Varus deformity of the proximal humerus in children is a little known pathology due to its low incidence of presentation. Progress has been made in recent years in understanding the possible etiology and pathophysiological causes. Radiological criteria for diagnosis and functional impairment that occurs have also been defined. However, there are few reports in the literature about the surgical treatment of this deformity in children. In this paper we present a case of surgical treatment of this deformity by corrective osteotomy fixed with precontoured external maleolar plate osteosynthesis.
La deformidad en varo del húmero proximal en la infancia es una enfermedad poco conocida debido a su baja incidencia de presentación. En los últimos años se ha progresado en el conocimiento de su posible etiología y fisiopatología de producción. Su etiología puede ser muy variada, tanto con causas traumáticas como no. También han sido bien definidos los criterios radiológicos de diagnóstico y la discapacidad funcional que produce. Sin embargo, existen pocos trabajos en la literatura sobre el tratamiento quirúrgico de esta deformidad en la infancia. En este artículo presentamos un caso tratado mediante osteotomía valguizante fijada con una placa de osteosíntesis preconformada maleolar externa.
Humerus varus is an infrequent entity which is characterized by an increase of the varus angulation of the proximal humerus and a shortening of the length of the limb. Several etiologies, traumatic and atraumatic, have been proposed as the causative origin of this deformity.1
From the clinical standpoint, the most common symptoms are pain and limitation of the range of movement in abduction and antepulsion, caused by an impingement of the greater tuberosity with the acromion.
Kölher2 described the radiographic criteria for its diagnosis, including: reduction of the head-neck angle below 140°, elevation of the greater tuberosity over the superior margin of the neck, and reduction of the distance between the joint surface of the head and the lateral cortical of the humerus.
Several methods of surgical treatment have been reported for the correction of this disease, with the most common being corrective osteotomy at the level of the neck deformity, followed by the application of plaster casts in abduction3 and fixation through tension cerclage.4,5
This article presents a case treated by valgus osteotomy and osteosynthesis with a precontoured rigid plate, in a similar manner to osteotomies conducted in the hip. We used an adult fibular malleolus plate due to the lack of proximal humeral epiphyseal plates specific for children. To our knowledge, this type of treatment has not been reported previously in adolescents.
Case reportThe patient was a female who attended consultation for an assessment at the age of 11 years. She presented a previous history of neonatal sepsis by Klebsiella pneumoniae which was treated by intravenous antibiotic therapy. No joint involvement was observed at this point. The subsequent evolution was favorable, with no sequelae being observed once the sepsis was resolved. The girl was able to crawl normally and began ambulation at the age of 1 year with no incidents.
Subsequently, the parents observed a progressive shortening and functional limitation of the right arm during growth, so they requested a traumatology assessment. This study took place at the age of 9 years, and the radiographic tests revealed varus deformity of the proximal end of the humerus and shortening of the length of the upper right limb. The patient was referred for rehabilitation treatment. Following extensive physiotherapy with no improvement, she was referred to our consultation for a surgical evaluation.
At the time of our assessment, the patient reported pain with everyday movements and functional limitation due to loss of movement range in the right shoulder, which had worsened in recent months up to a point where it limited everyday activities.
The examination found moderate deltoid, supraspinal and infraspinal atrophy, with clear shortening of the right arm, and with the forearm and hand having the same length as the contralateral limb. There were no signs of distal neurovascular involvement. Regarding the range of active movement of the glenohumeral joint, abduction was 60°, antepulsion was 80°, sacral internal rotation and external rotation of 45°. The contralateral limb presented abduction of 120°, antepulsion of 160°, dorsal internal rotation and external rotation of 70°.
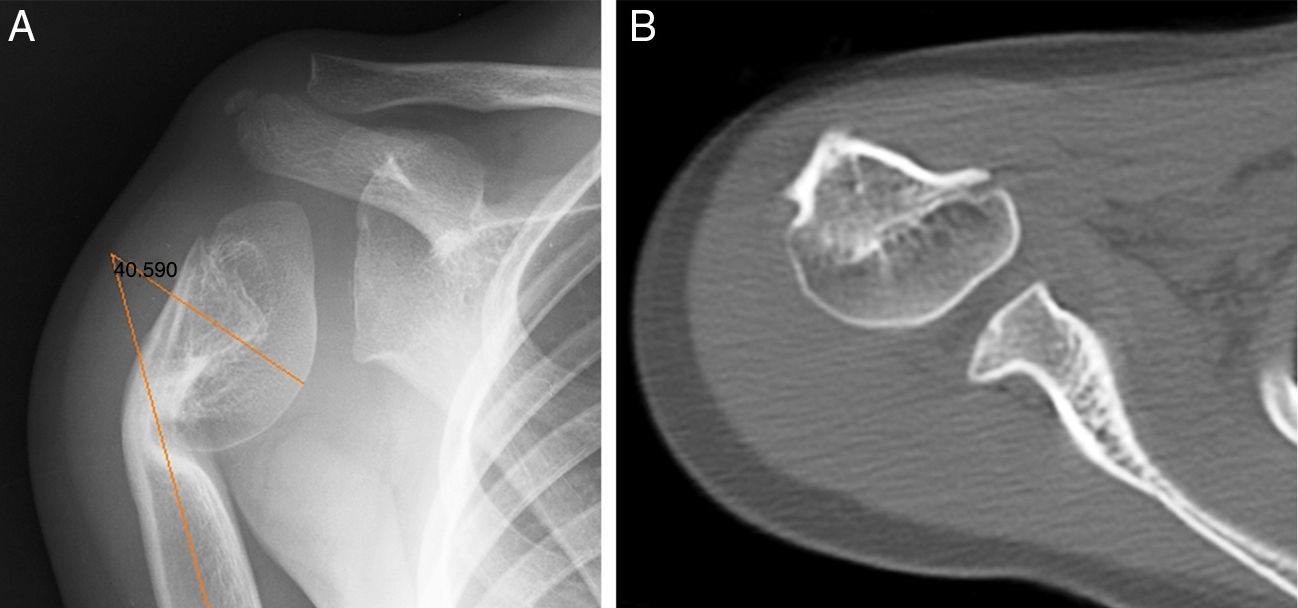
The radiographic study revealed varus deformity in the surgical neck of the humerus with closure of the medial growth plate and a neck-diaphysis angle of 40° (Fig. 1A). The comparative study of both upper limbs showed a shortening of 9cm of the right humerus. The CT scan identified a flattening of the glenoid cavity, as well as incurvation and thinning of the proximal metaphysiodiaphyseal region of the humerus, with remodeling of the humeral head (Fig. 1B).
The diagnosis of humerus varus secondary to neonatal septic arthritis led to consideration of surgical treatment through valgus osteotomy at the level of the humeral surgical neck. After being informed of the possibility of conducting a surgical correction of the deformity, the parents accepted the treatment.
Surgical techniqueThe patient was placed in the “beach chair position” with a support under the affected arm. The deformity was exposed through a deltopectoral approach to the proximal humerus and a partial subperiosteal disinsertion of the pectoralis major and anterior insertion of the deltoid were carried out.
Two Kirschner wires were placed under scopy control from the lateral region of the humerus, marking the location and direction of the planned osteotomy. An oblique, wedge-shaped, closure osteotomy was conducted under direct vision at the level of the surgical neck, in the location of the metaphyseal deformity. We carried out a provisional fixation using Kirschner wires and conducted an intraoperative scopy control to verify the correction of the deformity. Once a satisfactory correction had been obtained, we conducted the definitive fixation using a rigid osteosynthesis plate (Epi-Union© external malleolar plate [Stryker, Kalamazooo, MI]), with 4 proximal and 2 distal cortical cancellous screws. We verified the stability of the fixation assembly and closed the surgical site by planes.
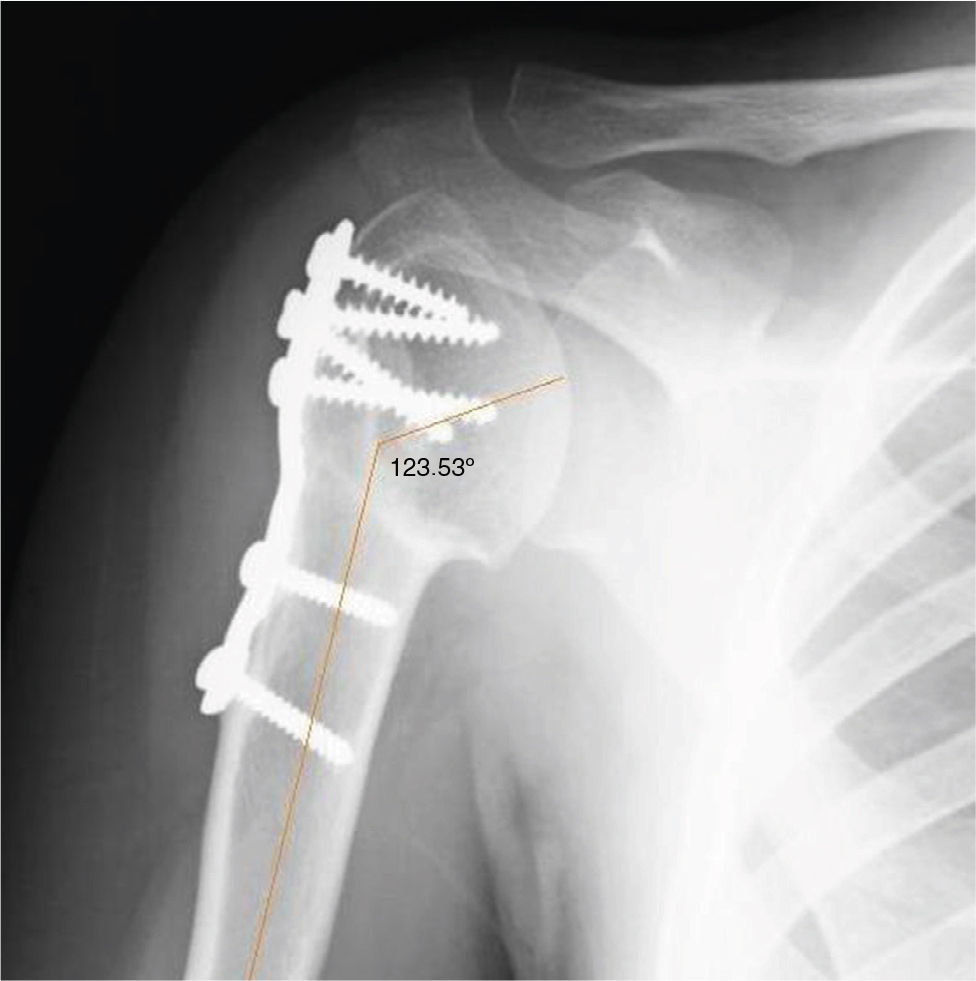
There were no incidences in the immediate postoperative period, during which the patient was immobilized with a sling. Rehabilitation treatment through passive mobilizations began 1 week after the intervention. Active exercises of the range of movement began after 4 weeks. Exercises to build musculature were started after 8 weeks, once the osteotomy was consolidated. The radiographic control conducted after 1 year confirmed that the reduction was maintained and found no signs of osteonecrosis.
ResultThe range of movement has improved gradually and, at present, more than 1 year since the intervention, the glenohumeral joint presents 90° abduction, 120° antepulsion, dorsal internal rotation and full external rotation.
The radiographs showed a correction of the neck-diaphysis angle of 83°, from 40° preoperatively to 123° after the surgical treatment (Fig. 2).
The osteotomy was consolidated at 8 weeks from the surgery, without complications. After 2 years of evolution, the correction achieved was maintained and no necrosis of the humeral head was observed.
DiscussionVarus deformity of the proximal humerus is an infrequent pathology which affects the development and function of the glenohumeral joint. Several causes have been proposed for this condition.6–12 Ogden et al.1 classified the possible causes of this alteration into: normal anatomical variations, posttraumatic, pathological fractures, skeletal dysplasias, metabolic disorders, osteomyelitis, hematological alterations, neoplasms and neuromuscular diseases.
All these conditions can cause a destruction of the medial physis, with the lateral physis remaining intact and continuing its growth, leading to varus deformity of the proximal humerus. The proximal physis is responsible for approximately 80% of humeral growth in terms of length,13 so its alteration is usually accompanied by a progressive shortening with respect to the contralateral limb. Mobility of the glenohumeral joint, especially in flexion and abduction, is limited by impingement of the greater tuberosity with the acromion.
Surgical treatment should be considered in cases with continuous pain and limitation of movement restricting everyday activities. Several treatment methods have been proposed to correct this pathology: in the past, the most common was osteotomy and immobilization with a plaster cast at 90° abduction.3 This treatment requires prolonged immobilization until consolidation of the osteotomy has been achieved, thus entailing significant discomfort for patients. Moreover, it has been associated with losses of reduction and subsequent rigidity. Acromial resection was another treatment proposed in the past by Lloyd-Roberts14 and, although the author described it as being simpler than osteotomies and with a satisfactory clinical outcome in cases like the present one, it is an aggressive form of treatment which causes significant deformity at the level of the shoulder and which has not been followed in subsequent years. At present, the most commonly accepted surgical treatment is valgus osteotomy with fixation through needles and tension wires, as described by Gill and Waters.4 In recent years, Ugwonali5 also reported satisfactory results after using this technique in a series of 6 patients.
Treatment through osteotomy and plate fixation has been described previously in adults for the treatment of humerus varus secondary to fractures. Solonen and Vastamaki15 published satisfactory results in 5 out of 7 patients. In their article they referred to the importance of factors such as the presence of preoperative glenohumeral contractions, presence of severe muscle atrophy and scarce motivation for rehabilitation treatment as elements which significantly influenced the final outcome.
To our knowledge, the correction obtained through osteotomy fixed with a plate has not been described in adolescent patients with immature skeletons. Based on the experience with hip osteotomies, we believe that osteosynthesis of osteotomies with a rigid plate are an adequate, safe and reliable option. The lack of precontoured plates for children adapted to the proximal end of the humerus is a drawback, but in our case we employed a precontoured adult plate adapted to the distal fibula and observed an adequate adaptation, which enabled a stable osteosynthesis. We believe that it is a good solution for cases with significant deformities. As previously reported by other authors,5 an important point is attempting to preserve the medial cortical of the humerus, in order to avoid possible lesions of the ascending branch of the anterior humeral circumflex artery.
In conclusion, osteosynthesis with an adapted rigid plate achieves stable fixation, thus reducing the risk of pseudoarthrosis and loss of reduction, whilst also allowing early mobilization to avoid postoperative rigidity. The need to remove the osteosynthesis material can represent a drawback, but as pointed out, this type of deformity is usually associated with a shortening of the length of the limb, so the material can be removed during the lengthening intervention, in a second surgical stage.
Level of evidenceLevel of evidence V.
Ethical responsibilitiesProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Please cite this article as: Tallón-López J, Domínguez-Amador JJ, Andrés-García JA. Húmero varo: corrección mediante osteotomía proximal valguizante con placa de osteosíntesis preconformada en edad infantil. Rev Esp Cir Ortop Traumatol. 2014;58:249–252.