The management of postoperative pain in joint replacement surgery represents a challenge. Therefore, the advent of new strategies in the management of pain such as local infiltration analgesia (LIA) and the adductor canal block, allowed an adequate postoperative pain control and early rehabilitation of the patient in total knee arthroplasty.
Materials and methodsA descriptive, observational and longitudinal study of a prospective cohort of patients operated by the group of joint replacements between September 29, 2017 and November 30, 2017 was conducted. They were evaluated with the analog pain scale for postoperative pain at 5 different times (1. Upon leaving recovery, 2. On the first postoperative day, 3. Before initiating in-hospital physical therapy, 4. At the end of physical therapy, 5. Upon departure from the clinic).
ResultsOf the 141 patients operated on, 70.9% of the patients were managed with LIA and 29.1% with adductor canal block. There were no differences between groups in postoperative pain assessment during the 5 different times (p ≥ .45).
DiscussionOur results indicate that LIA and the adductor canal blockade demonstrated the same efficacy for the control of postoperative pain and rehabilitation.
El manejo del dolor posoperatorio en la cirugía de reemplazos articulares representa un desafío. Por ello el advenimiento de nuevas estrategias en el manejo del dolor como la analgesia por infiltración local (LIA) y el bloqueo del canal de los aductores, han permitido un adecuado control del dolor posoperatorio y con ello la rehabilitación temprana del paciente en cirugía de reemplazo articular.
Materiales y métodosSe realizó un estudio descriptivo, observacional y longitudinal de cohorte prospectiva de pacientes intervenidos por el grupo de reemplazos articulares entre el 29 de septiembre de 2017 y el 30 de noviembre de 2017. Los cuales fueron evaluados con la escala análoga del dolor (EVA) para dolor postoperatorio en 5 momentos diferentes (1. Al salir de recuperación, 2. En el primer día de posoperatorio, 3. Antes de iniciar terapia física intrahospitalaria, 4. Al finalizar terapia física, 5. Al momento de salida de la clínica).
ResultadosDe los 141 pacientes intervenidos el 70.9% de los pacientes fueron manejados con LIA y el 29.1% con bloqueo. Se encontró que para cada momento de la evaluación del dolor posoperatorio había una distribución semejante en los desenlaces tanto para el grupo de LIA como bloqueo, con la obtención de valores de p ≥ 0,45.
DiscusiónNuestros resultados indican que tanto la LIA como el bloqueo del canal de los aductores demostraron la misma eficacia para el control del dolor posoperatorio, y así mismo la rehabilitación temprana (marcha y movilidad) del paciente.
The management of postoperative pain in joint replacement surgery represents a challenge, because pain interferes with early functional recovery, prolongs hospital stay and the use of opiates, reduces the patient satisfaction scale score, increases the rate of hospital readmission and the appearance of chronic pain.1 it is also the first cause of hospital readmission prior to 30 days.
Traditional techniques with intravenous opiates do not provide good analgesia and have many side effects. Epidural analgesic has a 20% failure rate as the only analgesic method in total knee replacement1; femoral block does provide good analgesia for the anterior surface of the knee but in 1%–2.5% of cases it is associated with motor block which impedes early rehabilitation, and may lead to nerve lesion or local infection, although the latter is increasingly rare.2–6
However, other postoperative pain management techniques, such as adductor canal block have appeared as suitable techniques to reduce the consumption of opiates during the first 48 h, with much lower weakness in the quadriceps, compared with the femoral nerve block. However its great disadvantage is that this procedure is dependent upon the surgical skills involved.1,7
Local infiltration analgesic (LIA) is a simple, easily reproducible technique, which needs no special training or equipment. It has been demonstrated to be an effective procedure for pain control and provides optimal conditions for the initiation of early rehabilitation.1,7
Our aim was to assess whether adductor canal block or LIA in the context of a multimodal analgesic guideline offered greater control of pain and early recovery in replacement surgery.
Materials and methodsA descriptive, observational longitudinal study of a prospective cohort of patients who had undergone surgery for joint replacements between 29th September 2017 and 30th November 2017 was conducted. The sample population were 176 cases of patients who underwent joint replacements. They were represented by 141 cases of knee procedures (TKR: total knee replacement / TKRR: total knee replacement revision / KRA-arthroplasty: knee replacement arthroplasty a / KA-arthrodesis: artrodesis of the knee), of all ages, who agreed to participate in the study and who were assessed during the postoperative period.
The sample was divided up through convenience, without random assignation and according to the decision of the anaesthesiologist, for the determination of pain management. This was either adductor canal block performed by the anaesthesia department or local analgesic infiltration (LIA) performed by the surgeon during the surgical procedure in the two groups. Group 1: patients with ultra-sound guided regional adductor canal block performed by the anaesthesia group with a mixture of drugs: 5 cc of bupivacaine at .75% + 5 cc of lidocaine at 2% without epinephrine. Group 2: patients with LIA performed by the surgeon with a mixture of 20 cc de bupivacaine at .75% with or without epinephrine + 30 mg (1 cc) ketorolac + 10 mg (1 cc) morphine + 28 cc saline solution, with a standard injection technique in 8 anatomical points of the knee: (1) suprapatellar bursa and quadriceps tendon; (2) medial retinaculum; (3) patellar tendon and fat pad; (4) medial collateral ligament and capsular union of the medial meniscus; (5) tibial insertion of the posterior cruciate ligament; (6) femoral insertion of the anterior cruciate ligament; (7) lateral collateral ligament and capsular union of the lateral meniscus and (8) lateral retinaculum.8
Both groups received additional analgesic management according to times and medical prescription: 1 g acetaminophen and 200 mg celecoxib one hour prior to surgery, 1 g i.v. dipyrone every 6 h and 50–10 mg tramadol every 8 h as postoperative analgesia and they were assessed with the verbal analogue scale (VAS) for postoperative pain from 0 to 10 (0: no pain; 1-3: slight pain; 4–6: moderate pain; 7–10: severe pain) at 5 moments: (1) upon leaving recovery; (2) on the first postoperative day; 3) before initiating in-hospital physical therapy; (4) at the end of physical therapy and (5) upon departure from the clinic.
Regarding assessment of early functional recovery of the patient, the in-hospital physiotherapist made the assessment and the follow-up of the following items: sitting, standing, support protected with external means such as a stick or waling aid, recovery of mobility arcs, active and passive mobility and starting to walk prior to patient discharge. Each of them was assessed according to tolerance.
The variables were collected on a sheet based on the Microsoft Office Excel 2007® programme, each one of them was coded and later exported to the statistical programme SPSS® version 20.0. Univariate and bivariate analysis was performed. For description of the normally distributed continuous variables central tendency measures were used, mean and standard deviation (SD); median and interquartile range were used in the contrary case. The categorical variables were presented as frequency, proportion and 95% confidence intervals (95%CI). P values of <.05 were considered statistically significant.
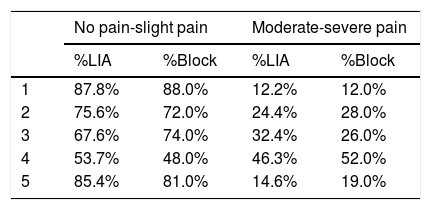
ResultsOf the 141 patients operated on by the joint replacement group 70.9% were controlled with LIA and 29.1% with block, with an average age of 64.5 years. The distribution of the groups in knee procedures by intervention for pain management is contained in Table 1.
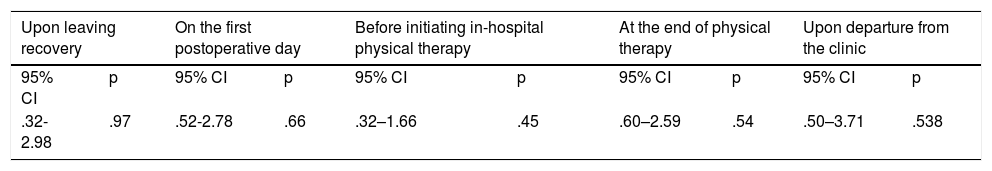
According to the multivariate analysis, for each moment of postoperative pain assessment a similar distribution was observed in the triggers both for the LIA group and for the block group, which may be observed in Table 2. This was confirmed with obtainment of values of p ≥ .45 (Table 3).
Distribution of postoperative pain during the 5 assessment moments.
| No pain-slight pain | Moderate-severe pain | |||
|---|---|---|---|---|
| %LIA | %Block | %LIA | %Block | |
| 1 | 87.8% | 88.0% | 12.2% | 12.0% |
| 2 | 75.6% | 72.0% | 24.4% | 28.0% |
| 3 | 67.6% | 74.0% | 32.4% | 26.0% |
| 4 | 53.7% | 48.0% | 46.3% | 52.0% |
| 5 | 85.4% | 81.0% | 14.6% | 19.0% |
1: upon leaving recovery; 2: on the first postoperative day; 3: before initiating in-hospital physical therapy; 4: at the end of physical therapy and 5: upon departure from the clinic.
Distribution of the 95% CI and p value at the 5 pain assessment moments.
| Upon leaving recovery | On the first postoperative day | Before initiating in-hospital physical therapy | At the end of physical therapy | Upon departure from the clinic | |||||
|---|---|---|---|---|---|---|---|---|---|
| 95% CI | p | 95% CI | p | 95% CI | p | 95% CI | p | 95% CI | p |
| .32-2.98 | .97 | .52-2.78 | .66 | .32–1.66 | .45 | .60–2.59 | .54 | .50–3.71 | .538 |
Adductor canal block has become a suitable technique. It reduces the consumption of opiates during the first 48 h after total knee replacement, with much lower weakness in the quadriceps compared with femoral nerve block, where apart from sensitive block, there is a motor block which affects early rehabilitation for the patient. However, the block as an analgesic control has the limitation of being dependent on the surgeon, with a risk of failure close to 15%.1,7
The LIA technique, however, is simply reproducible, and needs no special training or equipment. Several recent publications have demonstrated that it is an effective procedure for pain control and that it provides the optimal conditions to initiate early rehabilitation. These publications indicate superiority in the ability to walk 24 and 48 h after surgery. However, many studies present the limitations of not having a standardised protocol for the infiltration technique to suggest which drugs to use in infiltration and at what doses.1,7,9
The most highly accepted LIA application technique is based on the application of a mixture of drugs (local anaesthetics, steroid, anti-inflammatory and on occasions an inductor of platelet aggregation) in 8 regions with high neurosensorial perception and an elevated concentration of mechanoreceptors, which serve as a guide for conducting this study. Becoming aware of the 8 points of infiltration and the anatomy of the knee reduces the risk of the main complication of LIA: lesion of the popliteal artery, which is located 2 cm from the posterior capsule and in over 95% of cases lateral to midline.10
Many studies are in favour or against the use of the LIA technique of regional block or even the use of epidural analgesia for postoperative pain management. Choi et al.11 showed that the effects of epidural analgesia are limited to a period of 4–6 h, which makes it only a pain relief technique for the immediate postoperative period and there would be a risk of adverse reactions or complications such as hypotension, urinary retention or itching.
Spreng et al.12 found that patients treated with LIA had faster joint function and mobility than patients with intravenous analgesia, showing that the use of some drugs, such as morphine and ketorolac may improve pain management up to 24 h after termination of surgery.
Nevertheless, the LIA studies have many limitations, many of them are associated with the non standardisation of the cocktail of drugs required for appropriate analgesic control, drug dose, total volume of drug dilution, infiltration time and technique used.12–15
A meta-analysis conducted by Hu et al.1 found that LIA offered a better analgesic than regional block when resting and preserved the quadriceps function, which facilitated early functional recovery.
Also, Lund et al.16 demonstrated that the adductor canal block provided analgesia postoperatively up to 48 h, which was associated with a reduced consumption of supplementary opiates. However, studies are needed to endorse the use of the continuous adductor canal block as a postoperative analgesic control from implantable infusion pumps.
Bauer et al.17 consider that the femoral nerve block is the gold standard for postoperative pain in total knee arthroplasty and should be complemented, when necessary, with a rescue dose of opiates. However, they consider that further studies are required to endorse the use of LIA or adductor canal block as new regional analgesic techniques.
Our results indicate that both the LIA and the adductor canal block have the same efficacy for postoperative pain control, since there were no statistically significant differences between them.
However, the researchers consider that LIA is a superior technique due to its simplicity, availability, easy reproduction, non requirement of trained staff, appropriate pain management and non compromise of the knee motor function, thereby not limiting early mobility and rehabilitation.
It should be noted that a limitation of this study is that treatment groups were not homogeneously assigned and this impeded analysis of results in terms of the interventions.
Level of evidenceLevel of evidence II.
FinancingNo external financing or financial support was received for conducting this study.
Conflict of interestsThe authors have no conflict of interests to declare in this study.
Please cite this article as: Montoya BE, Serna ID, Guzmán DL, López JJ, Mejía LA, Restrepo VE. Estudio observacional descriptivo sobre recuperación funcional temprana y dolor postoperatorio en cirugía de reemplazo articular de rodilla. Rev Esp Cir Ortop Traumatol. 2019;63:389–393.