Uncemented hip replacement matches the best results of classic cemented replacements. With the aim of preserving bone and soft tissue, implants with shorter stems and proximal metaphyseal support have been developed. Likewise, the lack of distal load should avoid cortical diaphyseal remodelling phenomena and the thigh pain of some cylindrical and wedge implants. The resurfacing implant, very popular as a conservative hip replacement in the young adult, has disadvantages associated with the fragility of the neck and with large head metal friction torque. Short stem hip replacement may be a reasonable alternative to classic implants and surface hip replacements. The different designs of conservative short stem implants are analysed, and are classified according to their morphology and biomechanical characteristics. Some medium term series show promising results.
La artroplastia de cadera no cementada iguala los mejores resultados de las artroplastias cementadas clásicas. Con el fin de preservar el tejido óseo y las partes blandas, se han desarrollado implantes con vástagos más cortos y con apoyo proximal en la metáfisis. Además, la ausencia de carga distal evitaría los fenómenos de remodelación cortical diafisaria y el dolor de muslo de algunas prótesis de geometría cilíndrica o en cuña. Las prótesis de superficie, muy populares como artroplastia conservadora en el adulto joven, han generado inconvenientes relacionados con la fragilidad del cuello y con el par de fricción metálico de cabeza grande. Las prótesis femorales de vástago corto pueden ser una alternativa ventajosa a las prótesis clásicas y a las artroplastias de superficie. Se analizan los diferentes diseños de prótesis conservadora de vástago corto y se clasifican según su morfología y características biomecánicas. Algunas series, a medio plazo presentan resultados prometedores.
Uncemented hip prostheses have rivalled the best classic cemented prostheses in terms of stability and survival. Femoral implants designed for proximal metaphyseal fixation and coated with porous titanium and hydroxyapatite achieve primary stability and early osseointegration that competes favourably with cemented prostheses that, until recently, were considered the gold standard in hip replacement.1
Recent studies have revealed that 20-year survival rates for total hip replacement are lower with cemented than with uncemented prostheses.2
Uncemented femoral stems are designed with different morphologies and characteristics: cylindrical, conical or wedge-shaped, symmetrical, or anatomical. Proximal metaphyseal-fixed stems appear to give the best results in terms of survival, absence of remodelling phenomena, and absence of thigh pain.1
If we achieve good, proximal primary fixation, we need no diaphyseal stem extension. Immediate stability and good osseointegration may be achieved with a short-stem or stemless femoral prosthesis. A conservative prosthesis spares the femoral neck and takes advantage of the quality and volume of cancellous bone in the metaphysis and trochanteric area for a solid and durable primary fixation.3,4
Short-stem or stemless conservative prostheses were initially proposed as an alternative to classic stems after long-term experience with prostheses with proximal metaphyseal fixation only, where the stem extension has no mechanical function but simply assists with alignment. It has also been shown that avoiding contact between the end of the prosthesis and the diaphyseal cortex is advisable to prevent the thigh pain and remodelling phenomena associated with it. The recent, ongoing debate in numerous publications about complications associated with the design of resurfacing prostheses (fracture of the neck, acetabular loosening) and with the use of metallic friction couples (ALVAL [aseptic lymphocytic vasculitis and associated lesions],5 pseudotumours, increased peripheral blood levels of cobalt and chromium ions)—in short, the current controversy over metallic friction couples6—puts the short prostheses in a position to be the alternative to resurfacing prostheses. In young patients, the preservation of bone on the femoral side would justify this choice. An even more important reason, however, is that resurfacing prostheses have not demonstrated functional results superior to those of a total arthroplasty.7
As with classic femoral prostheses, the various so-called conservative prostheses of today vary in design. We will attempt to describe the different implants in terms of their morphology, their biomechanical characteristics, and the results that have been published, though these are from short- or medium-term series.
However, not all “conservative” prostheses have a stem that is actually short, nor are they all equal in terms of sparing the femoral neck, cancellous bone tissue, and the metaphysis.
Some manufacturers have confined themselves to shortening their classic implants without modifying the design. This could result in inferior prosthesis stability.
The prosthesis is fixed on the femoral neck and preserves it; the stem is implanted in the metaphysis–diaphysis keeping to the neck's trabecular structure (Pipino/CFP model).
Like the Morrey (Mayo conservative) model, the prosthesis is implanted as a wedge in cancellous bone tissue of the metaphysis, with a small distal extension for alignment.
The stemless prosthesis, with proximal circumferential fixation and high neck cut, is modelled after the Santori prototype.
There are prostheses designed for transitioning from a resurfacing prosthesis; these have a subcapital cut and solid hemispherical head and are implanted in the femoral neck axis via a conical, straight, porous-coated stem.
Shortened classic stemsFitmore (Zimmer), SMF (short modular femoral hip) (Smith nephew), taperloc microplasty, and balance microplasty (Biomet) are shorter versions of the previous, classic stems. We do not have published results available for these implants. However, it remains to be confirmed that shortening a stem without changing its profile does not alter primary stability.
Neck-sparing prosthesis fixed on the neckAmong the conservative prostheses available at this time, the oldest concept is the design proposed in 1979 by Pipino under the name biodynamic.8 The CFP™ (collum femoris preserving) stem (link) evolved from Pipino's model. This is a neck-sparing prosthesis with collar fitted to the neck fixation; it is a curved, ribbed, and relatively short stem. There is triplanar loading to achieve rotational stability. It is fixed on the neck and in metaphyseal cancellous bone, obtaining physiological fixation through alignment with the metaphyseal trabeculae, and its distal end lies in the proximal diaphysis.9 This is apparently the most technically demanding segment to handle: fractures of external cortical bone in the proximal femoral diaphysis have been reported. Resorption or rounding off of the femoral neck have also been detected, as well as reinforcement in distal cortical bone with radiographic patterns typical of remodelling.10 It is important to point out that, in uncemented long-stem prostheses, these are the patterns associated with thigh pain. Medium-term results published reflect a high rate of implant survival, although these were small series.11,12 A radiostereometric analysis (RSA)13 shows low levels of migration and collapse at 2 years. With CFP implants, however, a recent computerized tomography (CT)-assisted osteodensitometry study, which can differentiate between bone density (BD) in cortical bone and bone density in cancellous bone, showed progressive BD loss in proximal cortical bone between first-year (0–8%) and third-year (0–22%) measurements; BD in proximal cancellous bone also progressively decreased between the first year (0–33%) and the third year (0–45%). The authors concluded that metaphyseal fixation cannot be achieved with the CFP design. No cortical BD loss was observed below the lesser trochanter. This study suggests that, with this model, the fixation is diaphyseal.14
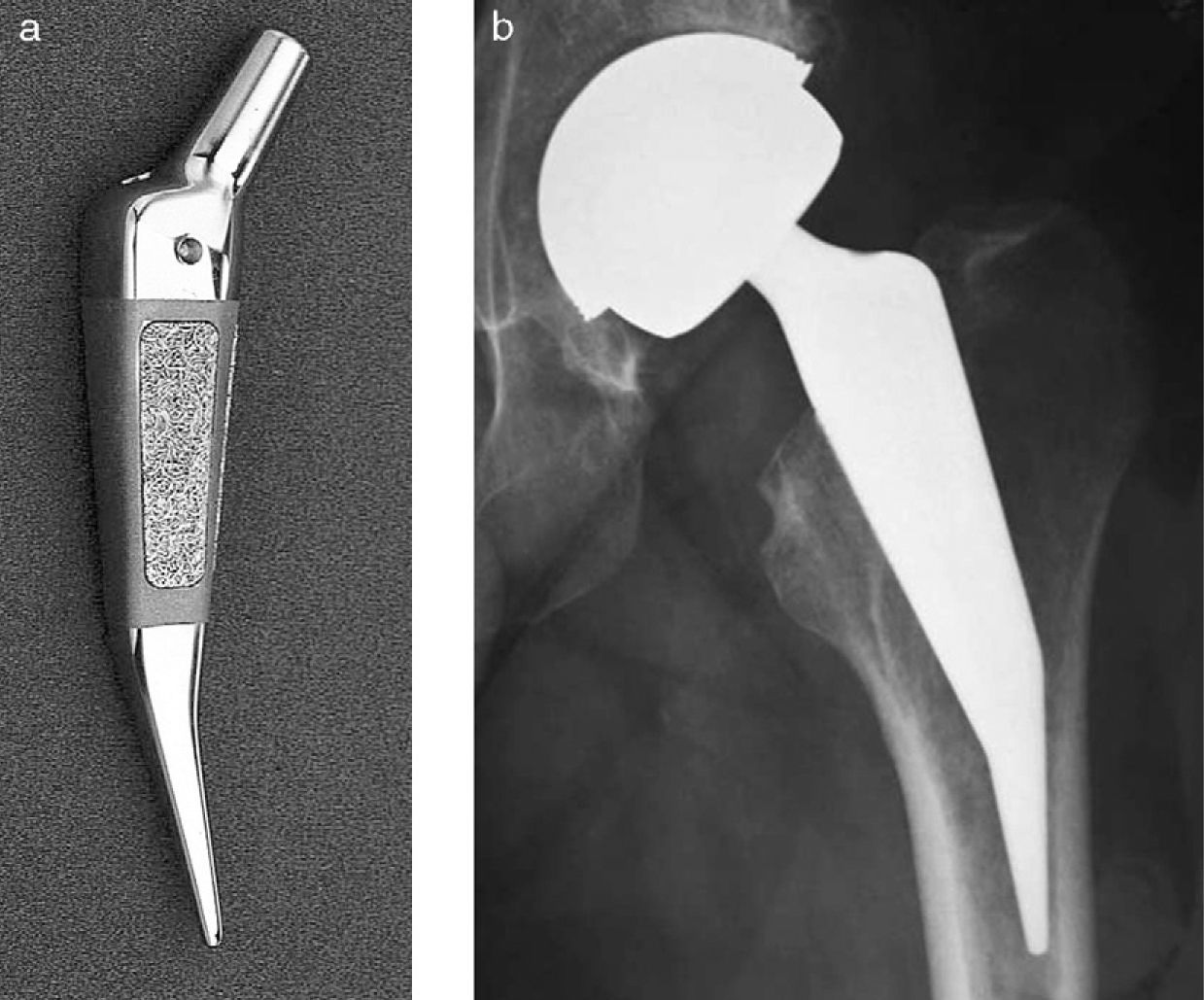
Prosthesis wedged into the metaphysisThe Mayo stem (Zimmer), first devised by Morrey in 1984 and approved by the Food and Drug Administration (FDA) in 1988, has a double-wedge design that preserves the femoral neck. Its proximal trapezoidal cross-section follows calcar and femoral neck contours, and the distal end runs parallel to and in contact with the external cortical bone of the femur.15 There have been reports of perforation of the external cortical bone,16 resorption of the neck and metaphysis,15 and cases where there was a high incidence of alignment problems.17 A review of the original series reveals a 98.2% survival rate for the stem with no mechanical loosening15; however, the authors do report cases of proximal osteolysis (6%) and intra-operative, non-displaced fractures (6%). Other authors18 report post-operative fractures and stem collapse with radiotransparent lines at 6 years (6.6%). In patients with a mean age of 50.8 years and a mean follow-up period of 5.7 years, studies with DXA (dual-energy X-ray absorptiometry) and a mathematical model for bone remodelling showed significant remodelling with proximal resorption and medial and lateral bone growth. The authors relate the remodelling to the mechanical load distribution defined by the implant design. Based on data found in the literature, however, they conclude that there is less bone resorption with short-stem than with most long-stem prostheses.16
There was also a study comparing patients with osteonecrosis (ON) of the femoral head and patients with osteoarthritis of the hip to evaluate the hypothesis that, in ON, the damage is not confined to the epiphysis but extends to the neck and metaphysis. In patients with a Mayo prosthesis, no differences in migration or valgus were found in the medium term.19
An experimental cadaver study showed no greater risk of fracture for the Mayo prosthesis than for the long-stem prosthesis. This would be a predictive factor for design-related peri-prosthetic fractures.20
The Metha prosthesis (Braun-Aesculap) has a modular neck that allows the cervical angle and offset to be changed. In the initial series, this was the source of failures due to the neck breaking or dislodging. Changes were made in the design. A prosthesis biomechanics study with the stem-neck interface in Metha and similar models showed that micromotion at the interface may be the cause of failure.21 The Metha profile is similar to that of the Mayo, slightly thicker in the metaphysis. It has metaphyseal anchoring, with no collar or trochanteric flare. Proximally, it has a porous plasma-sprayed coating, and its distal end rests against the external cortical bone. It demands meticulous technique,4 and the few studies that have been published are short-term.22
Like the Metha, the Nanos stem (Smith and nephew) has a Mayo-inspired design; it is collarless and somewhat thicker, with a short distal appendage. There is a short-term series that compares it with the Alloclassic using a DXA study.23
The Mini-Hip (Corin) and the Collo MIS (Lima) have a curved, conical profile, with no metaphyseal flare. The Aida (implant cast) is more conical, with a more curved end, and its profile is reminiscent of the Mayo prosthesis. There is one study of the Mini-Hip using radiographic geometry evaluation,24 but there are no published clinical results for these products.
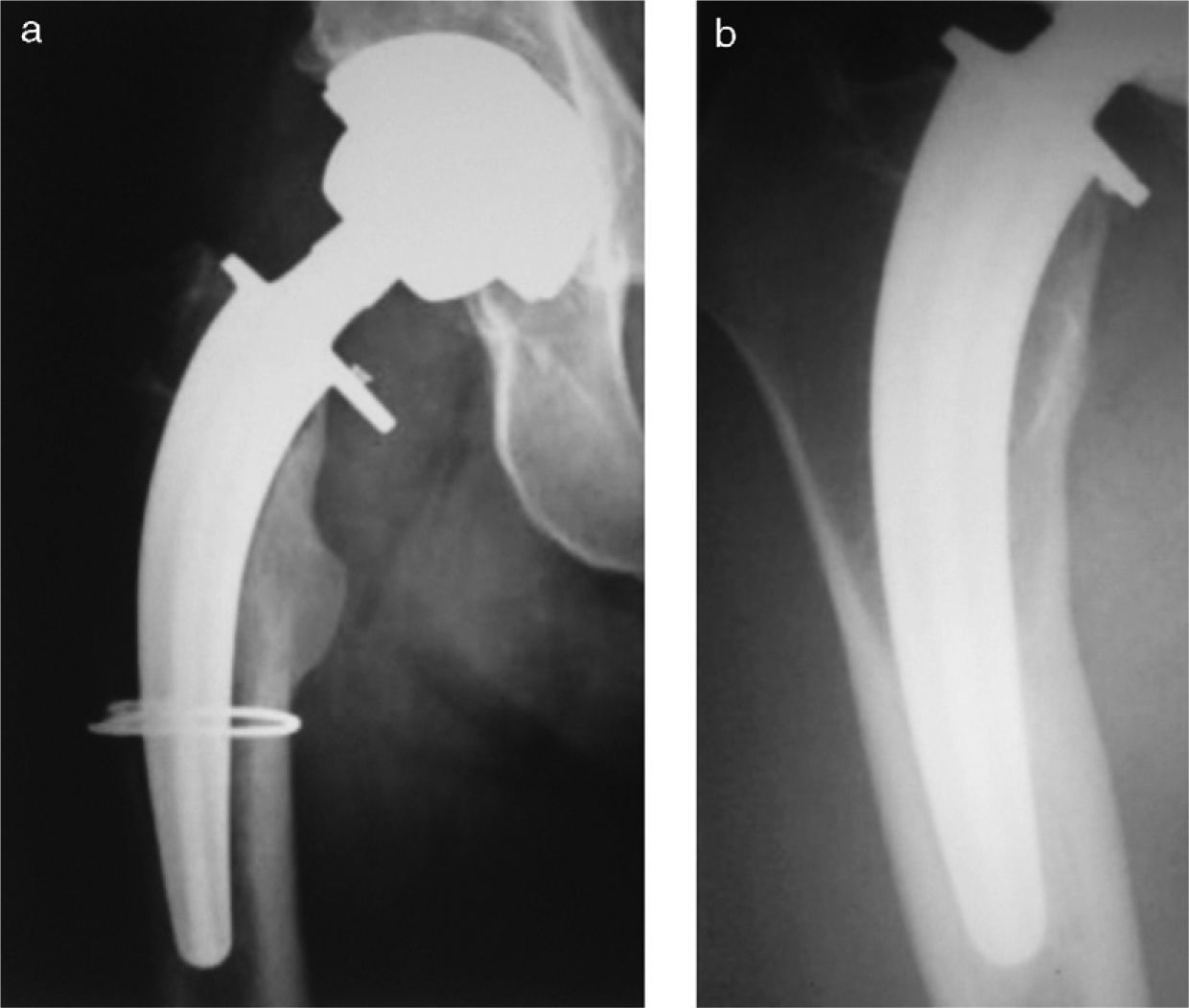
For the cut implant (ESKA)—a rough metaphyseal cylinder with a small, uncurved, distal appendage—there is a 5-year series with good results,25 but unacceptable rates for loosening and fracture of the distal extension have been published.26–28 This implant cannot be recommended (Figs. 1–6).
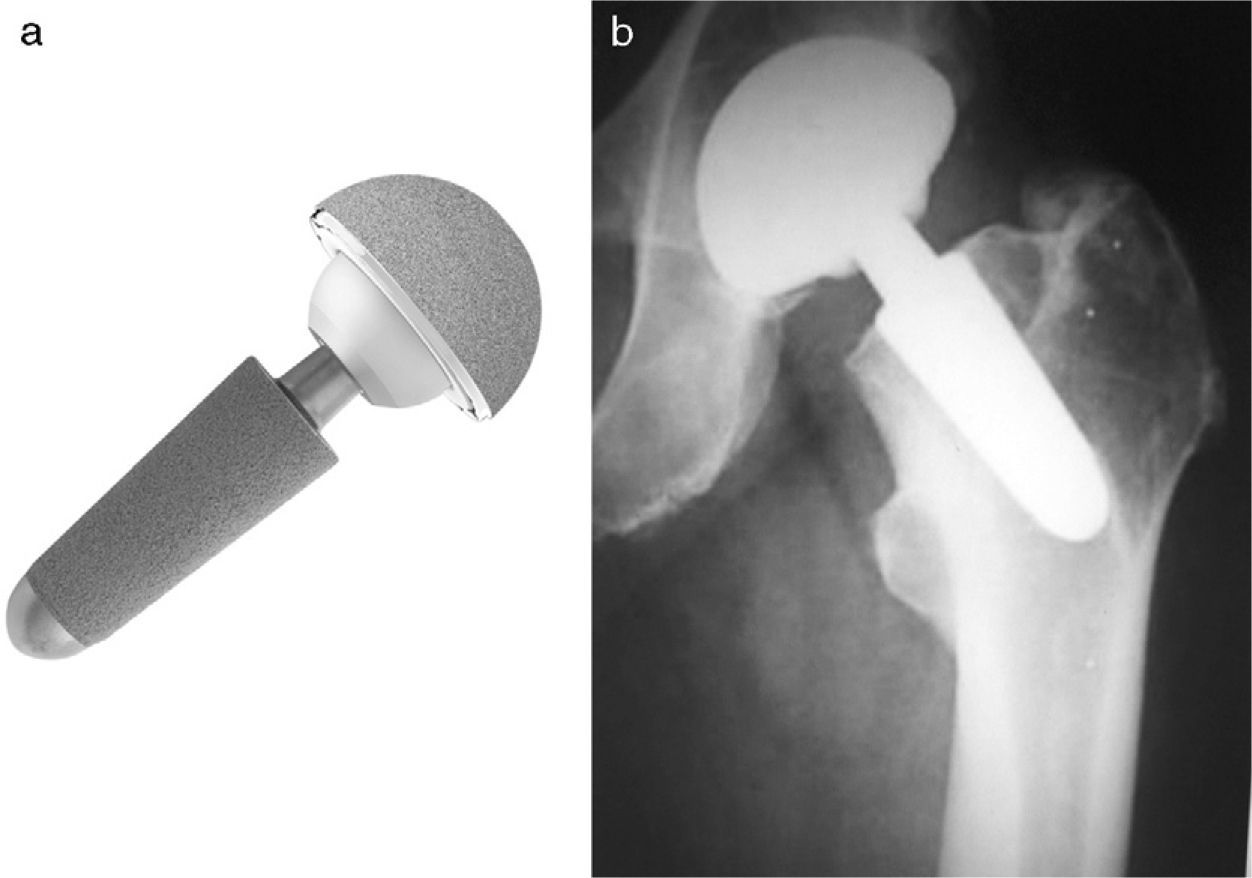
The proxima prosthesis (DePuy J&J) is a stemless femoral implant that is much wider proximally and much shorter distally than other conservative prostheses. It has a lateral flare lying in the cancellous bone of the greater trochanter, taking advantage of the quality and quantity of cancellous bone in that area to provide greater rotational stability. In young patients with good bone quality, metaphyseal loading occurs in this impacted cancellous bone. A high neck cut in its medial portion spares the calcar, and the lateral cut is made at the level of the piriform fossa. The prosthesis has proximal circumferential fixation to distribute the load and minimize the risk of fracture due to impaction or expansion.29 It is double-coated with porous plasma-sprayed titanium and hydroxyapatite, except at the distal end, which is polished. Primary stability ensures an early osseointegration and early formation of spot welds and medial and lateral buttressing that afford a durable fixation. DXA studies on the Santori “Custom” model (forerunner of the Proxima) demonstrate effective proximal loading with preservation of metaphyseal bone and greater density of the periprosthetic bone mass.30
Fixing the implant in neutral position, thereby ensuring primary stability, demands meticulous surgical technique and it requires the use of an external guide to obtain precise neutral orientation. It is not very permissive with varus positioning and with the choice of an underdimensioned size.
Because the initial good results with the Proxima in young patients were so promising,31–34 it was possible to expand the indications to any age up to 88 years.35 There are also cases published where the Proxima was used for rescue in patients who had implants in the femoral diaphysis that would have interfered with a long-stem prosthesis.36,37
Prosthetic head for transitioning from resurfacing prosthesisThe design of the BMHR (Birmingham Mid-Head Resection) device is intermediate between the BHR (Birmingham Hip Resurfacing) prosthesis (Smith and nephew) and the short-stem metaphyseal-fixed prosthesis. It is a solid metal hemisphere with a thick, porous-coated stem that is implanted in the femoral neck axis like a resurfacing prosthesis but without cement. After a subcapital osteotomy of the femur, it is fixed on the neck, replacing the defective or fragile femoral head and using a resurfacing acetabular component without insert. It is used in treatment of the hip when the femoral head is severely deteriorated or necrotic; it is also used for rescue in resurfacing prostheses, where the femoral component fails more often than the acetabular component and, at close to 40%, fracture of the neck is the most common mode of failure.38 The condition of the femoral neck may determine the choice of the revision implant. The limitations of the BMHR are the head size, determined by the acetabulum, and the controversial metal-metal couple. Moreover, in comparison with the BHR, the BMHR has shown neither superior mechanical strength nor greater resistance to fracture.38
With the same basic features as the BMHR—coated stem, uncemented, implanted in the femoral neck axis—the Silent (DePuy J&J) has a 12/14 cone that can accept an articulable metal or ceramic head with a standard acetabulum using a polyethylene, ceramic, or metal insert. Thus, it allows for a choice of acetabulum and friction couple: ceramic, metal, ceramic–polyethylene, or ceramic–metal. It is more versatile and is currently in the clinical trial phase.
DiscussionResurfacing hip prostheses have been very popular in recent years for treating hip disease in the young adult. They are conservative from the standpoint of the femur but not so much from the standpoint of the acetabulum. Because they require that the femoral head have reasonable viability, the head must be cemented. Tiny flaws in the reaming and cutting may give rise to neck fractures or notching that renders the neck fragile. Once the femoral cap has been cemented, the rest of the femoral head remains invisible. The friction couple is metal–metal.6 Numerous articles point out the complications specific to this prosthesis—aseptic lymphocytic vasculitis and associated lesions (ALVAL) and the appearance of pseudotumours with destruction of soft tissues around the hip—which require that the patient be closely followed, clinically and radiographically, and necessitate sometimes complex revision surgery. The effect of cobalt and chromium ions is not well known. In contrast to polyethylene, which are micrometric-scale particles, these are nanometric-scale metallic particles.39 Thus, while polyethylene wear causes a localized particle disease, metallic particles—of lesser volume but greater number, owing to their tiny size—are disseminated throughout the circulatory system.
The conservative prosthesis may be an alternative to resurfacing arthroplasty.
Long-term results with uncemented prostheses are equal to or better than those with classic cemented prostheses. Metaphyseal-fixed femoral implants show the best, thigh pain-free survival rates.1 Having no diaphyseal extension, conservative stems are implanted without cement and fixed in the metaphysis or on the neck,4,8,10 the various designs sparing femoral neck anatomy to a greater or lesser degree. DXA studies comparing short-stem prostheses with classic, anatomical, uncemented femoral components showed increased proximal (Gruen zone 1) and decreased distal (zone 7) BD with short-stem prostheses while, with the classic stems, BD was reduced in zones 1 and 7; this occurred with no clinical or radiographic changes.40 Long-term clinical studies on short-stem or stemless femoral implants are not yet available, but the articles that have been published on medium-term series show promising results in terms of primary stability, early osseointegration, and the absence of thigh pain and undesirable diaphyseal remodelling phenomena.4 They also reflect a low incidence of complications—provided that surgical technique is meticulous—because, having no self-aligning diaphyseal extension, short-stem implants generally tend toward varus positioning.
Regarding ON in comparison with osteoarthritis of the hip, no differences have been found in medium-term results with short-stem implants in terms of migration or varus.19
There is no evidence that functional results with minimally invasive surgery are superior to those with traditional surgical approaches.41
Femoral stems with a standard 12/14 cone allow the individual surgeon to choose the friction couple and the acetabulum.
This is why conservative prostheses—short-stem prostheses—may be preferred in surgical treatment of the hip in the young adult. Persistent good results have also expanded the indications for conservative prostheses to all patients of any age for whom an uncemented hip prosthesis is indicated.35 Once primary stability and early osseointegration have been accredited, along with an enduring stability comparable to the classic stems, research could focus on (1) the long-term stability and survival of the acetabular component and (2) the development of friction couples that are increasingly resistant to mechanical wear, corrosive wear, breakage, and banging and squeaking as well as other noise phenomena.
The survival rates and long-term results from conservative prostheses series will need to be compared with those for well-known prostheses in future studies.
Level of evidenceEvidence level: IV.
Conflict of interestThe authors have no conflicts of interest to declare.
Ethical DisclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of Data. The authors declare that no patient data appears in this article.
Right to privacy and informed consent. The authors declare that no patient data appears in this article.
Please cite this article as: Valverde-Mordt C, Valverde-Belda D. Prótesis femorales conservadoras. Vástagos cortos. Rev Esp Cir Ortop Traumatol. 2012;56(1):72-79.