Arthroscopic repair of rotator cuff disorders is a technically demanding but successful procedure. Many anchor and suture alternatives are now available. The choice of the implant by the surgeon is less important than the configuration of the suture used to fix the tendon, however it is necessary to know if there are differences in the results, using each one of them.
The aim of the study is to evaluate if there are differences between the knotted and non-knotted implant in terms of functional and satisfaction results.
Material and methodsA retrospective study was carried out on 83 patients operated between 2010 and 2014 in our center using 2 anchoring systems with and without knotting (39 versus 44 patients respectively), with single row in complete rupture of the rotator cuff.
ResultsAt the end of the follow-up, an average score was obtained on the Constant scale of 74.6 points. 98% of the patients considered the result of the surgery satisfactory. Statistically, there were no significant differences between the 2 groups in terms of functionality, satisfaction or reincorporation to activities.
Discussion and conclusionsThe functional results of the single-row cuff suture are satisfactory, although biomechanical studies show advantages in favor of sutures that reproduce a transoseo system. It our series of patients the presence of knotting does not show per se a significant functional difference being both superimposable techniques in absolute values of functionality and patient satisfaction.
La reparación artroscópica de los trastornos del manguito rotador es un procedimiento técnicamente exigente pero exitoso. En la actualidad hay disponibles muchas alternativas de anclas y suturas. La elección del implante por parte del cirujano es menos importante que la configuración de la sutura usada para fijar el tendón, no obstante hay que conocer si existen diferencias en cuanto a los resultados, utilizando cada uno de ellos.
El objetivo del estudio es valorar si existen diferencias entre el implante anudado y no anudado en cuanto a resultados funcionales y de satisfacción.
Material y métodosSe realiza un estudio retrospectivo en 83 pacientes intervenidos entre 2010 y 2014 en nuestro centro mediante 2 sistemas de anclaje con y sin anudado (39 frente a 44 pacientes respectivamente), con hilera simple en rotura completa de manguito rotador.
ResultadosUna vez finalizado el seguimiento, se consiguió una puntuación media en la escala de Constant de 74,6. Un 98% de los pacientes, consideraron el resultado de la cirugía como satisfactorio. A nivel estadístico no hubo diferencias significativas entre ambos grupos en parámetros de funcionalidad, satisfacción ni reincorporación a actividades.
Discusión y conclusionesLos resultados funcionales de la sutura de manguito mediante hilera simple son satisfactorios, aunque estudios biomecánicos muestran ventajas a favor de suturas que reproducen un sistema transóseo. En nuestra serie de pacientes la presencia de anudado no muestra per se una diferencia funcional significativa siendo ambas técnicas superponibles en valores absolutos de funcionalidad y satisfacción de los pacientes.
The incidence of shoulder pain in the general population stands at around 4%1 and it is often associated with rotator cuff disorders, especially in older adults. The incidence of rotator cuff lesions found in cadaveric studies varies from 7%2 to 20%,3 and it reaches up to 30%4 if partial thickness lesions are included. In patients with degenerative or inflammatory tendon pathologies of the cuff the treatment of choice is conservative, although if tendon continuity solutions exist in symptomatic patients then surgical treatment should be considered.
Tearing of the rotator cuff is among the most common diseases at the level of the shoulder blades, and it is a growing problem in the population aged over 50 years old. The aims of treating these lesions are to eliminate pain, restore functioning and preserving biomechanical properties to prevent the progression of arthropathology and the resulting rise of the humeral head.
The results of treating these lesions using arthroscopic techniques are good to excellent in the majority of cases.5–8 Arthroscopic techniques have been shown to be less invasive, while they make it possible to preserve the insertion of the deltoids and require less soft tissue dissection.9 The ideal repair should be as anatomical as possible, with a strong initial anchorage while reducing the formation of gaps during the tendon integration process in the bone. Although single row suture technique is considered to be the standard in treating these lesions, a double row reproduces a mechanically superior structure (in terms of strength and rigidity). When their functional results were compared in recent randomized studies and different meta-analyses, both methods were found to be similar.10–12
Single row cuff sutures have also been studied to compare knotted vs. non-knotted implants. These studies show that non-knotted techniques give superior biomechanical results.13
Given our experience in single row cuff sutures and the proven theoretical biomechanical superiority of knotless implants, we propose a study to compare the clinical results and patient satisfaction when 2 different anchoring systems are used (knotted and knotless).
Material and methodsA retrospective study was undertaken of 2 cohorts of patients in which 2 different systems supraspinatus suture systems had been used, knotted or knotless. The cohorts were formed from February 2010 to October 2014 in our health catchment area; the type of implant to be used was determined by the surgeon consecutively, according to his experience. Irreparable tears were excluded, as were cases of cuff arthropathology and those subjects who failed to complete the rehabilitation and follow-up protocol. Clinical evaluation was undertaken by surgeons with more than 8 years’ experience in arthroscopic shoulder surgery. Before surgery the patients were evaluated for the existence of pain, Neer's pain arc, the lift off test and Hawkins’ sign, as well as the presence of a pseudoparalytic shoulder. The Constant test was applied after the operation; abduction values, external and internal rotation with the arm extended and at 90° and strength in comparison with the other arm using Constant test criteria, with 2.27 points per kilogram of weight raised. At the end of the follow-up patients were evaluated for return to work and sports activity, as well as for the presence of complications.
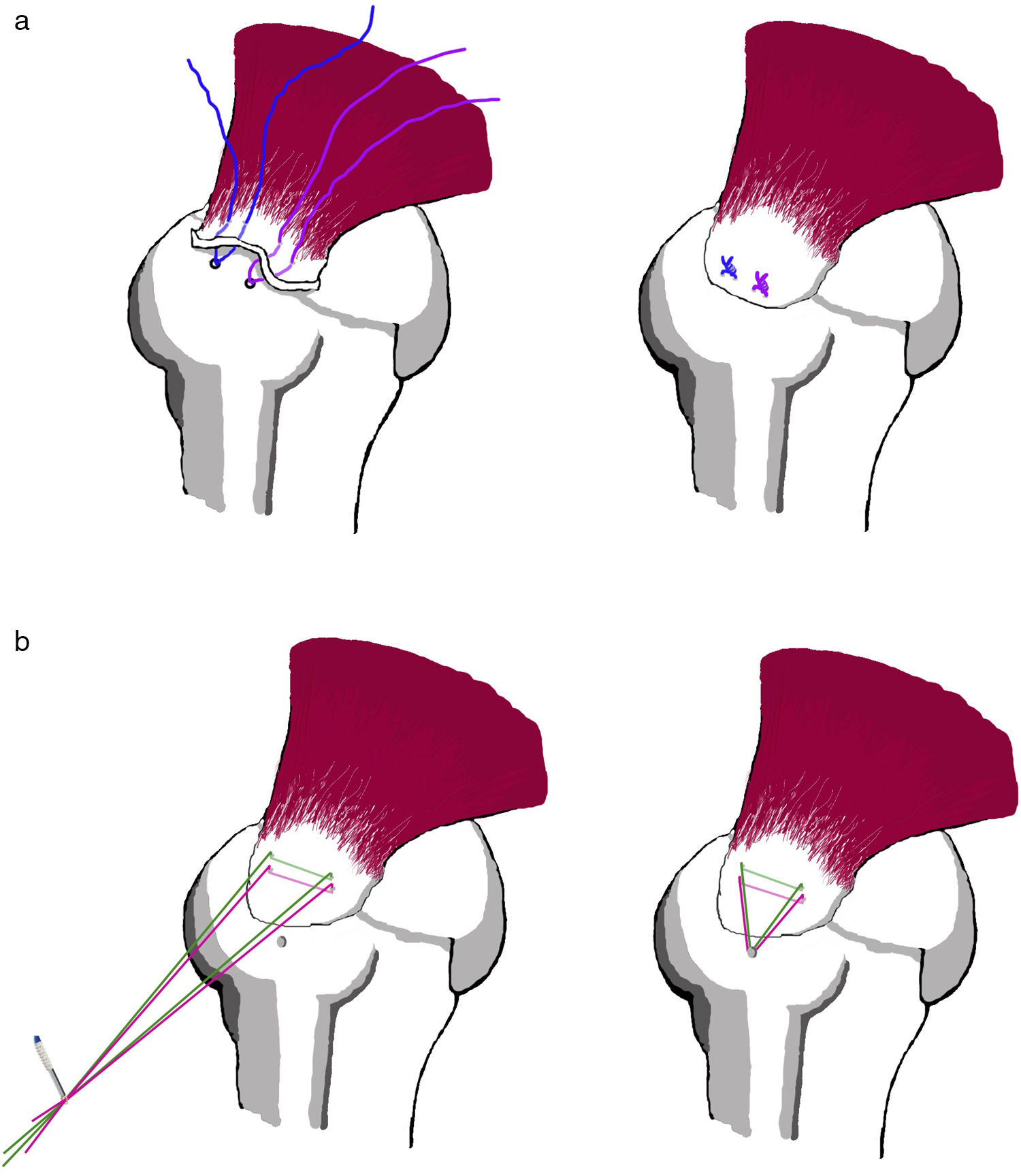
Surgery took place with the patient in lateral decubitus. In the first phase the joints were examined and the biceps was observed, evaluating the grade of tendon pathology, if any, using Hedtman's scale1 that includes partial lesions of the long part of the biceps and instability/subluxation in degrees II and III. The joint was also evaluated to identify the presence of glenohumeral arthropathology. If grade II or III biceps tendon pathology was found in patients over the age of 50 years old, biceps tenotomy was performed. Debridement was performed in those younger than 50 years old. During subacromial exposure the decision was made to perform acromioplasty and bursectomy, the tear was identified and debrided, and an abrasion was made at the level of the greater tuberosity in the supraspinatus tendon insertion mark. At this moment the surgeon decided which type of implant to use. The group of knotted sutures included the Truepass® passer (Smith and Newphew® Ref: 72203791) with implants such as the 3.5mm Twinfix® (Smith and Newphew® Ref: 72203784) and single row knotted suture. In the case of knotless sutures, the FastPass Scorpion® passer was used (Arthrex® Ref: AR-13997SF) with a Fibertape® suture system (Arthrex® Ref: AR-7237), using the 4.75mm SwiveLock® type implant (Arthrex® Ref: AR-2324BCC) with a titanium tip. The positioning and number of implants were decided by the surgeon during the operation.
Immediately after the operation a Velpeau-type sling was fitted, and the arm was allowed to hang free after the first week following surgery. In general rehabilitation commenced according to the protocol of the said department. Passive assisted movement in the scapular plane commenced after the third week and continued in the sixth week with assisted passive exercises without limitation, depending on the tolerance, as well as active assisted exercises and scapular mobility. Abduction and gaining strength in external rotation were delayed until 8 weeks.
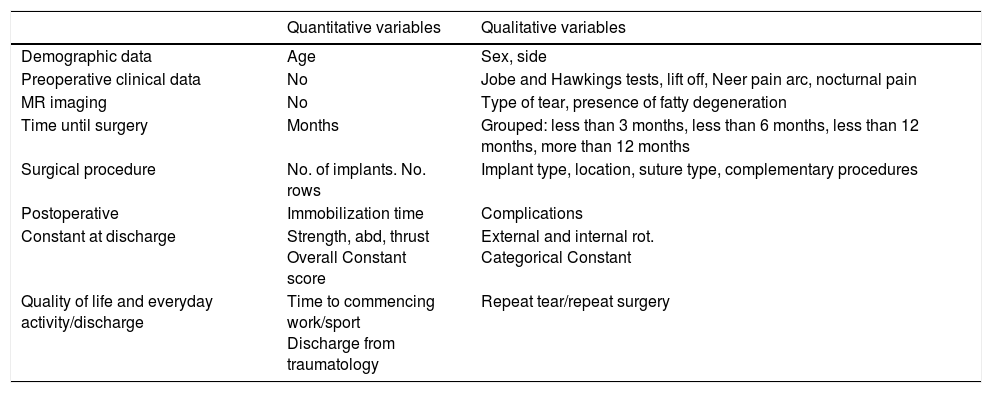
The sample was described statistically in terms of frequencies for qualitative variables and dispersion measurements for quantitative variables. The existence of differences between sociodemographic parameters and the type of tear and symptoms was evaluated, while differences between the groups in the other qualitative variables were evaluated using the chi-squared test or Fisher's exact test for qualitative variables, with the independent variable of the type of suture performed. To evaluate the differences in functional parameters the differences between averages were analyzed using Student's t-test and, secondly, by grouping the functional tests into categories before evaluating them using the chi-squared test respecting the suture. Previously the normality of patient distribution had been evaluated respecting age, time delay to surgery and the Constant scale according to the Shapiro–Wilk test (P>.05), which allowed us to apply parametric tests for statistical analysis. Table 1 contains a summary of the variables. The statistical package SPSS 15.0 was used for this analysis, and the general level of significance was P<.05.
Summary of the variables studied.
| Quantitative variables | Qualitative variables | |
|---|---|---|
| Demographic data | Age | Sex, side |
| Preoperative clinical data | No | Jobe and Hawkings tests, lift off, Neer pain arc, nocturnal pain |
| MR imaging | No | Type of tear, presence of fatty degeneration |
| Time until surgery | Months | Grouped: less than 3 months, less than 6 months, less than 12 months, more than 12 months |
| Surgical procedure | No. of implants. No. rows | Implant type, location, suture type, complementary procedures |
| Postoperative | Immobilization time | Complications |
| Constant at discharge | Strength, abd, thrust Overall Constant score | External and internal rot. Categorical Constant |
| Quality of life and everyday activity/discharge | Time to commencing work/sport Discharge from traumatology | Repeat tear/repeat surgery |
Abd=abduction.
Eighty-three cuff sutures were performed in 81 patients, with 2 bilateral sutures, with single row with a Swivelock® (knotless) suture system in 44 patients, and Twinfix® type in 39 patients. The average age in the Swivelock® group was 64 years old (R=42–81) vs. 63.82 years old (R=42–79) in the Twinfix® group. The distribution according to sex was 59 women and 22 men. No differences in age or sex were found between both groups of patients, where P=.925 for age and .117 for sex.
The most frequent symptoms at diagnosis were pain, at 66.3%, vs. pain and functional impotence at 33.6%. The existence of Neer's painful arc and subacromial irritation (Hawkins’ sign) appeared in a high percentage of patients, at 94% and 96.2%, respectively.
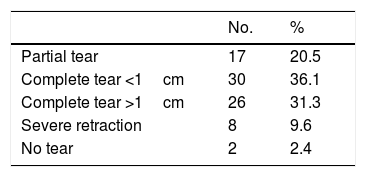
The most frequent MR images were tear of the complete thickness of at least 1cm. 14.5% also showed signs of grade III fatty degeneration. There were no differences between both groups respecting preoperative imaging studies, where P=.212 (Table 2).
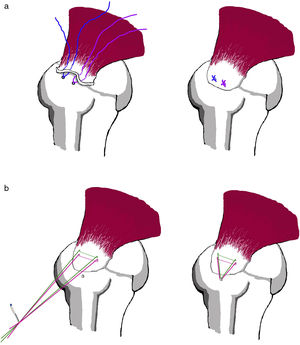
The average delay before surgery was 5.26 months (R=1–24), without differences according to the implant used: P=.523. We found no differences in the number of implants (P=.133) or the number of threads according to the implant (P=.191. A single row suture was performed with the implants over the previous mark, according to surgical protocol (Fig. 1). Acromioplasty and bursectomy were performed jointly as the most common complementary procedure (64/83), while it biceps tenotomy in case of a lesion to the same was less frequent (10/83). No biceps tenodesis was performed. Statistically significant differences were found between the number of biceps tenotomies in both groups, as there were more in the knotless group (P=.007).
The average duration of hospitalization was 1.06 days (R=1–5), without associated complications or readmission. 86.7% of the patients required shoulder immobilization by means of a Velpeau sling during an average of 2.20 weeks, R=1–3 weeks. The average number of weeks of immobilization was higher in the Swivelock® group, at 2.50 weeks (R=2–3) as opposed to the Twinfix® group at 1.87 weeks (R=0–3). This difference was statistically significant, where P=.006.
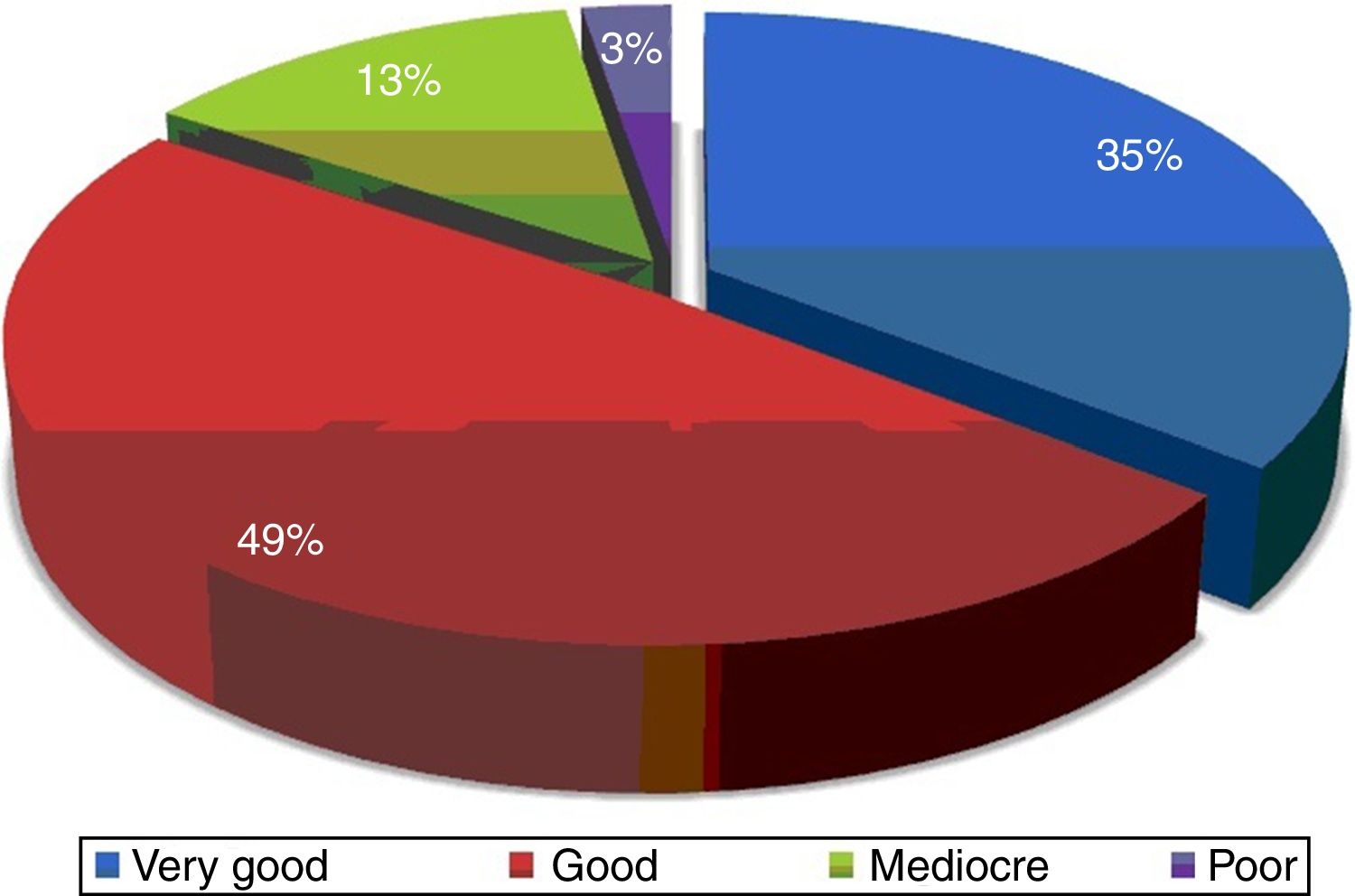
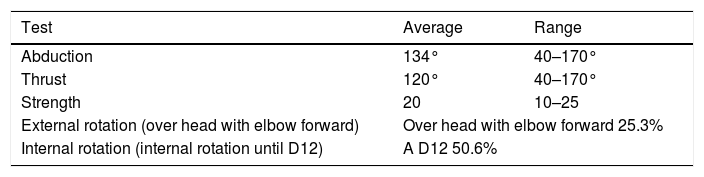
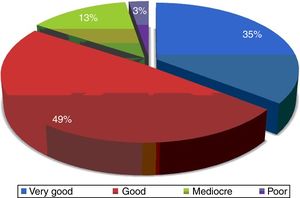
The patients returned to work after an average of 3.71 months (R=1–13 months), and their average score on the Constant scale was 74.6 points (median 77, range 41–98). The follow-up lasted for an average of 7.34 months (R=3–13 months). The patients with complete tear larger than 1cm or retraction were definitively discharged as outpatients significantly later (at 9.03 months vs. 6.73 months, P=.012). A new evaluation of the Constant scale when follow-up as outpatients terminated found no differences in the average Constant scale score (74.6 vs. 74.45, P=.434). From a qualitative point of view 84.3% were considered to be good or very good, in comparison with the 15.7% of results that were mediocre or poor (Fig. 2). A summary of the functional results is shown in Table 3.
MR imaging was used to follow-up those patients with a mediocre or poor result (13/83). A re-tear rate of 23% was found in this group, i.e., 3 patients, without any differences depending on the implant used (P=.546).
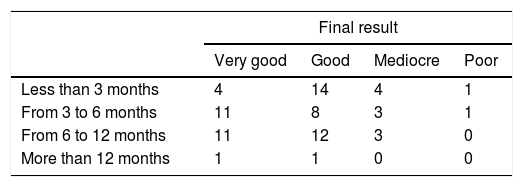
The factors that could modify the functional result in these patients were evaluated. The detection of fatty degeneration in the MR imaging did not modify the final functional state from a quantitative viewpoint (P=.738) or a qualitative viewpoint (P=.566); nor did the presence of retraction have any influence (P=.354). The delay before surgery after the onset of symptoms did not significantly change the functional result (P=.391) (Table 4).
Regarding their return to work and degree of satisfaction, 98% considered the result of surgery to be satisfactory. 50% of the patients returned to work or leisure in the first 3 months after surgery. Only one patient took more than 12 months to return to activity. At the end of follow-up 3 repeat tears of the supraspinatus were identified by ultrasound scan or MR imaging. 2 repeat operations took place, one in case of re-tear and the other for acromioclavicular arthrosis that was subjected to an arthroscopic Mumford procedure.
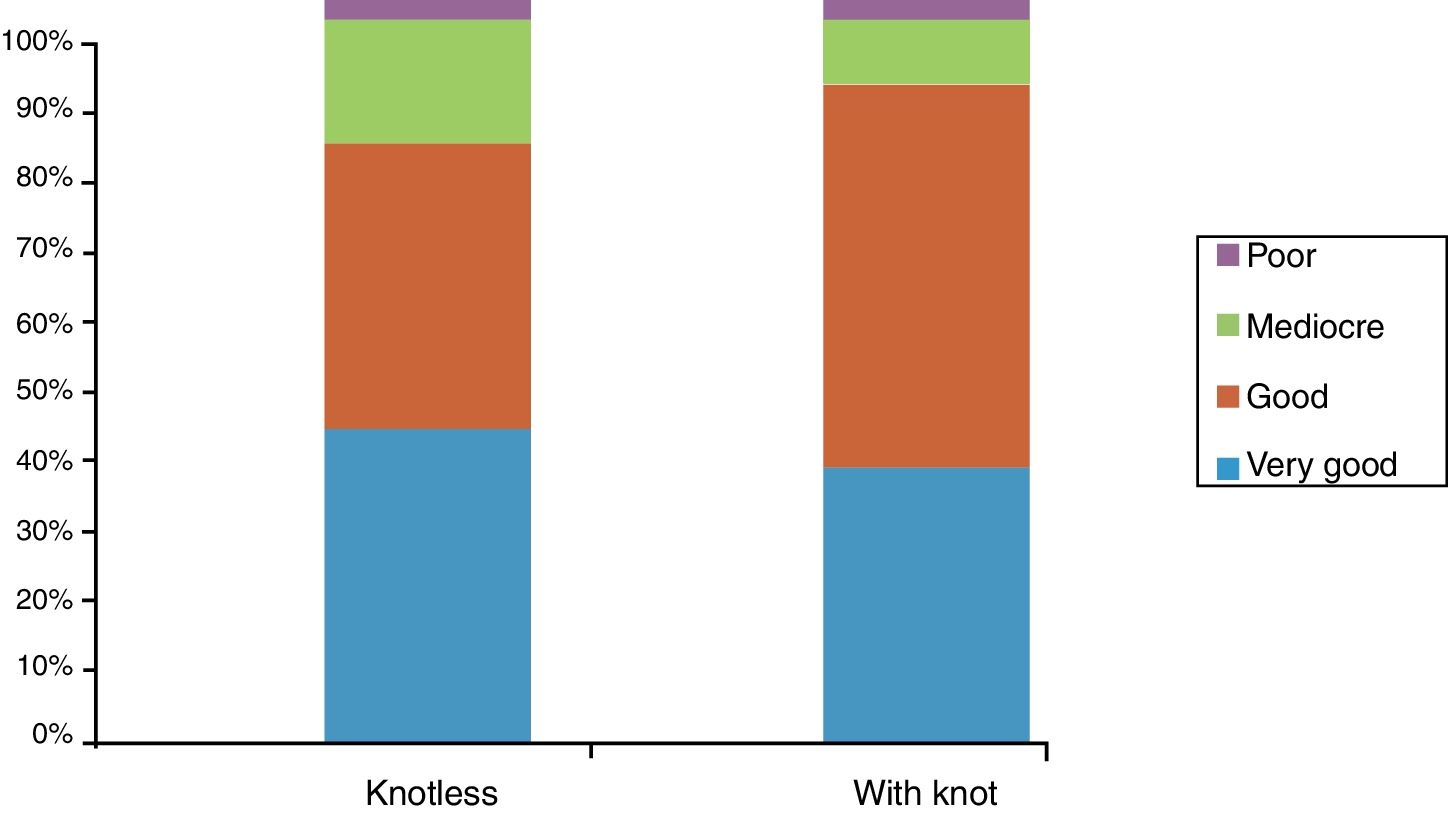
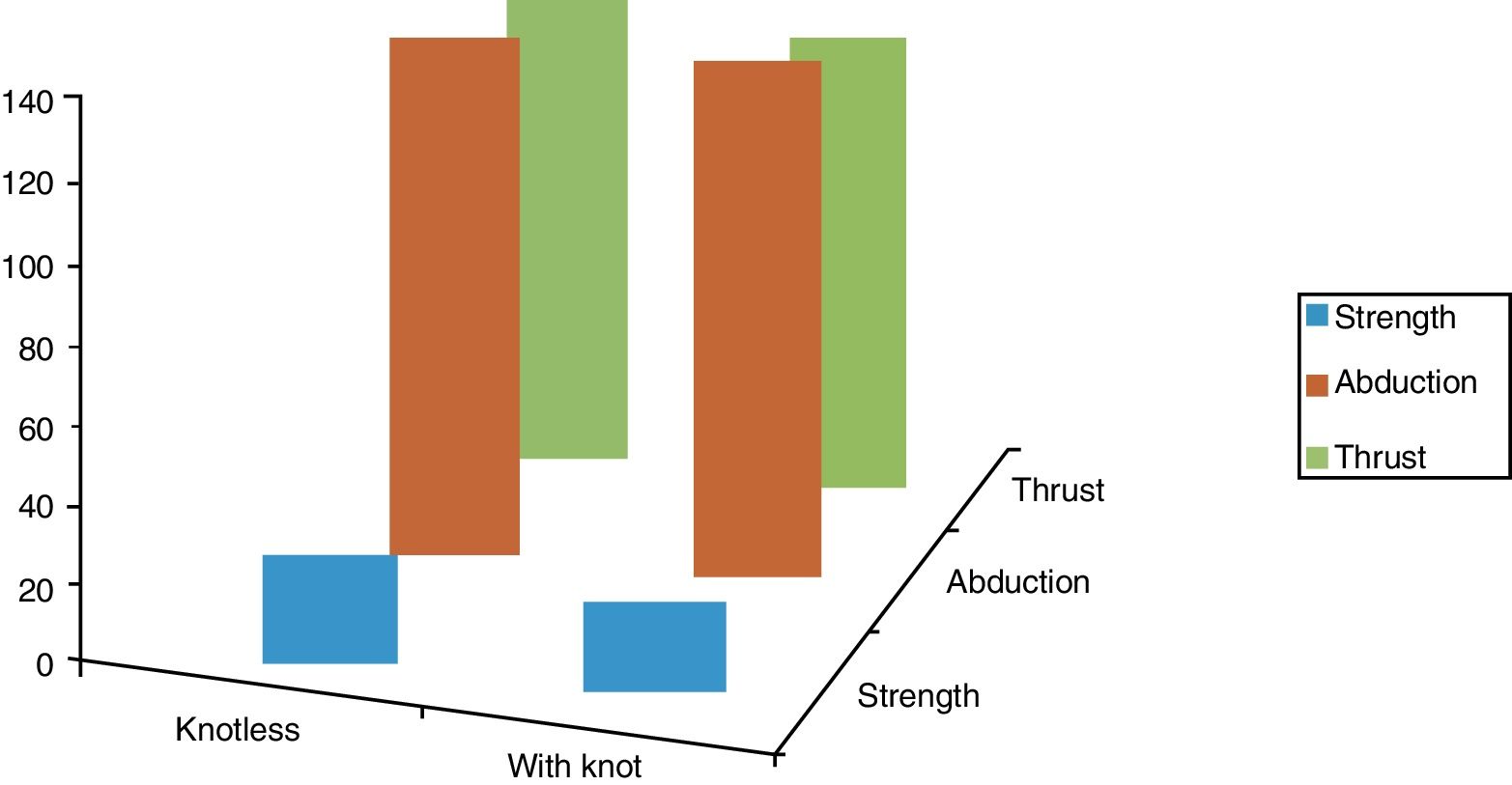
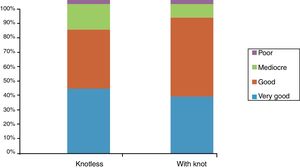
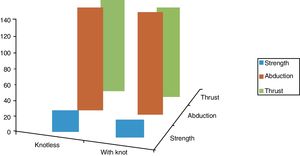
The functional scale averages corresponding to the implants used were compared at the end of follow-up; there were no statistically significant differences between the average Constant scale scores from a quantitative point of view (P=.990). Nor were the differences between the groups statistically significant from a qualitative viewpoint (P=.731) (Fig. 3). No statistically significant differences were found between both groups in arc of movement and strength scores; (P=.724 for abduction, P=.212 for thrust and P=.146 for strength) (Fig. 4).
As we had found difference between the number of tenotomies in the knotless group vs. the knotted group, we evaluated the hypothesis that tenotomy may change the final result. We found no differences in the Constant scale (P=.881) from a quantitative point of view or from a qualitative point of view (P=.713).
The average time to discharge was 3.84 months in the knotless group vs. 3.72 months in the other group, without any significant differences between them (P=.83). Nor did we find any significant differences between both groups in terms of when they restarted work or leisure (P=.498).
DiscussionDuring the last 2 decades surgical treatment of the rotator cuff has changed from open to mini-open, all arthroscopic. The surgical technique has developed from simply debriding massive tears to repairing them.
These advances in surgical technique have been made possible by the explosion in the number of devices and suture materials to affix the tendon to the greater tuberosity; nevertheless, there is a significant incidence of poor results after the introduction of stronger anchors and metallic materials. Failure tends to occur at the suture-tendon interface, as this seems to be the weakest place in the rotator cuff repair process.13 The constant evolution of implants and the range of repair techniques mean that interest will continue to grow in evaluating results over the medium to long terms.
There are now many biomechanical studies of different repair techniques that show the superiority of TOE or double row suture over traditional single row suture.14 Although the double row reproduces a mechanically superior structure (strength and rigidity), comparison of the functional results in recent randomized studies and different meta-analyses still show them to be similar.10,11
Given that in our everyday clinical practice we systematically use a single row of suture, the aim of our study arises from the following possibility: if neither a double nor a single row of suture is functionally superior, we would ask whether one of 2 different anchor systems is better than the other, supposing from the first that they are biomechanically superior in knotless techniques.
This impression is corroborated by papers such as the ones by Carli and the one by Lanceti et al., who in 2012 published an experimental study in a bovine model that compared the biomechanical aspects of 2 techniques similar to those used in our study. They concluded that the SwiveLock® system (Arthrex®) with Fibertape® (Arthrex®) has greater mechanical strength and a lower failure rate compared to a knotted system and Fiberwire (Arthrex®). Additionally, the form of failure is different in both systems, as the contact surface is far greater in Fibertape®, giving it an advantage comparable to that of a transosseous suture. Other studies have emphasized this type of implants to the same degree, fining a biomechanical advantage at all abduction angles vs. a single row suture with a harpoon.15
From a statistical viewpoint our study has two highly homogeneous samples in sociodemographic terms (age, sex, time before suture, MR imaging), the type of surgical procedure and postoperative findings.
We obtained highly satisfactory results with both techniques, achieving high values in the Constant functional scale, with an average above 74 points (median 77) and with a functional arc of movement. These results are similar to those obtained by Burks et al. in their 2009 study, with an average after one year of 77 points in the Constant scale in a single row suture cohort.16 In a subsequent study, Carbonel et al. obtained similar results with the same type of suture row and an average of 79.8 points.17,18 Nevertheless, other authors such as Lapner et al.19 and Koh et al.18 obtained better results in their series, with averages of 86.4 and 85.4 points. However, the former study included a percentage higher than 30% of small lesions that, when logistic regression is applied, are found to be a confusing factor in the results,19 while the latter centers on lesions smaller than 4cm.
There were no significant differences between the groups in terms of the complementary procedures that were performed, except for biceps disease which was found in a form treatable by tenotomy in a higher number of patients in the SwiveLock® (knotless) group.
We detected a short follow-up in some patients in the series, with early discharges for everyday life activities. As the minimum out-patient follow-up was 3 months, to identify possible causes we compared average times of definitive discharge according to the type of tear shown by MR imaging; this showed a significantly shorter average follow-up in patients with partial tears or ones smaller than 1cm in comparison with large complete tears.
Secondarily, more than half of our patients returned to performing the same activities as prior to the tear in less than 3 months, with a higher than 90% satisfaction score and a very low rate of complications. These data are similar to those of the series by Lapner et al., as they obtained good or excellent results in more than 80% of their patients.19
Some studies indicate that the repeat tear rate for single row sutures may surpass the 25% found in series vs. a double row20; in our case we report a repeat tear rate of 3.6% as diagnosed by MR imaging. However, we are unable to rule out a higher number of tears as, if they occurred; they had no functional repercussions in our patients during follow-up.
It can be concluded from our study that both samples are homogeneous in mechanical and functional terms, independently of the implant and suture configuration used. We admit that our study has several important limitations: it is a retrospective study of cohorts; simple functional scales were used in basic evaluation; no evaluation using imaging techniques took place to detect the repeat tear rate, and the sample contained 44 and 39 patients in each group.
Level of evidenceLevel of evidence IV.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments took place in human beings or animals for this research.
Confidentiality of dataThe authors declare that they followed the protocols of their center of work governing the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this paper.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Muniesa-Herrero MP, Torres-Campos A, Urgel-Granados A, Blanco-Llorca JA, Floría-Arnal LJ, Roncal-Boj JC, et al. Comparación de resultados funcionales en 2 sistemas de fijación mediante hilera simple en sutura de manguito rotador. Rev Esp Cir Ortop Traumatol. 2018;62:178–184.