A 76-year-old male patient with a history of implantation of a total hip arthroplasty (Perfecta (Orthomet)®), who presented with an iliac fossa mass, increased diameter of the thigh, and pain during hip flexion and extension. CT and ultrasound show the presence of a giant cystic mass in left iliac fossa about 7cm in diameter next to the prosthesis. A pseudo-tumor secondary to wear debris after placement of a total arthroplasty is rare. We present a case of a large iliopsoas bursitis caused by polyethylene particles, which caused compression and thrombosis of the superficial femoral vein.
Paciente varón de 76 años, con antecedente de implantación de prótesis total de cadera tipo Perfecta (Orthomet®), que consultas por masa en fosa ilíaca, con aumento del diámetro del muslo y dolor flexión y extensión de la cadera. Los estudios complementarios de ecografía y tomografía evidencian la presencia de una tumoración quística gigante lobulada en fosa ilíaca izquierda de unos 7cm de diámetro en la proximidad de la prótesis. La formación quística ocasionada por la enfermedad del polietileno tras la colocación de una artroplastia total de cadera es poco frecuente. Presentamos un caso de bursitis del psoas de gran tamaño, secundaria a la liberación de partículas del polietileno, que ocasionó compresión y trombosis de la vena femoral superficial.
The iliopsoas bursa is the largest bursa around the hip, extending across the anterior surface of the joint capsule and toward the pelvis behind the iliopsoas muscle. Communication with the joint can be demonstrated in 9–15% through arthrography.1 Enlargement of the sac may result from increased synovial fluid production due to inflammatory processes, such as pigmented villonodular synovitis, bacterial bursitis, and overuse activity,2,3 but it is most often secondary to an inflammatory condition in the hip. Osteolysis from polyethylene wear in hip arthroplasty is a phenomenon well documented in the literature. However, this seldom causes a swelling to form in the soft tissues around the prosthesis, resulting in compression of the adjacent structures. We present the case of a large iliopsoas bursitis secondary to the release of polyethylene particles, which caused superficial femoral vein compression and thrombosis.
Clinical caseThe patient was a 76-year-old male with a history of hepatitis B, upper gastrointestinal bleeding, and left cementless total hip replacement (THR) 7 years earlier—Perfecta (Orthomet®, Minneapolis), including a titanium alloy femoral rod of anatomical design with porous-coated proximal third, fully porous-coated hemispheric acetabular component, flanges, and screws in 2 orifices. The friction couple was metal to high-molecular-weight polyethylene (Duramer®), gamma-ray sterilized, with 28-mm chrome-cobalt head.
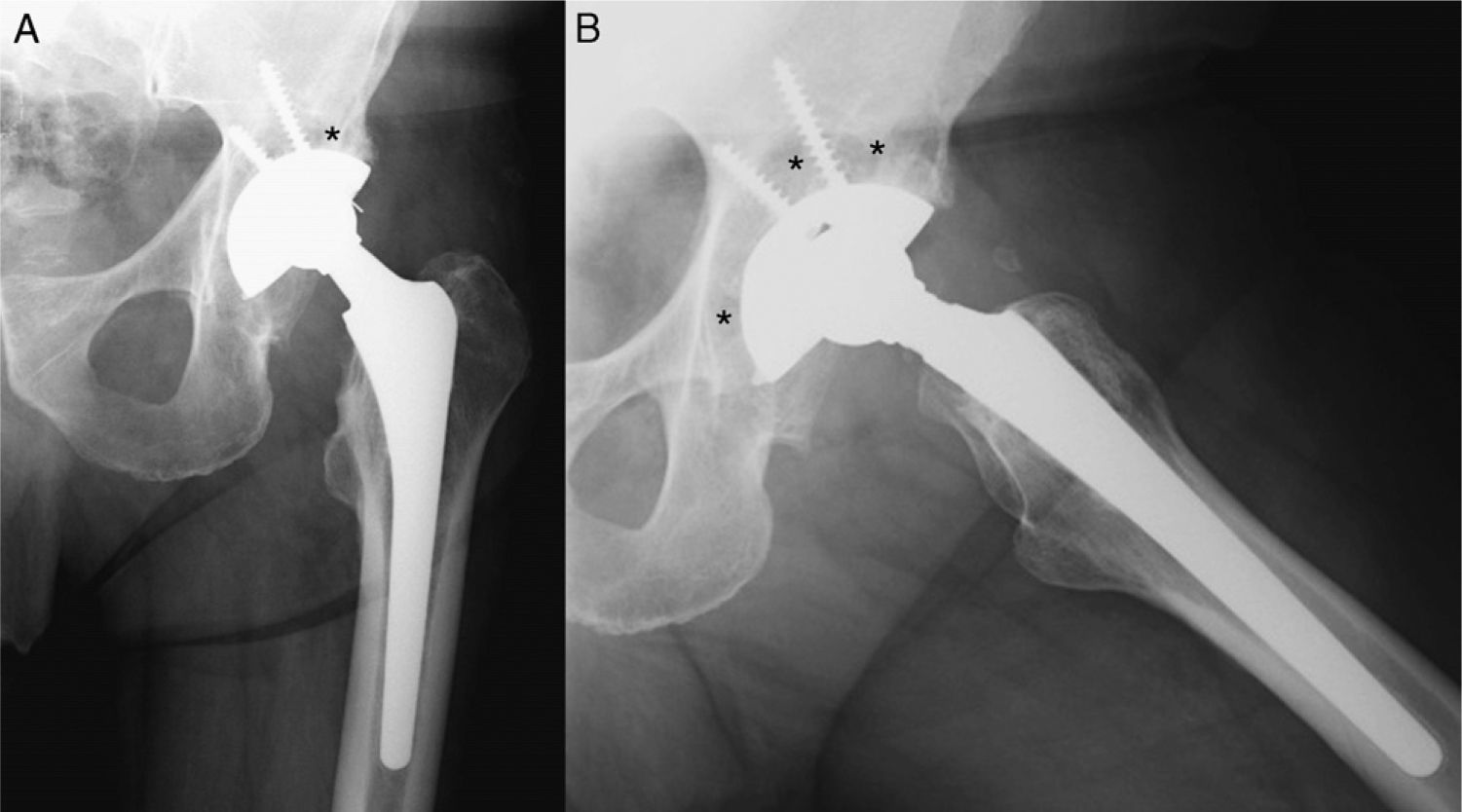
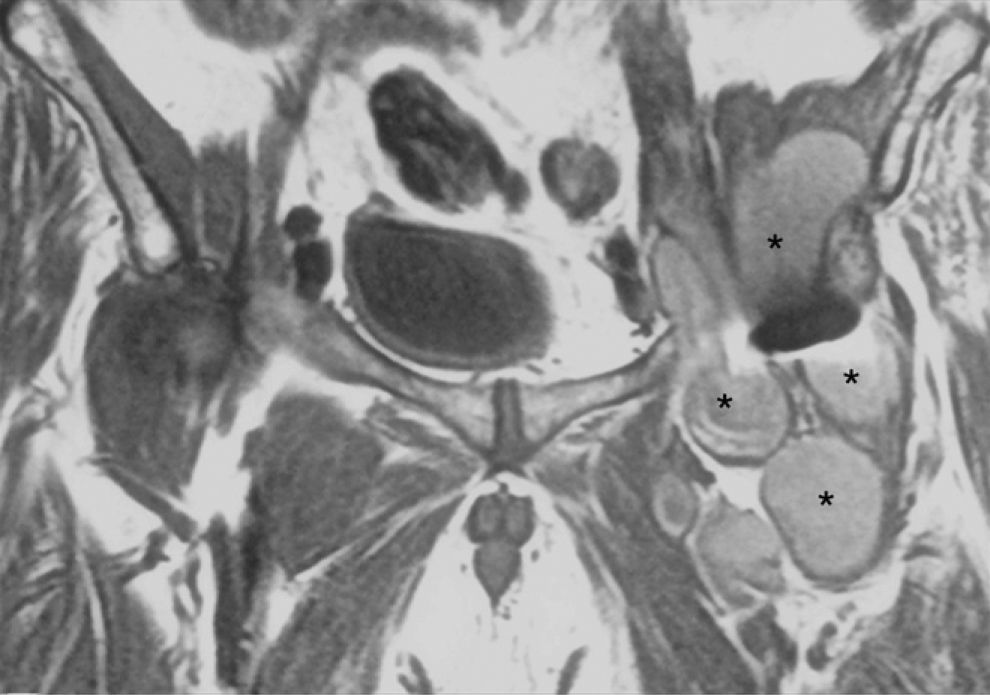
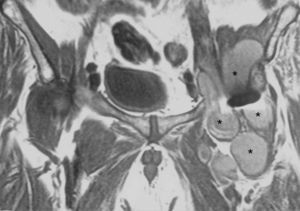
The patient came to the Traumatology clinic for non-radiating pain in the left hip that had begun suddenly more than 2 months earlier and did not subside with analgesic therapy. He was afebrile; physical examination revealed that left inguinal pain was worse on palpation as well as on passive hyperextension and flexion counter-resistance of the left hip. Pain was limiting the range of motion in his hip at the last degrees of all movement arcs. Upon deep palpation, a soft, depressible mass of about 7cm×5cm was detected in the proximity of the femoral artery, with no bowel sounds on auscultation. There were no inguinal adenopathies or hernias in this area. Ancillary studies were done. On simple anteroposterior and axial X-rays of the hip, polyethylene wear and signs of periacetabular osteolysis were appreciated (Fig. 1). Ultrasound examination revealed a cyst approximately 7cm in diameter in the proximity of the THR. Computerized axial tomography (CAT scan) of the pelvis showed a large lobulated cystic swelling, about 7cm in diameter, in the left iliac fossa (Fig. 2). Magnetic resonance imaging (MRI) showed a 15cm×8-cm multilobulated cystic mass between the THR and the deep plane of the iliac muscle, following the iliac and femoral artery vascular axis and extending toward the greater trochanter. Cyst content was heterogeneous, with hyperintense foci on T1 and no signal changes in the surrounding tissues (Fig. 3). A fine-needle puncture-aspiration (FNPA) of the cyst was done for studies in anatomical pathology and microbiology. The specimen was serosanguinous with lymphocytes and plasmatic cells, indicating a granulomatous reaction to the release of polyethylene particles; the microbiology report was negative.
Magnetic resonance image (T1-weighted coronal slice of pelvis). Multilobulated 15cm×8-cm cystic mass (*), with heterogeneous content and hyperintense foci, between the total hip prosthesis (central black artefact) and the deep plane of the iliac muscle, following the iliac and femoral artery axis.
Compression of the mass against the superficial femoral vein caused the venous thrombosis that was evaluated through echo-Doppler study of the lower extremity. Subsequently, a pulmonary thromboembolism (PTE) occurred, confirmed by helical CAT scan, for which the patient required placement of a vena cava filter.
The decision was made to intervene surgically for revision of the total hip prosthesis and drainage of the cystic mass. In view of the fact that, according to the imaging studies, (1) there was evidence of polyethylene wear and suspicion of acetabular loosening and (2) the multilobulated mass extended from the greater trochanter to the deep plane of the iliac muscle, the Hardinge approach – the one usually used for revision hip surgery at our hospital – was planned for the revision procedure. Upon reaching the greater trochanter and disinserting the gluteus medius, a portion of the mass appeared; the contents, yellowish in color, were aspirated, and specimens were taken for microbiological analysis. After the cyst was emptied, the walls of the mass were partially resected until good exposure of the prosthetic components was achieved. It was impossible to resect the entire mass because of its multilobulated morphology and because it extended behind the iliac muscle toward femoral artery and vein territory; however, several specimens of the cyst wall were sent for anatomical pathology study. As for the arthroplasty revision surgery, polyethylene wear was confirmed, and metallic reaction was noted in the exterior coating of the femoral head, not affecting the rod's cone (Fig. 4), so we proceeded to replace the femoral head (Cr–Co) and polyethylene (high-molecular-weight) insert. The acetabulum and prosthetic femoral rod showed good osseointegration, despite the radiographic signs of periacetabular osteolysis.
The microbiology report ruled out the presence of infection, and the anatomical pathology report confirmed that there was foreign body reaction due to polyethylene particles. The post-operative diagnosis was psoas bursitis secondary to polyethylene particle disease. Having confirmed the diagnosis and treated the cause of the bursitis, we decided not to make an ilioinguinal incision, at this time, to finish excising the bursa from the iliac muscle. The patient's post-operative course was without incident, and he remains asymptomatic after 2 years.
DiscussionCyst formation caused by polyethylene disease following total hip replacement is rare.3 It was reported for the first time by Kolmert et al.4; subsequently, Steinbach et al.5 and Berquist et al.6 reported on 6 and 12 cases, respectively, of bursitis of the iliopsoas muscle.
Polyethylene wear particles exert considerable biological action, triggering a reactive cascade in the tissues that activates the foreign body response, in which macrophages react to the particles with apoptosis and release of cytokines that induce osteoclastogenesis.7 This cascade would result in excessive synovial fluid formation, the increased pressure from which would, in turn, cause hypertrophy of the villi in the synovial membrane of the psoas bursa.8,9 The direction in which and degree to which the bursa stretches determine the clinical symptoms. There could be pain in the anterior aspect of the hip, an ilioinguinal mass, hip flexion, resistance to hip extension, snapping hip, or compression of adjacent abdominal or retroperitoneal structures,10,11 such as the femoral vein compression and thrombosis that other authors have described.2,12,13
The differential diagnosis includes inguinal or crural hernia, lymphoma or other neoplasm, lymphadenopathies, cryptorchidism, abscess of the psoas, and vascular anomalies.12,13 If a pelvic mass is found in a patient who has had a THR, simple X-rays should be taken as ancillary studies to look for signs of underlying joint pathology, polyethylene wear, and osteolysis in the periacetabular or trochanteric region.3 Ultrasound is the best method for initial evaluation of an ilioinguinal mass14 and best detects its septations, showing a lucent structure lateral to the femoral vessels and in front of the hip that may extend to the retroperitoneal space. MRI is the best way to estimate its size and, by delimiting the region's anatomy, can also determine how far the process extends and its relationship to the hip,1 presenting it as a cystic mass with thin walls and peripheral contrast enhancement.15 Doppler is useful in that it excludes aneurysms and vascular conditions.8 On the CAT scan, it appears as a fine-walled, well-defined mass, with the density of water, displacing adjacent structures.16,17 In case of uncertainty, arthrography of the hip may complete the diagnosis by indicating the communication between the hip joint and the psoas bursa.18 Lastly, histology and microbiology studies may determine the cause of the psoas bursitis (whether it is mechanical, infectious, etc.).
A cystic mass in the coxofemoral joint that is causing pain and loss of range of motion, with signs of prosthetic loosening or symptoms of compression of adjacent structures, must be removed.2,9,19 Surgical treatment must be aimed at the cause of the cyst's appearance; in the case of particle disease, this will require that the polyethylene be replaced. There was no aseptic loosening in the case we have presented, so we resected the inguinal mass and replaced the prosthetic polyethylene, thereby resolving the patient's symptoms.
Evidence levelEvidence level V.
Conflicts of interestThe authors have no conflicts of interest to declare.
Ethical DisclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of Data. The authors declare that no patient data appears in this article.
Right to privacy and informed consent. The authors declare that no patient data appears in this article.
Please cite this article as: Lax Pérez R, et al. Trombosis de la vena femoral superficial por gran bursitis en psoas secundaria a enfermedad de las partículas en artroplastia total de cadera. Rev Esp Cir Ortop Traumatol. 2012;56(1):54-58.