To evaluate the results and complications of flexor tendon repair in which a home-based rehabilitation program was utilised without the assistance of a hand therapist during the first 4postoperative weeks.
Materials and methodsBetween July 2009 and July 2014, a total of 21 digits in 15 patients were treated in our institution for complete laceration of the flexor tendons within the flexor pulley system (zone 1 and 2). Passive and active exercises performed by the patients themselves were started the morning after the operation. Data, as range-of-motion and complications, were collected 6months after the surgery.
ResultsFifteen digits had full recovery of flexion. One patient suffered a rupture in the fifth postoperative week. Ten of the 21 digits developed a flexion contracture of the proximal interphalangeal joint; in 5 the contracture was less or equal to 10° without impairment of function or aesthetics.
DiscussionOver recent decades, specialised hand therapy has been of great importance in the postoperative treatment of hand diseases. Unfortunately, these professionals are not always available in our area in the first days after surgery. With this protocol, the patient is in charge of carrying out the postoperative exercises, which could lead to a worse final result and a higher rate of complications.
ConclusionThe home-based rehabilitation program yielded complete recovery of joint mobility in most cases with a low complication rate.
Evaluar resultados y complicaciones de la reparación de tendones flexores en un programa de rehabilitación domiciliario sin la asistencia de un terapeuta de mano durante las primeras 4semanas postoperatorias.
Material y métodosEntre julio de 2009 y julio de 2014, un total de 21 dedos en 15 pacientes fueron tratados en nuestro centro por una lesión completa de tendones flexores en la zona del sistema de poleas (zonas 1 y 2). Ejercicios pasivos y activos de rehabilitación, ejecutados por el propio paciente, se empezaron la mañana siguiente a la operación. Los datos de movilidad y complicaciones fueron recogidos 6meses después de la intervención.
ResultadosQuince dedos tuvieron recuperación completa de la flexión. Un paciente sufrió una rotura en la quinta semana postoperatoria. En 10 de los 21 dedos se presentó una contractura en flexión de la articulación interfalángica proximal; en 5 la contractura fue de 10° o menos, sin afectar la función ni la estética.
DiscusiónLa terapia de mano especializada ha sido de gran importancia en el tratamiento postoperatorio de las dolencias de la mano. Desafortunadamente, en nuestro medio, es frecuente que estos profesionales no estén disponibles en los primeros días tras la intervención. Con este protocolo, el paciente asume la responsabilidad en la ejecución de los ejercicios, lo que podría conllevar un peor resultado final y un aumento en la tasa de roturas.
ConclusiónEl programa de rehabilitación domiciliaria proporcionó la recuperación completa de la movilidad articular en la mayoría de los casos, con un bajo número de complicaciones.
In the repair of flexor tendon injuries, even though the surgical technique is the best possible, the final result can be poor due to the appearance of adherences at the suture site during the postoperative period. To avoid such adherences, the rehabilitation is fundamental, constituting one of the main treatment mainstays, together with a non-invasive surgical technique and proper management of the pulley system.
Immobilisation after flexor tendon surgery is traditionally associated with poor results due to the rigidity, loss of sliding function, and joint contractures, mainly in the pulley system area.1,2 In 1967, Kleinert et al.3 reported their 10-year experience with an early passive mobility protocol for after primary repair of flexor tendon injuries with which they achieved full recovery of range of motion in all fingers. Since then, there has been a significant effort to improve rehabilitation protocols and increase repair strength with more resistant suture materials and configurations.4 From the beginnings of the 1960s on, experimental5 and clinical6,7 studies have shown the benefits of controlled active mobility protocols.
In spite of all the advances in rehabilitation programmes, it is still difficult to achieve good range of motion in the proximal interphalangeal (PIP) and distal interphalangeal (DIP) joints.8 In some areas, many patients cannot begin an early exercise programme because the rehabilitation centres are overburdened. Due to the lack of physiotherapist availability, some surgeons prefer to immobilise their patients following flexor tendon repair, accepting a less than optimum result. Other possible reasons for adopting this attitude are insufficient communication between the surgeon and the hand therapist and a lack of confidence in patients’ ability to carry out a home-based rehabilitation protocol because of fear of postoperative ruptures.
An early active mobility protocol to prevent adherences and rigidity and the shortage of specialised professionals in the first days after the operation are decisive. For that reason, we have developed a home-based rehabilitation protocol for patient use without the assistance of a hand therapist during the first 4 postoperative weeks. The objective of our study was to assess the results and complications of patients receiving flexor tendon repair on whom this home-based rehabilitation programme was applied.
Materials and methodsThis was a retrospective cohort study. Between July 2009 and July 2014, a total of 21 fingers in 15 patients were treated in our centre for complete laceration of the flexor tendons in the flexor pulley system (Zones 1 and 2). Children younger than 10 years old and patients with associated fractures, reimplantations or revascularisations were excluded. Patients with lacerations to the flexor pollicis longus were also excluded, due to the differences between the protocols applied and the measurement of the final results. All the patients in this series were capable of understanding and performing the postoperative exercises.
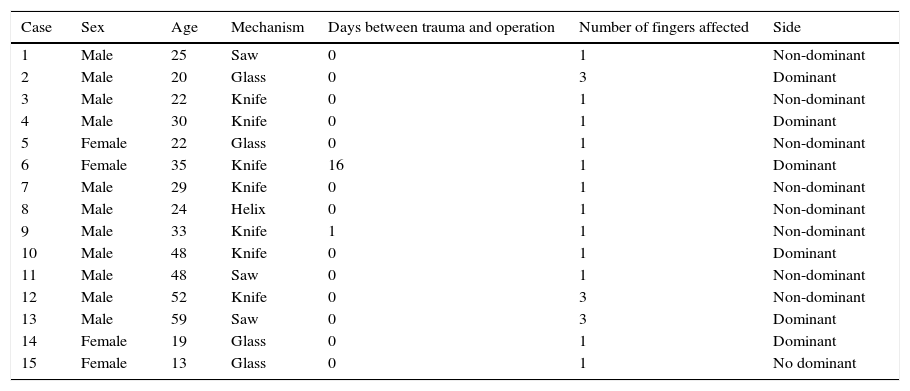
Table 1 presents the demographic variables and trauma mechanism. Mean age was 29 (range between 13 and 59 years), with a distribution by sex of 11 males and 4 females. Three patients had 3fingers involved (8 fingers in Zone 2 and 1 in Zone 1). The others had only 1 finger affected: 3 in Zone 1 and 9 in Zone 2 (Table 2). All of the patients that had Zone 2 involvement had lacerations in both tendons, superficial and deep. There were 14 fingers with an associated injury to the digital collateral nerve (12 had 1 nerve affected and 2, both nerves) and 12 fingers with 1 of the collateral arteries injured. The cases in which both arteries were repaired (revascularisation) were excluded because the fingers were immobilised for 14 days and this rehabilitation protocol was not applied.
Demographic data for 15 patients with acute flexor tendon injuries.
| Case | Sex | Age | Mechanism | Days between trauma and operation | Number of fingers affected | Side |
|---|---|---|---|---|---|---|
| 1 | Male | 25 | Saw | 0 | 1 | Non-dominant |
| 2 | Male | 20 | Glass | 0 | 3 | Dominant |
| 3 | Male | 22 | Knife | 0 | 1 | Non-dominant |
| 4 | Male | 30 | Knife | 0 | 1 | Dominant |
| 5 | Female | 22 | Glass | 0 | 1 | Non-dominant |
| 6 | Female | 35 | Knife | 16 | 1 | Dominant |
| 7 | Male | 29 | Knife | 0 | 1 | Non-dominant |
| 8 | Male | 24 | Helix | 0 | 1 | Non-dominant |
| 9 | Male | 33 | Knife | 1 | 1 | Non-dominant |
| 10 | Male | 48 | Knife | 0 | 1 | Dominant |
| 11 | Male | 48 | Saw | 0 | 1 | Non-dominant |
| 12 | Male | 52 | Knife | 0 | 3 | Non-dominant |
| 13 | Male | 59 | Saw | 0 | 3 | Dominant |
| 14 | Female | 19 | Glass | 0 | 1 | Dominant |
| 15 | Female | 13 | Glass | 0 | 1 | No dominant |
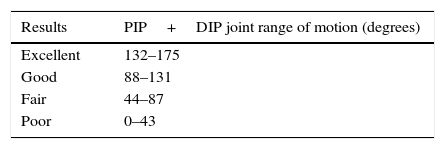
Modified Strickland and Glogovac criteria.
| Results | PIP+DIP joint range of motion (degrees) |
|---|---|
| Excellent | 132–175 |
| Good | 88–131 |
| Fair | 44–87 |
| Poor | 0–43 |
DIP, distal interphalangeal; PIP: proximal interphalangeal.
Source: Taken from Strickland and Glogovac.16
All the patients were operated on in less than 24h after the trauma, except for 1-patient that had surgery 16 days after it. All the repairs were performed by the same surgeon.
Surgical techniqueFollowing appropriate cleaning and debridement, the injury was extended distally in zigzag to the distal end of the tendon, always avoiding the formation of flaps with angles less than 90°. The end of the proximal tendon was recovered with a mosquito-type forceps inserted into the tendon sheath. If this manoeuvre was unsuccessful, the tendons were located with an additional transversal palm incision and were slid distally using 2Adson forceps (“worm” manoeuvre). It was unnecessary to use another manoeuvre to recover the tendons in the surgical repair site in any cases.
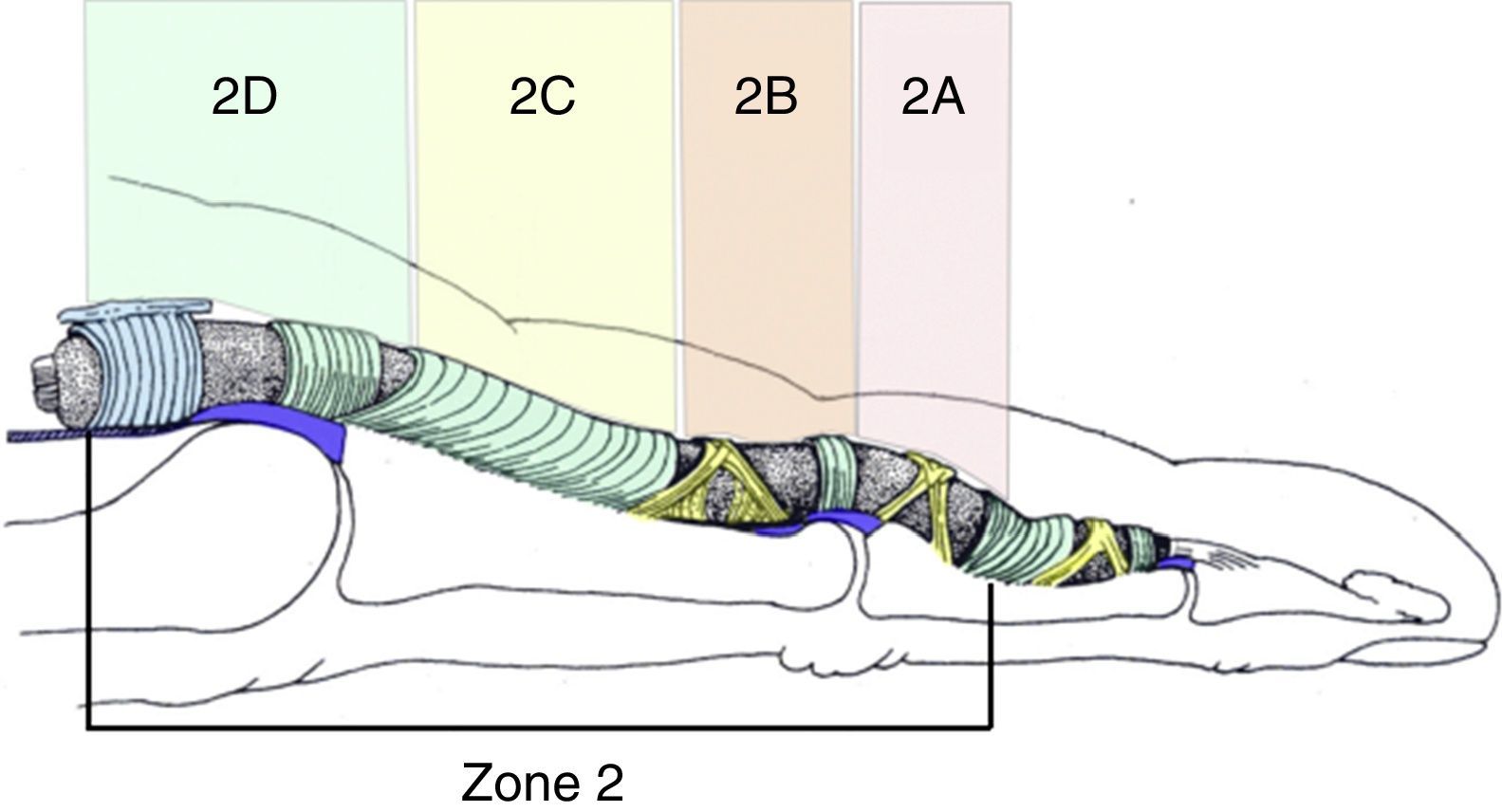
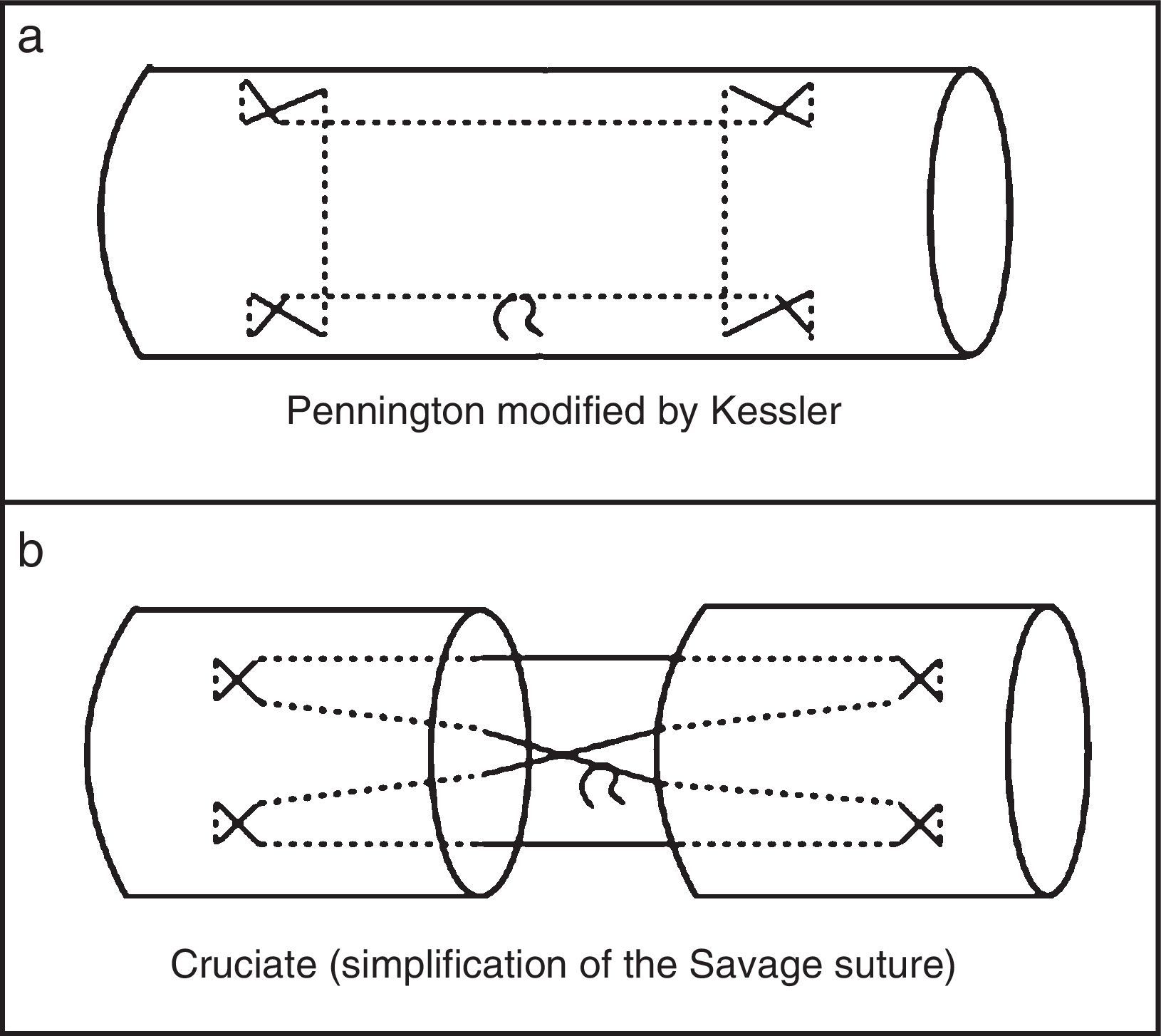
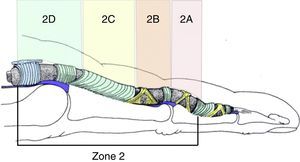
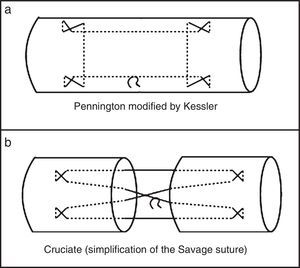
The criteria for superficial flexor tendon repair were the size of distal end available for suture and the excursion of the deep flexor tendon seen after the repair. If the sutures of the superficial tendon obstructed the excursion of the deep tendon, they were removed together with part of the superficial flexor. A band of the superficial tendon was sutured in 7 patients and the 2 bands in another 6 patients. In 4 patients, the repair was carried out in more proximal zones (Tang and Shi9 Zones 2C and 2D) (Fig. 1); while in 2 patients, the suture was removed after checking deep tendon excursion. The superficial flexor bands were repaired with a 5-0 polypropylene suture in a type of Kessler-modified Pennington configuration with additional locking10 (Fig. 2a). For lacerations in more proximal areas of the superficial tendon, the suture technique was the same as that used in the deep flexor tendon. Deep flexor tendons were repaired with a central 4-0 polypropylene Cruciate-type suture with 4 strands (a simplification of the 6-strand suture proposed by Savage11) (Figs. 2b and 3) and a simple 6-0 polypropylene epitendinous suture.
Zone 2 subdivision proposed by Tang and Shi.9
In spite of the fact that braided polyester (Ethibond®) has greater cut resistance than polypropylene (Surgipro™),12 we used polypropylene because it makes sliding and tension adjustment in suturing easier and generates similar resistance.13 All the repair configurations were compatible with a controlled active mobility protocol.14
In the postoperative period, the hand was immobilised with a dorsal splint to block the extension of the metacarpophalangeals at 70° and the PIP and DIP joints at 0° (Fig. 4a). The wrist was left in a neutral or slightly extended position.15 Rehabilitation exercises began on the morning after the operation, when the splint was readjusted to leave the palmar side of the fingers free in such a way that the patient could touch the palm of the hand with the fingertips. Two types of exercises were used: passive and active. Active exercises were introduced only after the patient understood and could perform the passive ones correctly.
Rehabilitation protocolPassive exercisesPatients were taught to move all the fingers (except for the thumb, but including the non-injured fingers) of the affected hand using the contralateral hand. The first exercise was passive flexion and extension of the PIP and DIP joints, the goal being to touch the palm of the hand with the fingertip, seeking complete passive flexion. Each finger was exercised individually. Extension came after the flexion, emphasising the importance of extending the PIP joint completely while the metacarpophalangeal joint was flexed at 90°. (It is easier to begin with uninjured fingers because the first movements of the fingers affected usually cause pain and frustration. At that time, it is important for the physician to emphasise that pain will decrease significantly after a few repetitions.) Patients were instructed to execute a minimum of 50 repetitions for each finger every hour. The objectives of the passive exercises were to soften the joints and facilitate tendon slide, and were important to avoid ruptures that might occur with active exercises; the active exercises were started only after verifying that the patient was capable of correctly performing the passive ones.
Active exercisesPatients were instructed to flex all the fingers completely at the same time in a passive manner with the aid of the contralateral hand. Next, patients took the contralateral hand away and were asked to keep the fingers flexed actively for 5s, using the minimum effort to hold the fingers in this position. Patients then relaxed and extended the fingers actively up to the splint limits. A total of 3 repetitions of active exercises were performed every half hour after the passive ones.
At the end of each session, the lacerations and the palm of the hand were covered with a dressing pad and adhesive tape to keep the interphalangeals in full extension inside the splint (Fig. 4b).
Follow-upFollowing the initial training session, patients were discharged and followed up twice a week for treatment, splint change if applicable, and supervision and correction of the exercises as needed. The splint was removed 4 weeks after the operation and free hand movement was permitted, avoiding excess effort during the first 12 weeks. All patients were advised to avoid active DIP range-of-motion exercises with the PIP joint blocked during the first 8weeks and to avoid gripping a rubber ball for 12 weeks. In patients that developed a flexion contracture of the PIP joint, a dynamic extension splint for night use was ordered following the sixth week (Fig. 5).
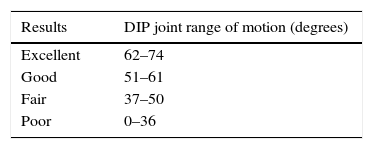
After 6 months, PIP and DIP range of motion was measured using a goniometer and complications (ruptures, adherences and contractures in PIP flexion) were recorded. In Case 13, the measurements were taken 3 months after tenolysis. Modified Strickland and Glogovac criteria16 were used for injuries in Zone 2 (Table 2), with Moiemen and Elliot17 criteria for those in Zone 1 (Table 3).
Moiemen and Elliot criteria.
| Results | DIP joint range of motion (degrees) |
|---|---|
| Excellent | 62–74 |
| Good | 51–61 |
| Fair | 37–50 |
| Poor | 0–36 |
Source: Taken from Moiemen and Elliot.17
The final result was compared based on mechanism of trauma, zone involved (1 or 2), age, sex, side according to dominance, affected finger and number of fingers involved. To simplify the analysis, the mechanism of trauma was divided into cut injuries (produced by cutting objects such as knives or glass) or contusive injuries (when there was a component of crushing, such as injuries from saws or screws). Non-parametric tests (Mann–Whitney U, Chi-Square and Fisher's Exact tests) were used for the statistical study. The Shapiro–Wilk test was used to evaluate whether the sample was of normal distribution. Statistical significance was set at P<0.05.
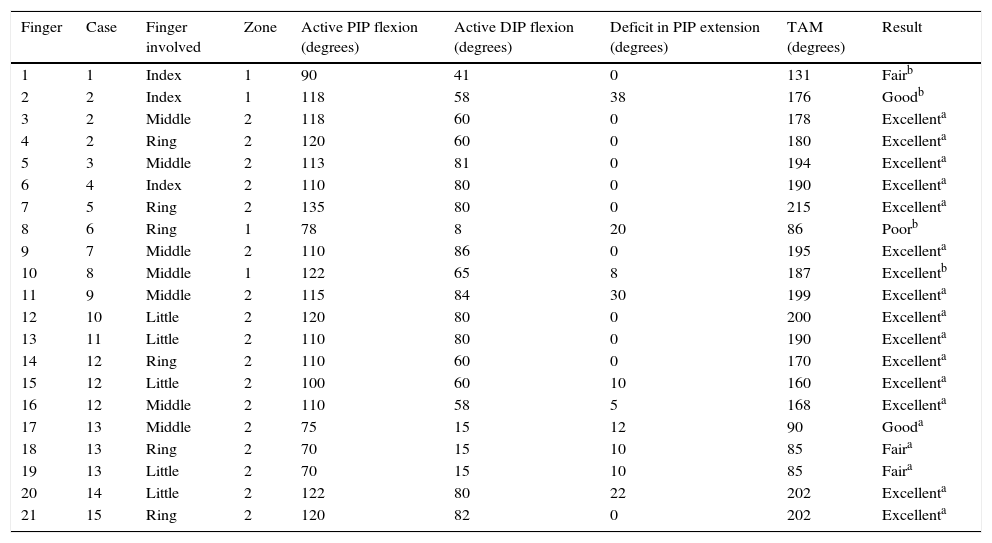
ResultsTable 4 presents the active flexion of the PIP and DIP joints and the deficit in PIP extension for each finger that was operated. For a total of 15 fingers (71%), there was an excellent result, with full recovery of flexion (Fig. 6).
Results of 21 digits in 15 patients.
| Finger | Case | Finger involved | Zone | Active PIP flexion (degrees) | Active DIP flexion (degrees) | Deficit in PIP extension (degrees) | TAM (degrees) | Result |
|---|---|---|---|---|---|---|---|---|
| 1 | 1 | Index | 1 | 90 | 41 | 0 | 131 | Fairb |
| 2 | 2 | Index | 1 | 118 | 58 | 38 | 176 | Goodb |
| 3 | 2 | Middle | 2 | 118 | 60 | 0 | 178 | Excellenta |
| 4 | 2 | Ring | 2 | 120 | 60 | 0 | 180 | Excellenta |
| 5 | 3 | Middle | 2 | 113 | 81 | 0 | 194 | Excellenta |
| 6 | 4 | Index | 2 | 110 | 80 | 0 | 190 | Excellenta |
| 7 | 5 | Ring | 2 | 135 | 80 | 0 | 215 | Excellenta |
| 8 | 6 | Ring | 1 | 78 | 8 | 20 | 86 | Poorb |
| 9 | 7 | Middle | 2 | 110 | 86 | 0 | 195 | Excellenta |
| 10 | 8 | Middle | 1 | 122 | 65 | 8 | 187 | Excellentb |
| 11 | 9 | Middle | 2 | 115 | 84 | 30 | 199 | Excellenta |
| 12 | 10 | Little | 2 | 120 | 80 | 0 | 200 | Excellenta |
| 13 | 11 | Little | 2 | 110 | 80 | 0 | 190 | Excellenta |
| 14 | 12 | Ring | 2 | 110 | 60 | 0 | 170 | Excellenta |
| 15 | 12 | Little | 2 | 100 | 60 | 10 | 160 | Excellenta |
| 16 | 12 | Middle | 2 | 110 | 58 | 5 | 168 | Excellenta |
| 17 | 13 | Middle | 2 | 75 | 15 | 12 | 90 | Gooda |
| 18 | 13 | Ring | 2 | 70 | 15 | 10 | 85 | Faira |
| 19 | 13 | Little | 2 | 70 | 15 | 10 | 85 | Faira |
| 20 | 14 | Little | 2 | 122 | 80 | 22 | 202 | Excellenta |
| 21 | 15 | Ring | 2 | 120 | 82 | 0 | 202 | Excellenta |
DIP, distal interphalangeal; PIP, proximal interphalangeal; TAM, total active mobility (sum of the active flexion of the PIP and DIP joints).
One patient (Case 8) suffered a rupture in the fifth week while performing active DIP flexion exercises with blocked PIP extension (recommended by professionals not connected with our service). The patient was reoperated with 24h of the rupture and treated with the same active range-of-motion protocol: full recover of active flexion of the finger was achieved.
Ten of the 21 fingers presented a PIP flexion contracture. In 5 fingers, the contracture was less than or equal to 10° without affecting function or aesthetics. In 3 fingers, the contracture was between 10° and 30°, which caused an aesthetic problem. In 2patients, the contracture was 38° (Case 1) and 30° (Case 9), respectively. These 2 patients were offered surgical liberation of the contracture, but only 1 of them accepted the procedure (Case 9). In this patient, the palmar plate was free and pulley system integrity was verified; however, in spite of continual night splinting, la contracture recurred at 3 months.
A patient that had 3 fingers affected (Case 13) presented postoperative adherences and was reoperated 128 days after the repair for tenolysis: more than 160° of active range of motion (the sum of PIP and DIP) was achieved in the fingers involved. Another patient (Case 6), who was operated 16 days after a Zone 1 ring finger injury, had a poor result (86° of active flexion [the sum of PIP and DIP]), but rejected reoperation because she felt that her hand function was not worse.
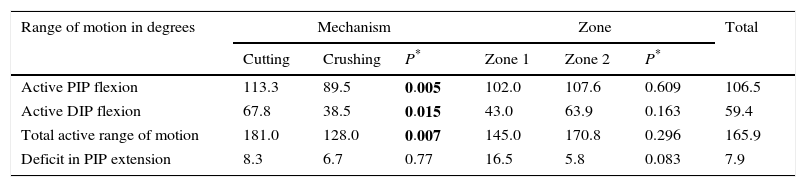
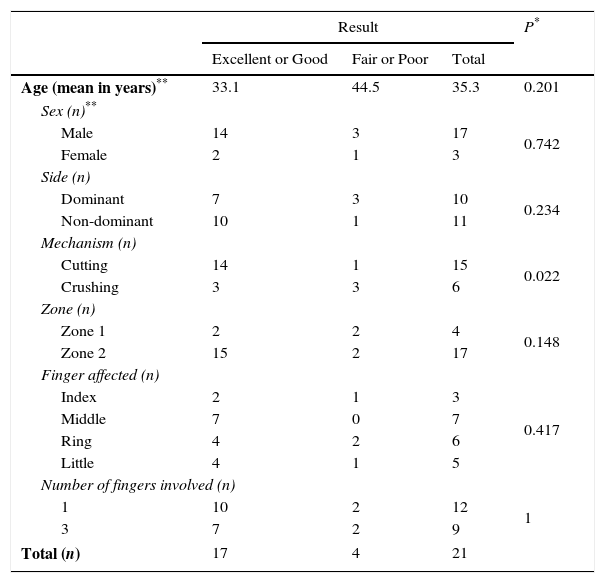
The final active flexion of the PIP and DIP joints was worse in fingers with contusive injuries compared with cut injuries (P=0.007). The mechanism of trauma had no effect on PIP extension deficit. There were no statistically significant differences between patients with injuries in Zones 1 and 2 (Table 5). The analysis of age, sex, side according to dominance, finger affected, number of fingers affected and zone, compared with the final result according to the criteria established did not reveal any statistically significant differences either (Table 6). The sole exception in comparison analysis was the mechanism of trauma, in which the final result was worse with injuries produced by saw or helix (P=0.02).
Average range of motion in degrees based on injury type (mechanism producing it) and zone involved.
| Range of motion in degrees | Mechanism | Zone | Total | ||||
|---|---|---|---|---|---|---|---|
| Cutting | Crushing | P* | Zone 1 | Zone 2 | P* | ||
| Active PIP flexion | 113.3 | 89.5 | 0.005 | 102.0 | 107.6 | 0.609 | 106.5 |
| Active DIP flexion | 67.8 | 38.5 | 0.015 | 43.0 | 63.9 | 0.163 | 59.4 |
| Total active range of motion | 181.0 | 128.0 | 0.007 | 145.0 | 170.8 | 0.296 | 165.9 |
| Deficit in PIP extension | 8.3 | 6.7 | 0.77 | 16.5 | 5.8 | 0.083 | 7.9 |
DIP, distal interphalangeal; PIP, proximal interphalangeal.
Values lower than 0.05 indicated in bold.
Analysis of the characteristics of the affected fingers in relation to the final results for Zone 2 injuries (according to Glogovac and Strickland criteria) and for Zone 1 injuries (Moiemen and Elliot criteria). Age, sex, side and mechanism given by fingers.
| Result | P* | |||
|---|---|---|---|---|
| Excellent or Good | Fair or Poor | Total | ||
| Age (mean in years)** | 33.1 | 44.5 | 35.3 | 0.201 |
| Sex (n)** | ||||
| Male | 14 | 3 | 17 | 0.742 |
| Female | 2 | 1 | 3 | |
| Side (n) | ||||
| Dominant | 7 | 3 | 10 | 0.234 |
| Non-dominant | 10 | 1 | 11 | |
| Mechanism (n) | ||||
| Cutting | 14 | 1 | 15 | 0.022 |
| Crushing | 3 | 3 | 6 | |
| Zone (n) | ||||
| Zone 1 | 2 | 2 | 4 | 0.148 |
| Zone 2 | 15 | 2 | 17 | |
| Finger affected (n) | ||||
| Index | 2 | 1 | 3 | 0.417 |
| Middle | 7 | 0 | 7 | |
| Ring | 4 | 2 | 6 | |
| Little | 4 | 1 | 5 | |
| Number of fingers involved (n) | ||||
| 1 | 10 | 2 | 12 | 1 |
| 3 | 7 | 2 | 9 | |
| Total (n) | 17 | 4 | 21 | |
Over the last decades, specialised hand therapy has been very important in postoperative treatment of hand lacerations. Unfortunately, in our setting, these professionals are frequently unavailable during the initial postoperative days. The fact that adherences form very early during the flexor tendon healing process18 has led us to establish a protocol in which the patients themselves begin rehabilitation exercises 24h after the operation.
In theory, carrying out these home-based exercises might increase the chance of postoperative ruptures, given that the patient could use excessive force, mainly in performing the active exercises. In our series, the rupture rate (5%) is no higher than that published for centres in which hand therapists are available in the first postoperative days.19
For the patient to be able to perform active exercises, it is important to focus on an atraumatic technique and on a repair capable of withstanding the forces generated by active mobility. We feel that a central 4-strand repair using a simple epitendinous suture is sufficient. More complex repairs or those with more strands could increase the strength of the repair; however, they do not appear to help to lower gap formation between the tendon ends20 and could indeed even make it more difficult for tendons to glide within the pulley system.21
In contrast to current preferences,22 we favour to keep the wrist immobilised in a neutral or slightly extended position for a maximum period of 4weeks. The 4-strand repair is strong enough to withstand the forces generated with passive range-of-motion exercises, so keeping the wrist flexed is unnecessary. However, to perform active exercises, wrist flexion is unwise because it increases the passive tension of the extensor tendons.15 We have not used a hinge splint such as that in the Indiana protocol.23 Although it is true that incorporating a hinge encourages flexor tendon excursion on changing wrist position between flexion and extension, using a plaster splint with the wrist in a neutral position seems not to have impacted our patient results negatively.
Many might consider splint removal in the fourth week to be too early because of the risk of rupture in the fifth and sixth postoperative weeks. However, we have had only 1 rupture, which occurred during the performance of active DIP range-of-motion exercises with PIP extension blocked. By blocking the PIP joint, resistance to the active movement that can promote the rupture is increased. That is why we avoid this type of exercise in the first 8 postoperative weeks. The indication for performing this exercise was given in a centre not connected to our service. For that reason, we do not feel it is justified to increase the time the protective splint is used, given that no ruptures occurred in the rest of the patients, who respected the prohibition against any loads in the first 6weeks after the operation.
In reality, home-based exercises form part of the majority of physiotherapy protocols. The main difference is that, under ideal circumstances, the hand therapist is in charge of the initial postoperative treatment steps within a daily programme: treatment, splinting and range-of-motion exercises. After a physiotherapy session, in which the exercises are repeated several times with the help of a therapist, the patient can leave with greater confidence to continue the mobility treatment at home. In our protocol, as there is no therapist present during the first weeks, the patient takes responsibility for exercise performance from the start.
The success of a home-based rehabilitation protocol depends on the patient's management capability. A key role in this process can be the motivation that the surgeon can transmit to the patient. The ability to understand and to perform the postoperative exercises, as well as the capacity to manage the injury in the initial healing stages, are also important. We have found that well-motivated patients with a high education level have fewer difficulties, as it is not so necessary to repeat and correct the exercises during postoperative visits.
We have been conscientious in seeking full extension of the PIP joint from the beginning of postoperative rehabilitation. Even so, 10 of the 21 fingers evolved with an extension deficit that did not totally improve with using the dynamic extension splint initiated following the sixth week after the operation. It is difficult to motivate patients to extend the joint completely due to the pain produced when the injury is stretched in the initial days of the postoperative period. With the aid of a hand therapist, a more personalised manipulation and proper passive splinting initiated during the first week would probably help to avoid this complication. However, the contracture was seen clinically in only 4 of our patients. Of these 4 patients with contracture equal to or more than 20°, surgical review was justified in just 2 (with more than 30° of contracture) and only 1 accepted the operation.
Insufficiency of the flexor pulley system could also be the reason behind residual contracture of the PIP joint. This flexion contracture and bow-stringing are typical findings in multiple pulley rupture, principally with joint involvement of A2 and A4.24 This happens due to imbalance of the forces in the joint, where the flexors prevail over the extensors from the increase in the lever arm (the distance between the tendon and the centre of joint rotation). In our patients, we believe that this was not the reason for the PIP flexion contracture, given that preserving maximum pulley system integrity was sought during dissection. We have based this on the fact that the opening of up to 3 pulleys (considering that A2 is equivalent to 2 pulleys) does not cause bow-stringing or an appreciable loss of excursion.25 This is because, in most cases, removing a small segment of the pulley system is required to prevent friction in the repair and its edges.
Although there is bibliographic evidence that results worsen in older patients, involvement of the little finger, delay in operating26 and zone affected,17 we found no statistically significant differences on analysing these factors in our study. The reason for this is probably the reduced number of cases, which is the main limitation of this study. The other is the lack of a control group, in which patients were taught by a hand therapist during the rehabilitation process. Our results could set the stage for comparative studies, in which the population available would be able to understand and undertake the rehabilitation exercises.
In spite of the fact that there were no statistically significant differences between patients with lacerations in Zones 1 and 2 (P=0.163), mean active flexion of the DIP joint was greater in patients with Zone 2 injuries (63.9°). This indicates a tendency for there to be worse results in patients with injuries in Zone 1 (43°), as Moiemen and Elliot noted.17 It is possible that, by introducing adjustments in our rehabilitation protocol, paying more attention to DIP joint mobility, we could improve results.
One of our patients with a Zone 1 laceration was operated 16 days after the trauma. In this case, operating delay might be a more determining factor in causing a final poor result. Rigo and Røkkum25 did not find any statistically significant differences in 23 patients having direct repair surgery 14 days or more after the injury. However, we feel that this indication should have been taken much more cautiously, given that excessive tension could cause a gap in the repair and, consequently, adherences.
Likewise, the injuries from saws or helixes can cause more fibrosis and adherences in the repair site, which justifies the fact that there were worse results in our patients (Tables 5 and 6). Of the 6 fingers with saw lacerations sierra, 3 achieved a fair result. These patients might have improved more with rehabilitation overseen from the start, but other factors (such as trauma severity) could have been more determinative in the loss of mobility of these fingers.
In this case series, transferring responsibility for rehabilitation to the patient yielded full recovery of joint range of motion for the majority, with few complications. However, home-based rehabilitation is not what is ideal. It is viable and acceptable only when the structure of the healthcare system organisation makes it impossible to immediately institute physiotherapy given by specialised hand therapists that communicate well with surgeons.
Level of evidenceLevel of evidence IV.
Ethical disclosuresProtection of persons and animalsThe authors declare that no experiments have been carried out on human beings or animals for the purpose of this research.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre about the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Conflict of interestsThe authors have no conflicts of interest to declare.
Please cite this article as: Sanmartín-Fernández M, Fernández-Bran B, Couceiro-Otero J. Rehabilitación domiciliaria en el tratamiento postoperatorio de la reparación de los tendones flexores. Rev Esp Cir Ortop Traumatol. 2017;61:224–232.