In trapeziometacarpal osteoarthritis (or rhizarthrosis), there is great controversy over the surgical technique to choose: simple trapeziectomy, resection-interposition arthroplasty, interposition arthroplasty suspension or arthroplasty with implant or prosthesis. These latter 2 are the most used without consensus in the literature on the technique to choose and without sufficient comparative studies.
The objective is to compare the 2 techniques most used today: suspension-interposition arthroplasty and arthroplasty with prosthesis.
Material and methodA prospective study was conducted on 15 patients diagnosed with grade 2–3 rhizarthrosis treated with interposition arthroplasty-suspension (group 1) and 15 with prosthesis (group 2) showing clinical outcomes, advantages and disadvantages of each. The study variables were the visual analogue scale (VAS), the DASH questionnaire, the grip strength, the strength of end to end and end-lateral clamp, the joint balance adduction–abduction and preemption-retropositioning, and the opposition. The 2 groups are from 2 different hospitals operated on by a hand surgeon from the Hand Unit. The follow-up time for all patients included in the study was 12 months.
ResultsThe VAS, DASH and grip strength at 12 months did not show significant differences. As regards the strength of end to end and end-lateral clamp, group 2 showed the highest values in all follow-up periods with statistically significant differences.
ConclusionsPatient selection and surgical experience is essential, given the satisfactory results of both techniques. Arthroplasty prosthesis is reserved for grades 2 and 3, middle-aged patients, good trapezium architecture, and experienced surgeons.
En la rizartrosis del pulgar existe gran controversia sobre la técnica quirúrgica a elegir: trapeciectomía simple, artroplastia de resección-interposición, artroplastia de resección-suspensión, artrodesis, artroplastia de suspensión-resección-interposición o artroplastia con prótesis. Estas 2 últimas son las más empleadas, sin consenso en la literatura sobre la técnica a elegir y sin suficientes estudios comparativos.
El objetivo es comparar las 2 técnicas más empleadas en la actualidad: artroplastia de resección-suspensión y artroplastia con prótesis.
Material y métodoPresentamos un estudio prospectivo de 15 pacientes diagnosticados de rizartrosis del pulgar grados ii-iii tratados con artroplastia de resección-suspensión (grupo 1) y 15 con prótesis (grupo 2) mostrando resultados clínicos, ventajas e inconvenientes de cada una. Como variables se emplearon la escala EVA, el cuestionario DASH, la fuerza de puño y de pinza terminoterminal y terminolateral; el balance articular en aducción-abducción, en anteposición-retroposición y la oposición. Los 2 grupos son de 2 hospitales diferentes, intervenidos por un cirujano de mano de la unidad. El tiempo de seguimiento para todos los pacientes incluidos fue de 12 meses.
ResultadosEl EVA, DASH y fuerza de puño a los 12 meses no muestran diferencias significativas; en cuanto a la fuerza de pinza terminoterminal y terminolateral, el grupo 2 mostró los mayores valores en todos los periodos de seguimiento, con diferencias estadísticamente significativas.
ConclusionesEs fundamental la selección del paciente y la experiencia del cirujano, dados los resultados satisfactorios de ambas técnicas. La artroplastia con prótesis se reserva para grados ii y iii, pacientes de mediana edad, buena arquitectura del trapecio y cirujanos con experiencia.
The widest range of thumb mobility is achieved in the trapeziometacarpal (TMC) joint, which Fick described by coining the term “saddle joint” in 1854.1
Degenerative pathology of the TMC joint is known as trapeziometacarpal osteoarthritis or rhizarthrosis. It accounts for 10% of osteoarthritis cases in the limbs and 8% in the general population.2 It is more frequent among postmenopausal women and those aged over 50 years. It can appear associated to other hand pathologies, such as carpal tunnel syndrome and De Quervain's disease. There have also been reports of cases secondary to trauma and appearing after fractures of the trapezium or the metacarpal base. Bilateral involvement is more frequent in females, in nearly 60% of cases.2 An overload develops on the joint as a consequence of a repetitive use of the thumb combined with joint incongruence and ligament instability; joint surfaces are subjected to greater compression forces, which damage the cartilage. In an attempt to avoid excessive compression, the base of the metacarpal produces a dorsoradial subluxation: the thumb gains adduction progressively.
The main symptom leading patients to the clinic is pain. In initial phases it appears during movements requiring a strong pinch and in advanced phases it is present even at rest. Deformity is another reason to attend the clinic, in some cases producing a “Z-thumb” deformity in the more advanced stages. Disease progression makes the joint more rigid and causes a loss of mobility, as the deformity in adduction of the metacarpal becomes more established. Another frequent complaint is loss of strength, particularly for tasks requiring a lateroterminal and terminoterminal pinch movement.
Simple radiograph is the main diagnostic test. Currently, the most commonly used classification is that established by Eaton and Glickel,3 which distinguishes between 4 stages.
Conservative treatment (medication, physiotherapy, orthesis and joint infiltration) usually represents the first therapeutic measure. The main indications for surgical treatment include pain, deformity and functional disability interfering with daily life activities, together with lack of response to conservative treatment. Various surgical techniques are available.
Simple trapeziectomy is indicated in stages II–IV. This technique entails complications, such as instability and loss of height of the column of the thumb. Although several studies have reported promising results, others consider it as a technique aimed at elderly patients with low functional requirements.4
Trapeziectomy with tissue interposition (resection-interposition arthroplasty) was initially used to prevent proximal migration of the metacarpal.
Trapeziectomy with ligament reconstruction (resection-suspension arthroplasty) also began to be used to avoid instability and proximal migration of the first metacarpal. The tendons of the flexor carpi radialis (FCR) and accessory of the abductor pollicis longus (APL) are the most commonly employed in ligament reconstruction.5 This technique can be employed in stages II–IV. There are several sub-variants of this technique.
Prosthetic replacement is used for TMC osteoarthritis and consists in replacing the degenerated joint surfaces of the trapezium and metacarpal by prosthetic components. The prosthesis cannot be used in stage IV of the disease. Currently, the most commonly used type is the ball and socket prosthesis. The use of non-cemented prostheses has been recommended in middle-aged subjects.6 One of the main drawbacks of this technique, particularly in the case of non-cemented implants, has been the possibility of loosening, especially of the trapezial component. However, recent works have reported good survival results with no aseptic loosening in cemented prostheses.7 Other complications reported were dislocation, intraoperative fracture of the metacarpal when introducing the stem and fracture of the trapezium. Prosthetic replacement is contraindicated in cases of young patients with professional activities requiring lifting heavy weights, cases with scarce bone stock and overly flattened trapezia.8
There are currently very few studies establishing the superiority of one treatment over another.
The objectives of this study were to evaluate the clinical results of patients suffering TMC osteoarthritis treated with resection-suspension arthroplasty techniques and total TMC prosthesis, as well as comparing these techniques to verify the existence of significant differences.
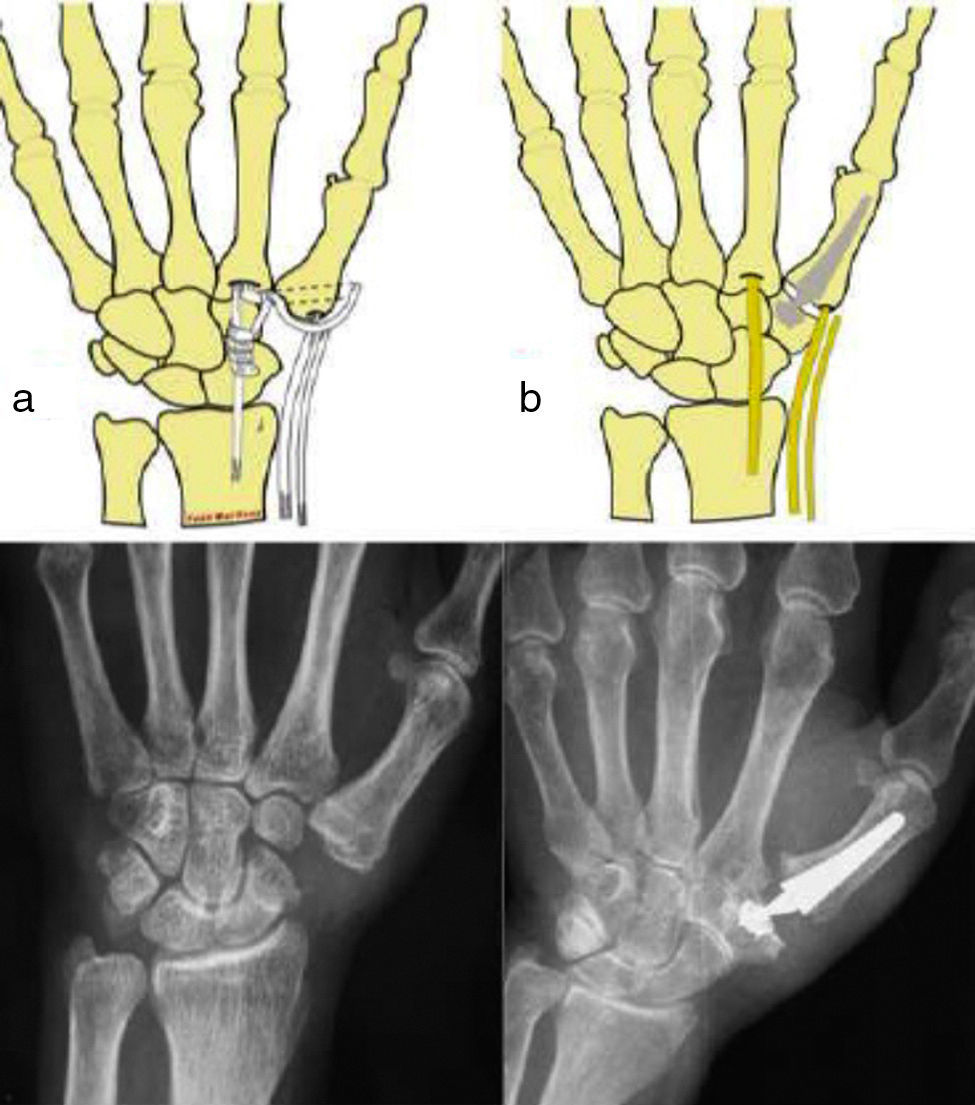
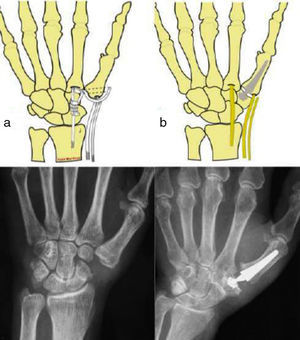
Material and methodWe present a prospective study of 30 cases intervened due to symptomatic TMC osteoarthritis through 2 different techniques: resection-suspension arthroplasty and total TMC prosthesis (Fig. 1), between June 2010 and July 2011. All the patients included in the study attended the respective clinics consecutively and were diagnosed with symptomatic and disabling thumb rhizarthrosis (pain in the base of the thumb interfering with daily life activities, positive grind-test and radiographic signs of trapeziometacarpal osteoarthritis) and proposed for surgical treatment following failure of conservative therapies. The exclusion criteria included: TMC osteoarthritis stage IV in the Eaton–Glickel classification, severe dysplasia of the trapezium, rigid and irreducible deformity of the MCP and young patients with professions requiring significant physical effort and manual lifting of heavy weights, as treatment with prostheses is controversial in all such cases. Moreover, patients with TMC osteoarthritis stage I in the Eaton–Glickel classification were also excluded.
The following 2 study groups were established:
- •
Group 1: resection-suspension arthroplasty with FCR, with 15 intervened patients.
- •
Group 2: total TMC prosthesis (Arpe Biomet model), with 15 intervened patients.
Patients in group 1 were obtained from Hospital Virgen de la Arrixaca, in Murcia, whilst those in group 2 came from Hospital Clínico Universitario, in Valladolid. All agreed to take part in the study and the research work was approved by an Ethics Committee.
The 2 groups were intervened by hand surgeons with over 10 years of experience. The same inclusion criteria and data collection protocol were employed in both groups. Patients who missed any of the review appointments were excluded from the study.
The mean age in group 1 was 58.25 years (range: 51–68 years), and that in group 2 was 61 years (range: 52–72 years). The mean age of the entire series was 59.61 years (range: 46–72 years). The predominant gender was female (91.6%). The total percentage of dominant hands intervened was 53.84%. The most frequent profession among patients in both groups was housekeeping (58.9%). In total, 50% of group 1 and 46.6% of group 2 presented an associated pathology. The most frequent associated disease in all series was carpal tunnel syndrome (25.6%). All the variables listed below were assessed preoperatively and 3, 6 and 12 months after the intervention.
Pain at rest, during activity and at the end of the day were assessed in all patients, based on a visual analogue scale (VAS), considering 0 as an absence of pain and 10 as the maximum pain possible. Patients also filled out the DASH (Disabilities of the Arm, Shoulder and Hand) questionnaire, which measures the general increase in quality of life following surgical treatment in the upper limbs. We also assessed the personal satisfaction of each patient through 2 questions: “How would you describe the result of the treatment received?” With the possible results being “excellent”, “good”, “average” and “poor”; and “Would you undergo an operation with this surgical technique again?” With the possible answers being “yes” and “no”.
As objective parameters we evaluated fist strength through a certified hand dynamometer (Jamar Hand Dynamometer, Sammons Preston, Rolyan, Chicago, USA) and terminoterminal and lateroterminal pinch strength using a specific hydraulic pinch dynamometer (B&L Engineering Pinch Gauge, Santa Ana, CA, USA). In both cases, strength was expressed in kg. We measured joint balance in adduction–abduction and in anteposition–retroposition, using a specific hand goniometer which recorded the amplitude in degrees, as well as opposition by means of the Kapandji test,9 which assigns scores from 0 to 10 according to the point of the hand reached with the thumb.
The surgical approach employed in both techniques was the posterolateral. Group 1 underwent full trapeziectomy using a hemitendon from the FCR for the repair, introduced through a transosseous tunnel created in the base of the metacarpal and subsequently knotted in place; the remaining plasty was then interposed surrounding the FCR tendon. In group 2, we placed a model Arpe (Biomet Spain Orthopedics S.L., Valencia, Spain) total TMC prosthesis after resection of the facet joints of the first metacarpal and the trapezium, sectioning the base of the metacarpal from a dorsoradial point at an angle of 45° in the horizontal plane and, in the trapezium, only the peripheral osteophytes were resected. The postoperative protocol was the same for the 2 groups and consisted in placing a short palmar plaster cast to immobilise the column of the thumb for 2–3 weeks. Upon removal, patients were advised to start ante–retroposition, abduction–adduction and thumb opposition exercises. Patients who did not regain mobility at an early stage were referred to the Rehabilitation Service.
ResultsVAS score (Table 1)The mean scores obtained in the VAS scale at rest in group 1 were: 6.33 (preoperative); 3.58 (3 months postoperative); 2.75 (6 months postoperative); 0.83 (12 months postoperative). The mean scores obtained during effort were: 8.33 (preoperative); 5.75 (3 months postoperative); 4.17 (6 months postoperative); 1.75 (12 months postoperative). The mean scores at the end of the day were: 7.92 (preoperative); 4.75 (3 months postoperative); 3.75 (6 months postoperative); 1.25 (12 months postoperative). Therefore, a progressive decrease until 12 months after the intervention was obtained in the mean VAS scale score at rest, during effort and at the end of the day, and these results were statistically significant. The reduction in the VAS scale score was of 86.88% at rest, 78.99% during effort and 84.21% at the end of the day (Table 1).
DASH (Disabilities of the Arm, Shoulder and Hand) questionnaire values.
| DASH | Group 1 | Group 2 | ||
|---|---|---|---|---|
| Mean score | Significance level (P) | Mean score | Significance level (P) | |
| Preoperative | 63.61 | <0.0005 | 58.72 | <0.0005 |
| 3 months | 40.63 | <0.0005 | 16.25 | <0.0005 |
| 6 months | 29.24 | <0.0005 | 12.91 | <0.0005 |
| 12 months | 17.36 | <0.0005 | 11.44 | <0.0005 |
| Percentage of reduction (%) | 74 | 80.52 | ||
Significance level P compared to initial value.
The mean VAS scale scores obtained at rest in group 2 were: 7.67 (preoperative); 1.20 (3 months postoperative); 0.87 (6 months postoperative); 0.80 (12 months postoperative). The mean scores obtained during effort were: 8.33 (preoperative); 2.00 (3 months postoperative); 1.27 (6 months postoperative); 1.27 (12 months postoperative). The mean scores at the end of the day were: 8.13 (preoperative); 1.87 (3 months postoperative); 1.20 (6 months postoperative); 1.13 (12 months postoperative). Therefore, a progressive decrease until 12 months after the intervention was obtained in the mean VAS scale score at rest, during effort and at the end of the day, and these results were statistically significant. The reduction in the VAS scale score was of 89.57% at rest, 84.75% during effort and 86.10% at the end of the day.
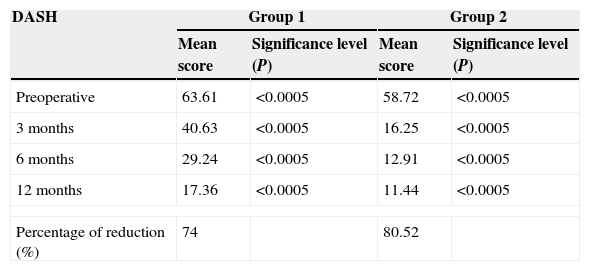
DASH (Table 1)In group 1, the assessment of the DASH questionnaire showed a statistically significant lineal decrease from 3 to 12 months, obtaining a reduction of 74% with respect to the preoperative value. Group 2 showed a statistically significant lineal decrease from 3 to 12 months, obtaining a decrease of 80.52% with respect to the preoperative value.
Patient satisfactionIn group 1, 91.6% of patients reported being satisfied with the treatment received. Up to 66.6% described their situation as excellent, 25% as good and 8.3% as average (none described it as poor). In group 2, 100% of patients reported being satisfied with the treatment received. Up to 77.33% described their situation as excellent and 26.66% as good (none described it as average or poor).
Fist grip, terminoterminal pinch and lateroterminal pinch strengthIn group 1, the mean values for fist grip strength were: 17.18 (preoperative); 14.77 (3 months postoperative); 17.42 (6 months postoperative); 20.20 (12 months postoperative). Therefore, this group presented a statistically significant increase (overall increase of 17.58% after 12 months); however, a significant loss of strength, of 14.03%, was experienced after 3 months, which later improved after 6 months.
The same occurred with terminoterminal and lateroterminal pinch strength, with mean values for terminoterminal pinch strength of 3.12 (preoperative); 2.26 (3 months postoperative); 3.37 (6 months postoperative); 4.19 (12 months postoperative), whilst lateroterminal pinch strength values were 4.31 (preoperative); 3.17 (3 months postoperative); 4.17 (6 months postoperative); 5.32 (12 months postoperative). Therefore, this group presented a statistically significant improvement of 34.29% and 23.43%, respectively, with respect to the preoperative condition.
In group 2, the mean fist grip strength values were: 19.13 (preoperative); 22.00 (3 months postoperative); 22.47 (6 months postoperative); 23.47 (12 months postoperative). Therefore, this group presented a statistically significant increase (overall increase of 22.65% after 12 months); this gain was already observed after 3 months.
The same situation occurred with terminoterminal and lateroterminal pinch strength. The mean values of terminoterminal pinch strength were: 3.67 (preoperative); 5.07 (3 months postoperative); 5.42 (6 months postoperative); 5.83 (12 months postoperative), whilst the values for lateroterminal pinch strength were: 4.78 (preoperative); 6.11 (3 months postoperative); 6.80 (6 months postoperative); 7.03 (12 months postoperative). Therefore, this group presented a statistically significant improvement of 58.81% and 47.13%, respectively, with respect to the preoperative condition.
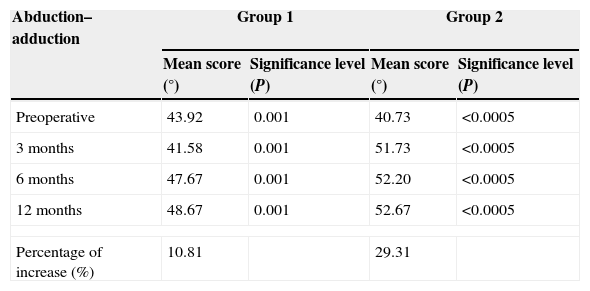
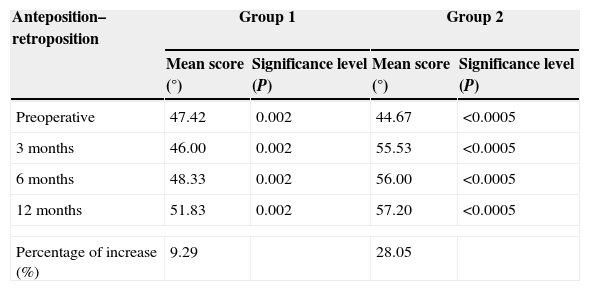
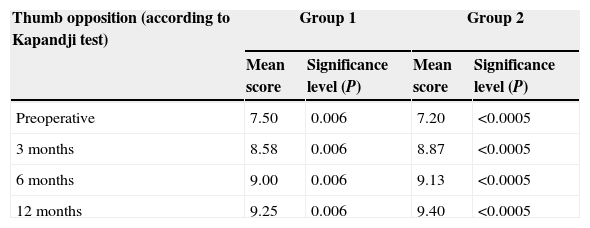
Joint balance (Tables 2–4)In group 1, joint balance in adduction–abduction and in anteposition–retroposition evolved in a similar manner to strength, reaching a balance of 4.75 and 4.46°, respectively, which represented a statistically significant improvement over the preoperative results. This meant a gain of 10.81% in adduction–abduction and 9.29% in anteposition–retroposition. It also meant a statistically significant gain in opposition of 1.75 points (Tables 2–4).
Abduction–adduction balance.
| Abduction–adduction | Group 1 | Group 2 | ||
|---|---|---|---|---|
| Mean score (°) | Significance level (P) | Mean score (°) | Significance level (P) | |
| Preoperative | 43.92 | 0.001 | 40.73 | <0.0005 |
| 3 months | 41.58 | 0.001 | 51.73 | <0.0005 |
| 6 months | 47.67 | 0.001 | 52.20 | <0.0005 |
| 12 months | 48.67 | 0.001 | 52.67 | <0.0005 |
| Percentage of increase (%) | 10.81 | 29.31 | ||
Significance level P compared to initial value.
Anteposition–retroposition balance.
| Anteposition–retroposition | Group 1 | Group 2 | ||
|---|---|---|---|---|
| Mean score (°) | Significance level (P) | Mean score (°) | Significance level (P) | |
| Preoperative | 47.42 | 0.002 | 44.67 | <0.0005 |
| 3 months | 46.00 | 0.002 | 55.53 | <0.0005 |
| 6 months | 48.33 | 0.002 | 56.00 | <0.0005 |
| 12 months | 51.83 | 0.002 | 57.20 | <0.0005 |
| Percentage of increase (%) | 9.29 | 28.05 | ||
Significance level P compared to initial value.
Thumb opposition balance.
| Thumb opposition (according to Kapandji test) | Group 1 | Group 2 | ||
|---|---|---|---|---|
| Mean score | Significance level (P) | Mean score | Significance level (P) | |
| Preoperative | 7.50 | 0.006 | 7.20 | <0.0005 |
| 3 months | 8.58 | 0.006 | 8.87 | <0.0005 |
| 6 months | 9.00 | 0.006 | 9.13 | <0.0005 |
| 12 months | 9.25 | 0.006 | 9.40 | <0.0005 |
Significance level P compared to initial value.
In group 2, joint balance in adduction–abduction and in anteposition–retroposition evolved in a similar manner to strength (rapid increase after 3 months), reaching a balance of 12.04 and 13.53°, respectively, which represented a statistically significant improvement over the preoperative results. This meant a gain of 29.31% in adduction–abduction and 28.05% in anteposition–retroposition. It also meant a statistically significant gain in opposition of 2.20 points.
ComplicationsComplications in group 1, were 1 case of dysesthesia of the sensory branch of the radial nerve (remitted at 6 months after treatment with pregabalin), 1 case of superficial infection of the surgical wound (resolved with oral antibiotic treatment) and 1 case of type I complex regional pain syndrome (received rehabilitation treatment, oral corticosteroids and calcitonin).
Complications in group 2, were 1 case of dysesthesia of the sensory branch of the radial nerve (remitted at 3 months after treatment with pregabalin), 1 case of adverse reaction to stitches (resolved after removing suture) and 1 case of intraoperative trapezial fissure (immobilisation for 5 weeks and not associated with worse results).
Comparison between the 2 techniquesGroup 2 achieved a reduction of over 1 point in VAS scale scores in all 3 categories, which was statistically significant on the third (P<0.0005) and sixth (P=0.004) months. However, after 12 months the VAS scale score showed a similar result between both groups, without statistically significant differences.
In terms of the score registered in the DASH questionnaire at 12 months, group 2 obtained a better score, with no statistically significant differences.
At the end of the follow-up period, group 2 presented a higher grip strength score, with no statistically significant differences. Regarding terminoterminal and lateroterminal pinch strength, group 2 showed higher values in all stages of the monitoring period, with statistically significant differences (P<0.0005).
Joint balance in adduction–abduction and anteposition–retroposition increased in group 2 in all 3 stages of the postoperative monitoring period, with statistically significant differences (P<0.0005). Opposition increased in all 3 periods, with no statistically significant differences.
DiscussionSurgical treatment of thumb rhizarthrosis has more problems and greater variability in stages II and III, due to the large amount of existing surgical techniques. The decision about which technique to employ is based on both objective (age, stage of the joint lesion and level of activity of the patient) and subjective factors (technical ability and experience of the surgeon). Vermeulen et al.10 concluded that the lack of scientific evidence about the superiority and benefits of a specific treatment made personal experience and the preference of each surgeon the basis for selecting one technique or another.
All resection arthroplasties are based on the simple trapeziectomy technique originally described by Gervis,11 which obtained good results in terms of pain reduction, but caused problems related to instability and proximal metacarpal migration. Froimson12 was the first to report tissue interposition to avoid this migration.
Resection–suspension–interposition arthroplasty is the most common surgical treatment in the literature,13–20 and adds different suspension techniques to avoid instability and proximal metacarpal migration. According to the literature, the most commonly used tendon as a hemitendon is the FCR, with no reports of adverse consequences for wrist biomechanics.13,14,18,19,21 Several authors, like Thompson and others,15,22 have used APL tendon arguing ease of extraction, decrease in dorsoradial subluxating force and preservation of the FCR as a wrist stabiliser. Rab et al.,23 compared the use of FCR versus APL tendon and obtained similar results in terms of pain, DASH score and mobility, but higher scores for fist and pinch strength. In addition, the technique employing APL tendon was reported to be simpler. On the other hand, Tomaino24 did not find any differences in the use of these 2 tendons. In our case, we employed FCR hemitendon extracted through an arthroscopy clamp and wire, which facilitated the process and minimised the risks derived from plasty extraction. We did not observe any adverse effects on fist or pinch strength. We examined ligament reconstruction techniques (Burton and Pellegrini,13 Eaton and Littler,14 Thompson,22 Scheker18) through transosseous tunnels and others which only aimed to carry out metacarpal suspension. We did not use a modification of the arthroplasty techniques described by Burton, Pellegrini and Scheker, using a single oblique tunnel from distal–radial to ulnar–proximal.
Another widely used technique is total trapeziometacarpal prosthesis. The ball and socket prosthesis has become widely accepted as the standard prosthetic replacement. The most commonly used and studied model in the literature is the cemented and constrained De La Caffiniere prosthesis. We used the Biomet Arpe model prosthesis, a non-cemented and non-constrained model, which is associated with excellent clinical and radiographic results in the literature, as well as long-term survival.8 We applied some modifications8 to the surgical technique, such as an upper posteroexternal access route, an oblique osteotomy at 45° in the base of the metacarpal without resection in the radial side, resection of osteophytes around the trapezium with no osteotomy and use of a tilted neck.
In our series, the 2 treatments achieved statistically significant improvements in pain 3 months after the intervention. Although the fastest reduction was obtained in the prosthesis group, after 12 months there were no significant differences. Ulrich-Vinter et al.25 obtained statistically significant results when comparing patients treated with an Elektra prosthesis and resection-suspension arthroplasty with APL. These results differ from ours, but confirm the fast improvement in the prosthesis group. However, Santos et al.26 did not find significant differences in terms of pain at 2 years when comparing the resection-suspension arthroplasty and prosthesis techniques. DASH scores in the prosthesis and resection-suspension arthroplasty groups showed no significant differences with each other and were comparable to the best results found in the literature, which ranged between 13.3 and 17.7.8 There were significant differences when comparing them with the resection-interposition arthroplasty group, although the score in this group was comparable to many other series, both of trapeziectomies 19 and prosthesis.27 When comparing our preoperative results with the strength scores of healthy patients reported by Lorenzo Agudo et al.,28 we observed that the greatest loss of strength in patients with thumb rhizarthrosis took place in lateroterminal pinch strength (loss of around 50%), followed by terminoterminal pinch strength values (approximate loss of 40%), and lastly in fist grip strength (loss between 20% and 30%). The majority of treatments achieved an increase in fist grip,25 terminoterminal pinch19 and lateroterminal pinch19 strength. The greatest increase in strength in our series was registered in the prosthesis group. Some studies did not find significant differences when comparing fist grip and pinch strength between suspension arthroplasty and total prostheses.26 Ulrich-Vinter et al. observed significant differences when comparing fist grip and pinch strength between total prostheses and suspension arthroplasty with APL tendon.25 As reported in various studies, we observed a decrease in strength during the first 3 months, with a subsequent and progressive increase in the groups of resection arthroplasties.13 However, this was not the case among those patients treated by total prosthesis, where the increase was evident after the first 3 months. Mobility also presented considerable variations between series in the literature due to several factors, like the different existing terminology. For this reason, we believe it necessary to establish a homogenous nomenclature, as done by the International Federation of Societies for Surgery of the Hand (ISSFH).29 The majority of studies, including our series, achieved an increase in mobility, to a greater or lesser extent.17
Wajon et al.,30 Vermeulen et al.10 and De Smet et al.31 carried out systematic reviews with a high statistical power in which they compared the majority of surgical treatments available and concluded that no surgical treatment was superior to the rest. Vermeulen et al.,10 like Jager et al.,32 observed better short-term results among groups treated with total prosthesis versus groups treated by resection arthroplasty, but were unable to conclude that one treatment was superior to the other due to the scarce number of comparative studies. Adequate patient selection and experience of the surgeon are crucial when indicating surgical treatment.
This study has concluded that both the resection-suspension arthroplasty technique with FCR and the Arpe total prosthesis achieve a statistically significant improvement in the parameters of pain, DASH scale score, fist grip and pinch strength and mobility compared to the preoperative period. Resection-suspension arthroplasty with FCR registered a loss of strength and mobility after 3 months, with clinical improvement 6 months after the intervention, whilst the Arpe TMC total prosthesis presented early clinical improvement with no loss of strength or mobility and reached higher absolute values for postoperative pinch strength and mobility.
As limitations of the study we highlight that both groups had few patients, operations were carried out by different surgeons and the monitoring period of 12 months was too short to reveal certain complications associated to implants, such as loosening, dislocation, collapse and wear.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data.
Right to privacy and informed consentThe authors declare that this work does not reflect any patient data.
Conflict of interestThe authors have no conflict of interests to declare.
Please cite this article as: Martínez-Martínez F, García-Hortelano S, García-Paños JP, Moreno-Fernández JM, Martín-Ferrero MÁ. Estudio clínico comparativo de 2 técnicas quirúrgicas de rizartrosis del pulgar. Rev Esp Cir Ortop Traumatol. 2015;60:59–66.