 123.8 | 124.3 | 0.9664 |
| External rotation | 11.3 | 17.1 | 0.5269 |
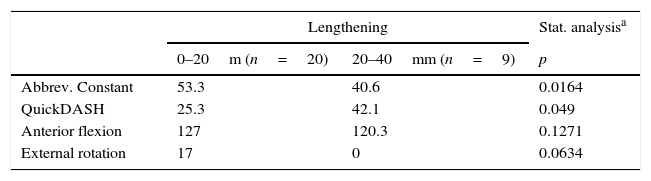
The increase in the mean length of the operated limb, compared to the contralateral limb was 13.4mm (SD=9.3). The operated arm was shortened in only one case. The articular balance of this patient was 100° anterior flexion and −20° external rotation, with a score of 28 on the abbreviated Constant11 scale and of 75 on the QuickDASH12 questionnaire. Lengthening was between 0 and 20mm in 20 patients and in 9 cases lengthening was greater than 20mm. The group with lengthening of the operated arm of less than 20mm achieved better mean scores on both the abbreviated Constant11 (53.3 compared to 40.6) and on the QuickDASH12 questionnaire (25.3 compared to 42.1). These differences on the functional scales were statistically significant. Mobility in anterior flexion was also better in the group with lengthening of less than 20mm, although the difference was only 7°, and was not statistically significant (Table 2).
Influence of the lengthening caused to the operated arm on outcomes (mean scores) on the abbreviated Constant score and QuickDASH and mobility in anterior flexion and external rotation functional scores.
| Lengthening | Stat. analysisa | ||
|---|---|---|---|
| 0–20m (n=20) | 20–40mm (n=9) | p | |
| Abbrev. Constant | 53.3 | 40.6 | 0.0164 |
| QuickDASH | 25.3 | 42.1 | 0.049 |
| Anterior flexion | 127 | 120.3 | 0.1271 |
| External rotation | 17 | 0 | 0.0634 |
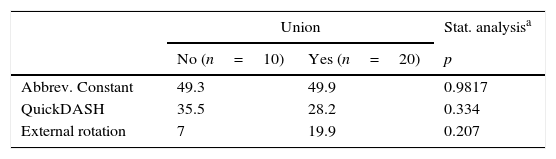
In 67% of the patients the tuberosities healed anatomically. Migration or lack of healing of the tuberosities was observed in 33%. The group with anatomic healing presented better mobility outcomes on external rotation (20° compared to 7°) and better mean QuickDASH12 scores (28.2 compared to 35.5 points) although these differences were not statistically significant (Table 3).
Influence of anatomical union of the tuberosities on the outcomes (mean scores) in the abbreviated Constant score, QuickDASH and mobility in external rotation functional scores.
| Union | Stat. analysisa | ||
|---|---|---|---|
| No (n=10) | Yes (n=20) | p | |
| Abbrev. Constant | 49.3 | 49.9 | 0.9817 |
| QuickDASH | 35.5 | 28.2 | 0.334 |
| External rotation | 7 | 19.9 | 0.207 |
Treatment of complex proximal humerus fractures with reverse shoulder arthroplasty is a good option for patients with risk factors that compromise outcomes after osteosynthesis or hemiarthroplasty: severe osteoporosis, high risk of avascular necrosis, unreconstructable fractures, difficulty in anatomical healing of tuberosities or cases where absence of a competent rotator cuff is anticipated.
In our series, we assessed the functional outcomes of 30 patients with a mean follow-up of 34.5 months. We obtained a mean value of 124° for anterior flexion and 12° for external rotation. The anterior flexion values are similar to those found in previous studies, where recovery of mobility varied between 97°18 and 138°.19 Mobility in external rotation is also similar to the majority of published studies, which report mean values between 8° and 13°, and lower than the 30° recorded by Klein et al.20 or Gallinet et al.21 and the 49° obtained by Young et al.22 Our mean score on the Constant scale was somewhat lower than the majority of publications18–21,23,24 at 49.1 points out of a maximum of 75, because we used the abbreviated Constant scale. Strength assessment is omitted in this scale due to the lack of standardisation of the method for measuring this parameter.20 The effect of this over the final outcome is not very important, because strength levels in this population are generally low.
The decrease and medialisation of the centre of rotation of the glenohumeral joint increases the deltoid lever arm and enables recruitment of a greater number of fibres of the anterior and posterior bellies. Shortening of the operated arm compared to its initial length results in a lack of deltoid tension with poorer functional outcomes and a higher incidence of luxation.17 The factors that predispose to shortening of the arm include revision surgery, posttraumatic arthritis or fracture sequelae with shortening of the arm prior to surgery, or the use of a superolateral approach that usually results in greater bone resection. Excessive lengthening increases the risk of complications such as injury to the nerve or acromion fractures.17,25 In our series, only one patient who had no predisposing factor had shortening of the operated limb, therefore the reduction in the length of the operated arm was probably due to his having sustained a fracture with significant metaphyseal comminution.
We compared the group of patients with postoperative lengthening of less than 20mm and the group with lengthening greater than 20mm. The mean anterior flexion was slightly better in the group with lengthening less than 20mm. The mean scores on the abbreviated Constant scale and the QuickDASH questionnaire were also better. These differences in the function scales were statistically significant. The objective of ideal tension would be to restore the anatomy of the healthy shoulder. The acromiohumeral distance will depend on the thickness of the polyethylene, the size of the implant, the use of an eccentric glenosphere and position of the glenosphere in the vertical plane.26 In our study, lengthening greater than 20mm of the operated arm is the benchmark threshold from which the functional outcomes stop improving. There is room for longer term follow-up, since several studies27 refer to functional deterioration after 6–8 years, associated with the gradual distension of the deltoid fibres.
One of the problems associated with reverse prosthesis is the systematic absence of shoulder rotation, which has negative repercussions on the patient's daily activities. Several studies21 have established a relationship between anatomic healing of tuberosities with better overall mobility outcomes, especially in rotations, and the Constant score. In 67% of our patients the tuberosities healed anatomically, and 33% migrated or did not heal. We observed better outcomes in shoulder external rotation mobility (20° compared to 7°) and a lower score on the QuickDASH questionnaire in the group with anatomically healed tuberosities. These differences were not significant. Our outcomes are similar to those published by Gallinet et al.21 (66%), although we did not obtain such clear differences in favour of the group with anatomical healing. Several authors have published rates of nonunion or migration of tuberosities varying between 0% and 46%.19 Surgical gestures, such as resection of the residual supraspinatus tendon or addition of a bone graft,9 promote union of the tuberosities in the right position. Furthermore, with reverse arthroplasty, the final outcome does not depend so much on this parameter as in the case of hemiarthroplasty,28 since cases with migration or nonunion of tuberosities achieve acceptable outcomes.
Our rate of complications was 13.3%. These chiefly comprised intra and postoperative fractures and one prosthetic infection. We had no cases of luxation, neurological complications or acromion fractures. Published rates of complications vary between 5% and 40%.29 Our rate, greater than that of Gallinet et al.,21 lies within those shown in the series of Bufquin18 (28%), Klein20 (15%) and Cazeneuve23,24 (13%).
Scapular notching is a finding specific to reverse prostheses. Forty-six percent of our patients presented scapular notching, in most cases this was mild (grade I–II according to Sirveaux14), perhaps due to the short follow-up period. Levigne14 presents rates of 68% after a mean 4 year follow-up and Cazeneuve24 57% after 6.5 years, with greater percentages of grades III and IV than our series. Hernández-Elena et al.30 record notching rates of 29%, although with a shorter mean follow-up (24 months). We found no relationship between the presence of scapular notching and functional outcomes or pain. None of the patients presented radiographic signs of glenoid component loosening. Levigne31 indicates that upward tilt of the glenoid component, as a consequence of erosion of the upper part of the glenoid, might encourage notching. Hernández-Elena et al.30 indicate that increased glenoid tilt (the angle formed by the intersection of a line parallel to the metaglene pin and another line perpendicular to the glenoid neck) might prevent its onset. The use of eccentric glenoid components or lateralised glenosphere helps to reduce its incidence, but at the expense of increased shear forces in the bone-base interface of the glenoid component. Placing a structural allograft to lateralise the glenosphere is a good option to reduce these shear forces.29
The small sample size is a limitation of our study, which makes it difficult to establish cause-effect relationships, and a relatively short follow-up period which did not enable the long term outcomes of these patients to be established. Although our hospital's Radiology Department technicians were instructed on the correct method of obtaining the necessary views for measuring the lengthening caused by surgery, it is possible that some measurements were affected by the radiological view. We do not have a group of patients treated with a different therapeutic alternative in order to compare outcomes.
ConclusionIn view of the outcomes achieved, we consider that total reverse arthroplasty is a valid procedure in the treatment of proximal humerus fractures in patients over 65 years of age. The functional outcomes with this type of implant are predictable and our rate of complications is low. However, the surgical technique is challenging: we should concentrate our efforts on achieving anatomic reconstruction of the tuberosities and avoiding increases in the length of the operated limb in excess of 2cm.
Level of evidenceLevel of evidence IV.
Ethical responsibilitiesData confidentialityThe authors declare that no patients’ data appear in this article.
Protection of people and animalsThe authors declare that neither human nor animal testing have been carried out under this research.
Right to privacy and informed consentThe authors declare that no patients’ data appear in this article.
Conflict of interestsThe authors have no conflict of interest to declare.
Please cite this article as: Villodre-Jiménez J, Estrems-Díaz V, Diranzo-García J, Bru-Pomer A. Tratamiento de las fracturas de húmero proximal en pacientes mayores de 65 años con prótesis inversa: resultados y complicaciones. Rev Esp Cir Ortop Traumatol. 2017;61:43–50.