Neurofibromatosis type 1 (NF-1) is one of the most common autosomal dominant disorder affecting humans. Patients with NF-1 may present with characteristic orthopedic manifestations such as scoliosis, congenital pseudoarthrosis and limb hyperttrophy. Dislocation of the hip associated with NF-1 is a rare occurrence. There is a relative paucity of reported cases of pathological hip dislocation in patients with NF-1, with 13 documented cases found in the published literature. Seven dislocations occurred following trivial trauma and 6 cases were deemed atraumatic. We report a case of hip dislocation in a 26-year-old male with NF-1 and scoliosis, that was treated successfully by closed reduction and skin traction.
La neurofibromatosis tipo I (NF-1) es una de las enfermedades autosómicas dominantes más comunes que afecta a los humanos. Los pacientes con NF-1 pueden presentar características manifestaciones clínicas ortopédicas como son la escoliosis, pseudoartrosis congénita y la hipertrofia de la extremidad. La luxación de cadera asociada a la NF-1 es muy poco frecuente. Hay muy pocos casos publicados de luxación de cadera en pacientes con NF-1, encontrando 13 casos documentados en la bibliografía. Siete luxaciones ocurrieron tras un traumatismo leve y 6 fueron atraumáticas. Presentamosun caso de una luxación de cadera en un varón de 26 años con NF-1 y escoliosis que fue tratado satisfactoriamente con reducción cerrada y tracción blanda.
Neurofibromatosis is an autosomal dominant disease, which was first described by the German pathologist Friedrich von Recklinghausen in 1882. It is a rare disease which is inherited in an autosomal dominant pattern and which is characterized by severe involvement of the musculoskeletal system, including tibial pseudoarthrosis (or nonunion), scoliosis, etc. in addition to other dermatological, neurological and vascular lesions.1
The treatment of pseudoarthrosis and scoliosis has been the subject of various publications; however, atraumatic hip dislocation is rare and has a poorly defined and controversial treatment.
We report the case of a atraumatic hip dislocation in a young male patient suffering type 1 neurofibromatosis (NF-1).
Case reportThe patient was a 26-year-old male with NF-1 who was referred to our emergency department due to left inguinal pain with a sharp and sudden onset during sleep. He presented inability for ambulation and intense inguinal pain on the left side, with palpation of a hard tumor at that level. The range of left coxofemoral mobility was severely limited and painful, with limb shortening and external rotation attitude. The patient did not present distal motor or sensory deficits. He had been diagnosed with NF-1 at age 3 and suffered severe thoracolumbar scoliosis. As relevant history, and secondary to the disease, the patient only had 1 kidney since the age of 13, with thoracolumbar arthrodesis, and with sacral support as a treatment for his lumbosacral scoliosis, currently presenting a Cobb angle of 65° (T9-L3). He had also undergone a distal femoral epiphysiodesis at age 14 due to dysmetria caused by a 3cm elongation of the left femur. At age 25, he underwent removal of the spinal osteosynthesis material due to an infection in which Staphylococcus aureus was isolated and which evolved successfully with antibiotic treatment.
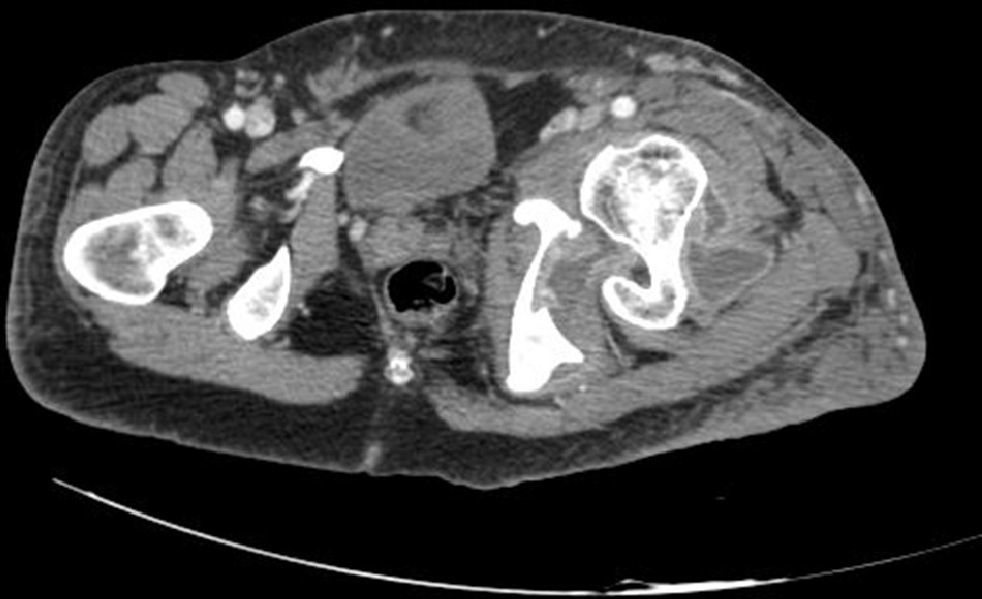
A radiographic study of the pelvis showed a left anterior coxofemoral dislocation (Fig. 1). We also conducted MRI and CT scans of the pelvis. The CT scan showed an anterior dislocation of the left coxofemoral joint and considerable swelling of the periarticular soft tissue (Fig. 2). In addition to the dislocation, the MRI scan revealed a soft-tissue mass in the anterior side of the femoral neck and trochanteric region. This mass had a maximum craniocaudal diameter of about 100mm by about 80mm in the anteroposterior plane and was compatible with plexiform neurofibroma. We conducted a closed reduction of the hip under general anesthesia, noting adequate coxofemoral stability and subsequently applying soft traction for 3 weeks. The study was complemented by electromyography, which revealed chronic neurogenic involvement in the L5 region without active denervation. Following reduction under general anesthesia, soft traction and unloading of the limb for 3 weeks, we placed a girdle-type orthotic device for 3 months, with fixed hip flexion of about 15° and abduction of the limb at 20°. At 12 months follow-up, the patient is asymptomatic and leads a similar life to that prior to the dislocation.
DiscussionHip dislocation associated with von Recklinghausen disease has been reported in 13 cases to date. Of these, 7 were due to minor trauma2–7 and 6 were atraumatic.8–12
Several causes of atraumatic dislocation have been reported, including: neurofibroma, which creates a mechanical problem causing dislocation2,4,6,8,10 and dysmetria due to limb elongation which determines a pelvic obliquity with decreased coverage of the femoral head by the cup4 on the elongated side; pelvic obliquity due to scoliosis will also generate the same problem of decreased coverage of the femoral head.12
Neurological disorders with muscle denervation or hypotonia can also cause an atraumatic hip dislocation.3,8 In the case presented, the neurofibromas did not cause mechanical involvement, as proven by the simple and stable reduction. In addition, the case associated pelvic obliquity secondary to scoliosis and dysmetria by elongation. These 2 factors determined an excessive verticality of the acetabulum which led to a significant reduction of the femoral head cover. This fact, along with muscle atrophy, caused a hip dislocation while the patient was sleeping, a phase in which there is greater muscle relaxation.
There are very few studies in the literature with therapeutic homogeneity. We found treatments ranging from surgical reduction and removal of the neurofibroma in the presence of a mechanical problem4 to hip arthroplasty, with the latter being a complex and bloody5 solution, as well as the possibility of carrying out a Girdlestone procedure9 in recalcitrant cases of dislocation.
Other cases reported applying surgical techniques like rotational femoral osteotomy aimed at increasing the anterolateral coverage of the joint,12 in association or not with other techniques.
Conservative treatment should always be the first option. Closed reduction should always be attempted and stability should be assessed prior to making other surgical decisions, if applicable.
The present case is currently solved, but the evolution is uncertain, since the triggering mechanisms of the dislocation are still present and are difficult to reverse.
Level of evidenceLevel of evidence IV.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation adhered to the ethical guidelines of the Committee on Responsible Human Experimentation, as well as the World Medical Association and the Declaration of Helsinki.
Data confidentialityThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Please cite this article as: del Bosque-Herrero A, Ezquerra-Herrando L, Albareda-Albareda J. Luxación de cadera en un paciente con enfermedad de von Recklinghausen. Rev Esp Cir Ortop Traumatol. 2014;58:246–248.