The proximity of the posterior horn of the lateral meniscus to the popliteal artery determines a risk of vascular injury in its suture. The aim of this study is to determine the location of the popliteal artery, and to establish the minimal distance from the posterior wall of the lateral meniscus to the artery, the common peroneal nerve (CPN), and its correlation to other variables.
Material and methodsA total of 102 magnetic resonance studies were retrospectively reviewed from patients undergoing surgery at our institution. The axial section where the lateral meniscus could be clearly defined was selected, and the measurements were performed.
ResultsThe artery lay laterally to the midline in 94% of the cases. The minimal mean distance from the posterior wall of the lateral meniscus to the popliteal artery was 1.01cm (0.32–1.74, SD: 0.304). The minimal mean distance to the CPN was 1.74cm (0.75–2.87, SD: 0.374). No association was found between the minimal mean distance from the posterior wall to the popliteal artery with the height, weight, BMI, the lateral meniscus diameter, or the tibial plateau diameter. An association was found between the distance from the posterior wall to the CPN with the weight and the BMI.
ConclusionsThe proximity of the posterior horn to the popliteal artery should be considered when performing sutures. This distance is within the recommended depth for all-inside meniscus repair devices. This distance is not related to height, weight, BMI, lateral meniscus nor tibial plateau diameters.
La proximidad del cuerno posterior del menisco externo a la arteria poplítea condiciona un riesgo de lesión vascular en su sutura. El objetivo es definir la localización de la arteria poplítea, establecer la distancia mínima del muro posterior del menisco externo a la arteria, al nervio ciático poplíteo externo (CPE) y su correlación con otras variables.
Material y métodoSe revisaron retrospectivamente 102 resonancias magnéticas nucleares de pacientes operados en nuestro centro. Se seleccionó el corte axial donde se identificase adecuadamente el menisco externo y se realizaron el conjunto de mediciones.
ResultadosLa arteria se localizó lateral a la línea media antero-posterior en el 94% de los casos. La distancia mínima media del muro posterior del menisco externo a la arteria poplítea fue de 1,01cm (0,32–1,74, SD: 0,304). La distancia mínima media al CPE fue de 1,74cm (0,75–2,87, SD: 0,374). No se encontró una correlación de la distancia del muro posterior a la arteria poplítea con la altura, el peso, el IMC, el diámetro del menisco externo ni el diámetro de la meseta tibial. Se encontró una correlación entre la distancia del muro posterior al CPE con el peso y el IMC.
ConclusionesLa proximidad del muro posterior a la arteria poplítea debe ser tenida en cuenta a la hora de realizar suturas. Esta distancia está dentro de la profundidad recomendada en los dispositivos de sutura «todo-dentro» y no está en relación con la talla, el peso, el IMC, el tamaño del menisco externo ni la meseta tibial.
It has been proven that joint degeneration is frequent and takes place rapidly after an external meniscectomy.1 This is due to the alteration in the load distribution of the knee that is produced following the intervention, where the severity is directly related to the amount of meniscus excised.2 The stability and function of the knee following a reconstruction of the anterior cruciate ligament (ACL) is conditioned by the preservation of the menisci.2
Thus, it is essential to preserve the menisci by carrying out repairs in those cases where the characteristics of the tear allow it. Performing meniscectomies in tears that can be repaired by suture is firmly contraindicated. The number of meniscal sutures performed with “all-inside”3 arthroscopic systems has increased in recent years, as these are less invasive than “inside–outside” suture techniques.
The popliteal artery is a structure that can be affected by these procedures, due to its anatomical proximity to the posterior horn of the external meniscus. Although the reported incidence of vascular lesions is low, it is likely that real incidence is higher. The sequelae observed once a complication of this type takes place are significant and include pseudoaneurysms, fistulas, need for secondary interventions and a high rate of amputation, which can sometimes reach up to 66%.4,5 Most published series on the incidence of vascular lesions only mention knee arthroscopies or meniscectomies generically, so the incidence could be higher in cases of meniscal sutures.6
The objective of this work is to define the location of the popliteal artery, establish the minimal distance from the posterior wall of the external meniscus to the popliteal artery, to the common peroneal nerve (CPN) and its correlation with weight, height, body mass index (BMI), the diameter of the external meniscus and the tibial plateau; studying whether this distance is altered by the presence of a Baker cyst or a tear of the ACL and comparing these distances to the depth recommended by various “all-inside” meniscal suture devices.
Material and methodsA total of 102 magnetic resonance imaging (MRI) scans were retrospectively reviewed. These scans corresponded to the knees of patients with different diagnoses who were surgically treated at our hospital consecutively between 2012 and 2014.
The preoperative MRI images were obtained using a 3-Tesla Philips Achieva (Philips Medical Systems, Best, The Netherlands) device. We analyzed the axial sections obtained through proton density sequences with fat suppression (SPAIR sequences), with a repetition time of 5917ms and an echo time of 30ms. The width of the sections was 3mm, with a 0.3mm gap between sections and a 500×355 matrix. We selected those axial sections which offered an adequate visualization of the external meniscus.
We excluded from our study those patients with “bucket handle” tears of the external meniscus, as they did not allow an adequate location of the necessary references to carry out measurements, as well as patients with multi-ligament lesions, as the location of the popliteal artery could vary in these cases due to an abnormal displacement of the tibia relative to the femur.
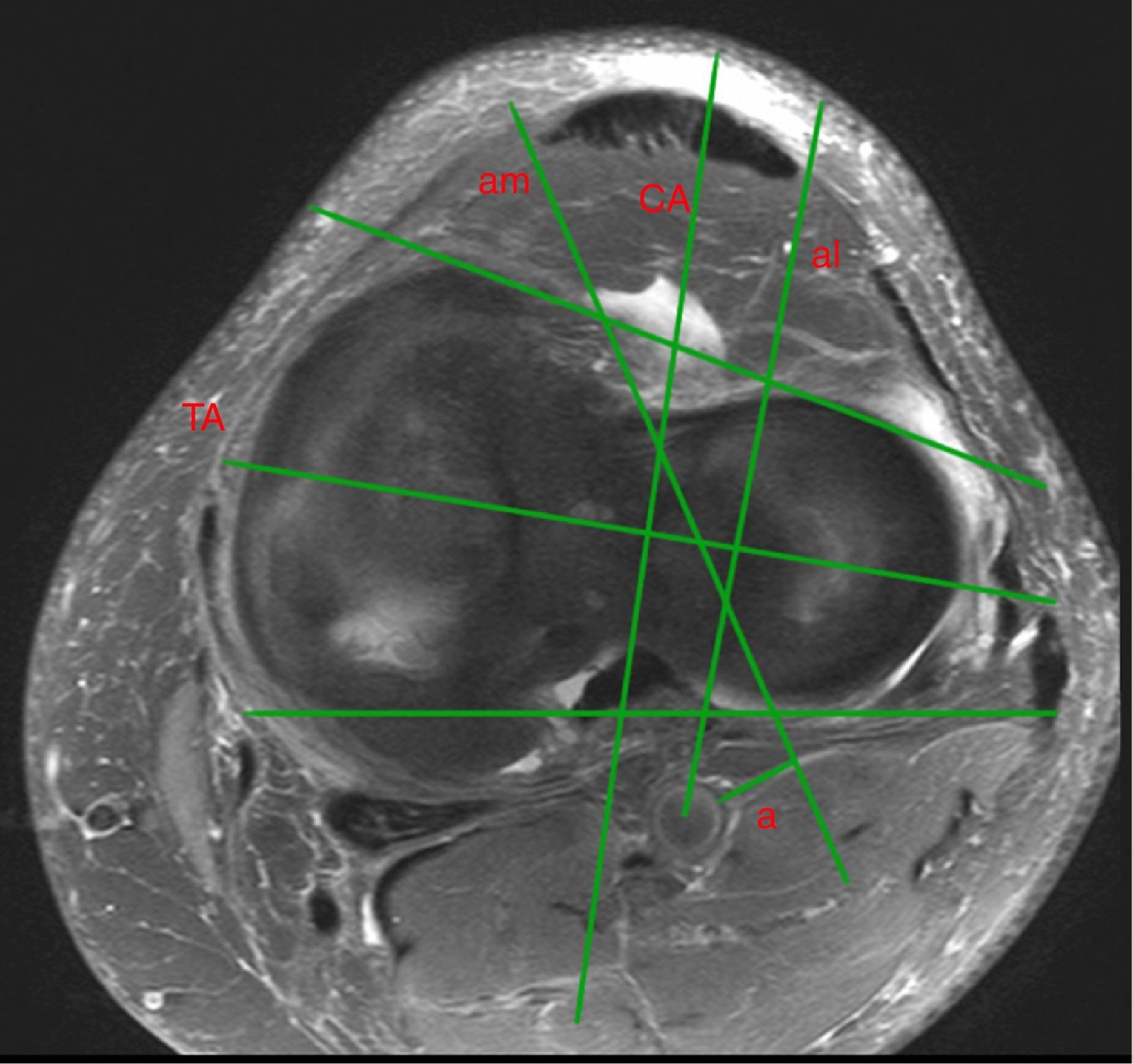
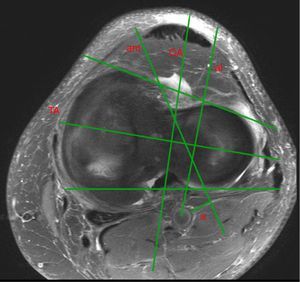
Following the description of Ninomiya,7 we traced two tangential lines to the anterior and posterior edges of the tibial plateau. Next, the bisector of both lines was traced at the level of the most prominent points, both medially and laterally, of the tibial plateau (TA) and the anteroposterior midline perpendicular to this line (CA) was also traced. We then located the popliteal artery, CPN, popliteal hiatus, meniscal wall and free edge of the external meniscus (Fig. 1).
Axial section in SPAIR sequence of the left knee. Tangential lines to the anterior and posterior edges of the tibial plateau, bisector of both lines (TA) and the perpendicular to TA (CA). Lines following the direction of the anteromedial and anterolateral portals to determine the accessibility of the popliteal artery from these portals. Mean minimum distance from the AM portal axis to the popliteal artery (a).
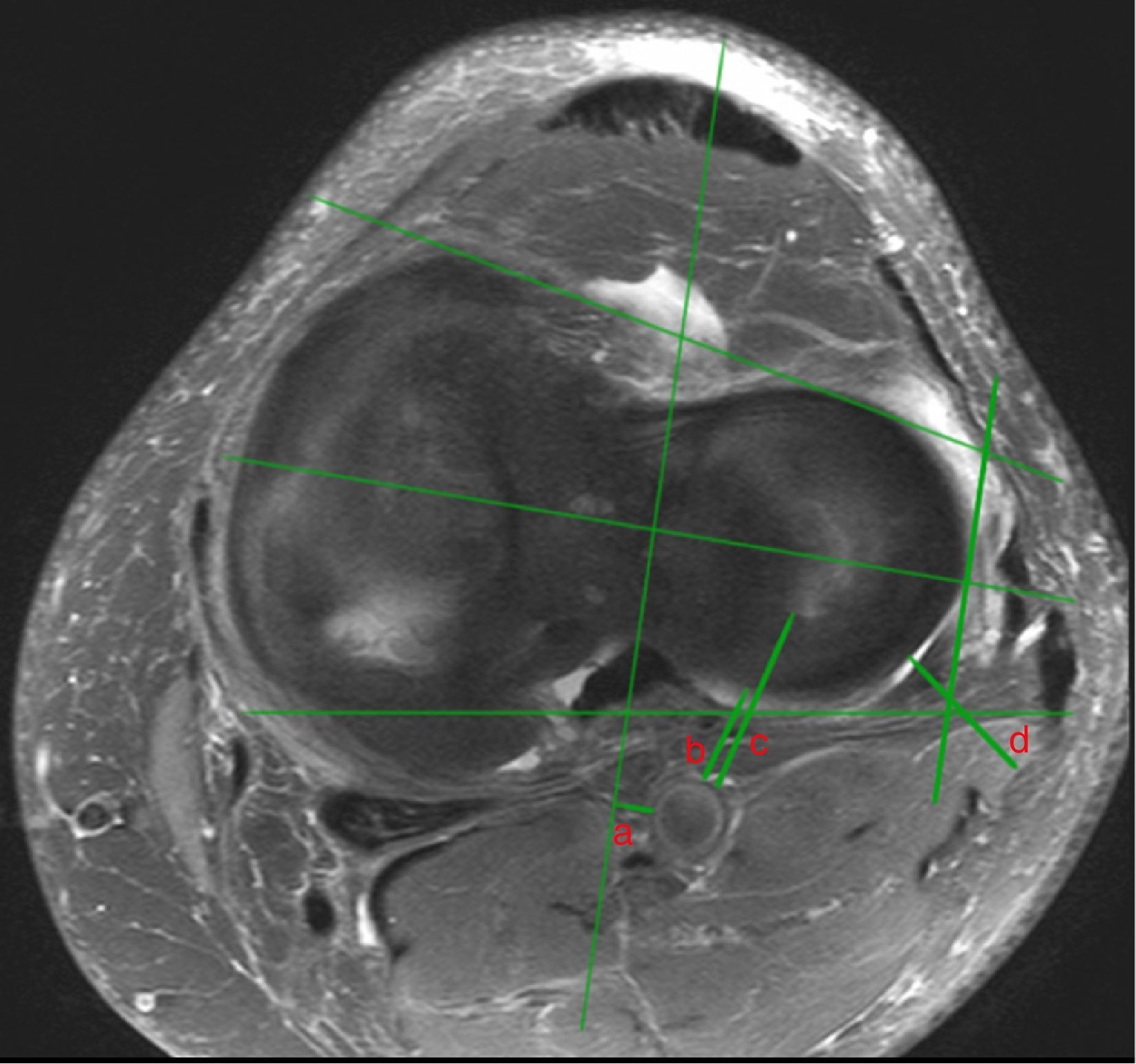
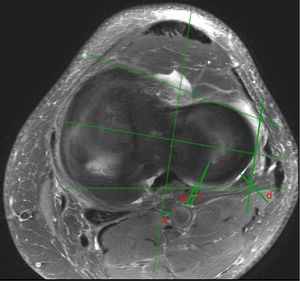
Using the digital measurement program available at our hospital (Syngo Studio), we carried out a series of measurements. The variables analyzed were the following: minimum distance from the meniscal wall to the popliteal artery, minimum distance from the free edge of the meniscus to the popliteal artery, minimum distance from the meniscal wall to the CPN, mean distance between CA and popliteal artery, mean diameter of the tibial plateau and mean diameter of the external meniscus. We traced a line running parallel to CA, which passed by the popliteal hiatus and determined the location of the CPN relative to this line (Fig. 2). We traced the lines, following the theoretical direction from the anteromedial and anterolateral portals, taking into account the limitation entailed by the external tibial spine, to determine whether the popliteal artery was accessible through those portals or not (Fig. 1). Other variables analyzed were the presence or absence of ACL tear or a “bucket handle” tear of the internal meniscus and the existence or absence of a Baker cyst.
Axial section in SPAIR sequence of the left knee. Mean minimum distance from CA to the popliteal artery (a), mean minimum distance from the wall to the popliteal artery (b), mean minimum distance from the free edge to the popliteal artery (c), mean minimum distance from the wall to the CPN (d). Line parallel to CA, medial to the popliteal hiatus and location of the CPN.
We contacted patients by telephone and asked their weight and height. We also calculated their BMI.
The continuous variables were presented with the mean, standard deviation (SD) and range of the sample. The hypothesis of normality of the distributions was evaluated through the Shapiro–Wilk test. The Student t test was used to compare the mean values of distances, BMI, age and weight between groups. The association between continuous variables was studied through the Pearson r correlation coefficient. For all these tests we accepted a level of statistical significance of P ≤.05 in bilateral contrast. The data were analyzed with the statistical software package SPSS v14.0 (SPSS Corp, Chicago, USA).
ResultsWe analyzed 102 magnetic resonances corresponding to 60 right knees and 42 left knees. The mean age of our patients was 45 years (range: 15–74 years), and there were 74 males and 28 females. A total of 18 patients (17.6%) presented a Baker cyst, 12 patients (11.8%) a torn ACL and 13 patients (12.7%) a “bucket handle” tear of the internal meniscus.
The popliteal artery was located laterally to the midline in 94.1% and coincided in 5.9% of cases. The artery was never located in a medial position.
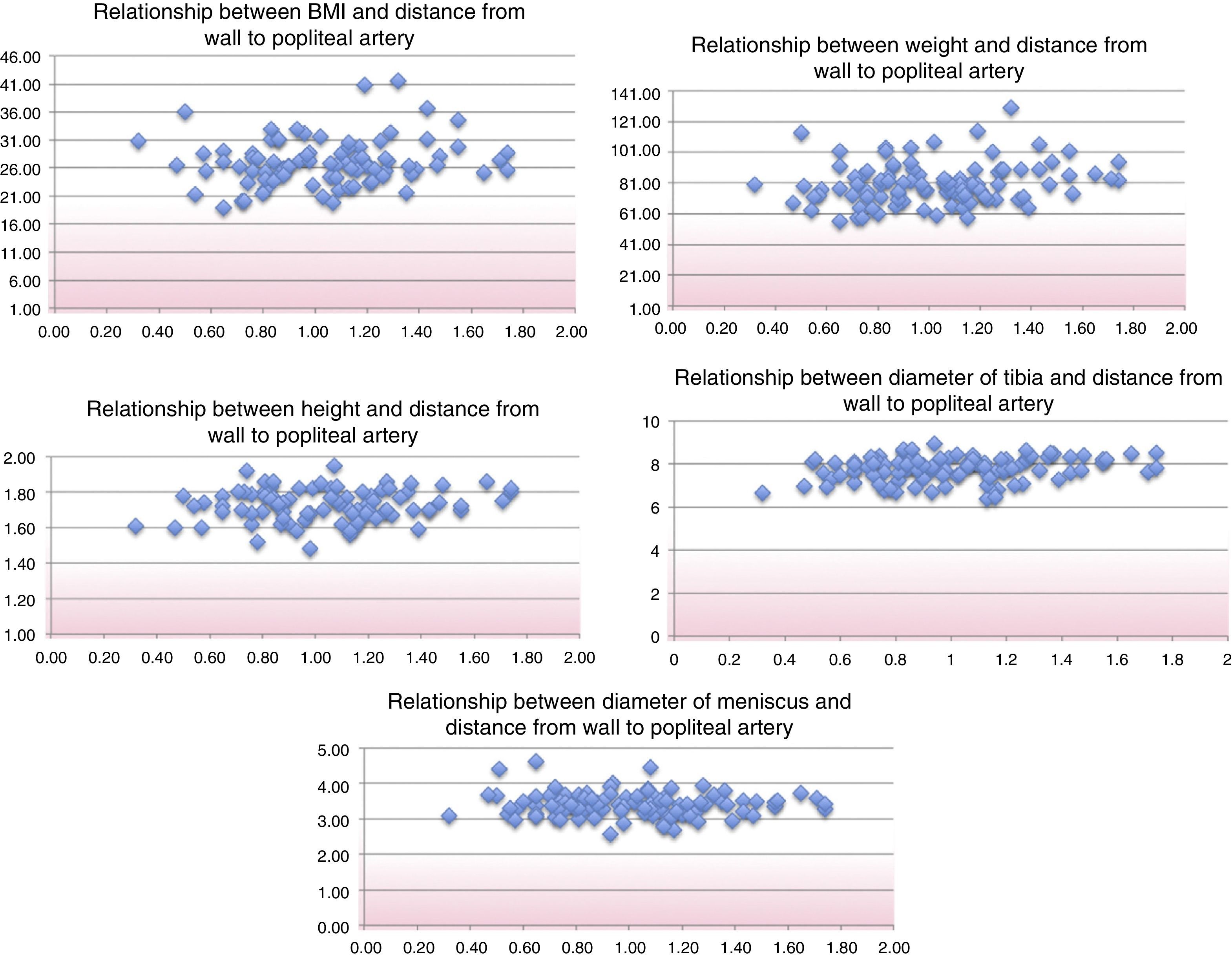
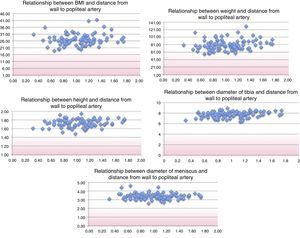
The mean minimum distance from the posterior wall of the external meniscus to the popliteal artery was of 1.01cm (range: 0.32–1.74cm, SD: 0.30). We observed that this distance was greater among males than females (males: 1.06cm, SD: 0.29; females: 0.88cm, SD: 0.28; P=.006) (Table 1). By relating this distance to other variables we observed that there was no correlation between the distance from the posterior wall of the external meniscus to the popliteal artery with: height (r=0.14; P=.17), weight (r=0.19; P=.04), BMI (r=0.15; P=.16), the anteroposterior diameter of the external meniscus (r=0.06; P=.55) and the diameter of the tibial plateau (r=0.23; P=.01) (Fig. 3).
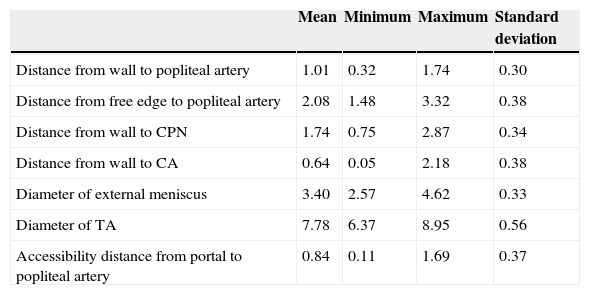
Data from measurements and statistical analysis of the main variables.
| Mean | Minimum | Maximum | Standard deviation | |
|---|---|---|---|---|
| Distance from wall to popliteal artery | 1.01 | 0.32 | 1.74 | 0.30 |
| Distance from free edge to popliteal artery | 2.08 | 1.48 | 3.32 | 0.38 |
| Distance from wall to CPN | 1.74 | 0.75 | 2.87 | 0.34 |
| Distance from wall to CA | 0.64 | 0.05 | 2.18 | 0.38 |
| Diameter of external meniscus | 3.40 | 2.57 | 4.62 | 0.33 |
| Diameter of TA | 7.78 | 6.37 | 8.95 | 0.56 |
| Accessibility distance from portal to popliteal artery | 0.84 | 0.11 | 1.69 | 0.37 |
CPN: common peroneal nerve.
Dispersion cloud. There is no correlation between the distance from the wall to the popliteal artery and BMI (r=0.15; P=.16), weight (r=0.19; P=.04), height (r=0.14; P=.17), anteroposterior diameter of the external meniscus (r=0.06; P=.55) and the mediolateral diameter of the tibia (r=0.23; P=.01).
Analyzing the data, we did not observe any differences between the presence or absence of a Baker cyst with the mean distance from the wall to the popliteal artery (1.12 SD: 0.26 vs 0.99 SD: 0.31; P=.10). Neither was this distance modified in the presence of an ACL tear (1.01 SD: 0.19 and absence 1.01 SD: 0.32; P=.96), or in the presence of a “bucket handle” tear of the internal meniscus (1.06 SD: 0.19 and absence 1.0 SD: 0.32; P=.41).
The mean minimum distance from the free edge of the external meniscus to the popliteal artery was 2.08cm (range: 1.48–3.32, SD: 0.37). We observed that this distance was greater among males than females (males: 2.15cm, SD: 0.38; females: 1.90cm, SD: 0.29; P=.002). By relating this distance to other variables we observed that there was no correlation between the distance from the free edge of the external meniscus to the popliteal artery with: height (r=0.17; P=.11), weight (r=0.18; P=.08), BMI (r=0.11; P=.31), the anteroposterior diameter of the external meniscus (r=0.17; P=.08) and the diameter of the tibial plateau (r=0.27; P=.006).
We assessed the location of the CPN based on the line running parallel to CA, which passed by the popliteal hiatus and determined that the position of the CPN was lateral to the popliteal hiatus in 91.2% of cases, medial in 5.9%, and coinciding in 2.9%. We did not find significant differences between genders in terms of the distance from the wall to the CPN (P=.89).
The mean minimum distance from the posterior wall of the external meniscus to the CPN was 1.74cm (range: 0.75–2.87, SD: 0.34). We observed that there were no significant differences in this distance between males and females (males: 1.74cm, SD: 0.33; females: 1.75cm, SD: 0.39; P=.89). By correlating this distance with other variables, we observed that there was no correlation between the distance from the posterior wall of the external meniscus to the CPN with: height (r=0.15; P=.18), the anteroposterior diameter of the external meniscus (r=0.006; P=.95) and the diameter of the tibial plateau (r=0.073; P=.46).
However, we did find a moderate positive correlation between this distance and weight (r=0.44; P<.001) and also BMI (r=0.41; P<.001). In the case of BMI, this correlation was higher among females (positive high r=0.68; P<.001) than males (positive low r=0.28; P=.03).
The popliteal artery was not accessible from the anteromedial arthroscopic portal in any case, whereas it was accessible from the anterolateral portal in 100% of cases. The mean minimum distance, perpendicular to the axis of the anteromedial portal to the popliteal artery was 0.84cm (range: 0.11–1.69, SD: 0.37).
DiscussionAlthough popliteal artery lesions during knee arthroscopy are infrequent,8 they can have severe consequences, such as pseudoaneurysms,9 arteriovenous fistulas10 and amputation.
In our series, the popliteal artery presented a lateral location to the midline in 94.1% of cases and coincided in 5.9%. The artery was not located in a medial position in any case. Similar results have been reported by Keser,11 with 94.3% of lateral location, and Ninomya,7 with 95%.
Other works have related the location of the artery relative to the edge of the tibial plateau,7,11,12 some of them even evaluating the vascular risk in tibial osteotomies and knee arthroplasties, and finding distances between 6.513 and 7mm.14 In order to assess the risk in meniscal sutures we must reference the location of the artery to the meniscus and calculate this distance relative to the references that we have during surgery, in this case the free edge and the posterior wall of the meniscus.
In our series, the mean minimum distance from the posterior wall of the external meniscus to the popliteal artery was 1.01cm (1.06cm in males and 0.88cm in females). This distance is within the depth range recommended by the different “all-inside” meniscal suture devices. Thus, for example, the FasT-Fix 360° suture system (Smith and Nephew, Andover, MA, USA) is preloaded at 18mm, and recommends 14mm,15 the Meniscal-Cinch (Arthrex, Naples, FL, USA) is preloaded at 10mm and recommends 14mm,16 the Omnispan (Mitek, Raynham, MA, USA) is preloaded at 13mm,17 the Sequent (ConMed, Utica, NY, USA) recommends 16mm18 and the Maxfire (Biomet, Warsaw, IN, USA) recommends between 16 and 18mm19 for sutures in the posterior horns. It could be deduced that using these devices at the recommended depth to perform sutures in the posterior horn of the external meniscus could entail a risk of vascular lesion.
Some authors20,21 recommend limiting the depth to 15mm. With a depth of 17mm, Cohen22 verified that in 43% of cases in his series of cadavers, the tip of the penetrating needle was within a radius of 0.5mm from the artery.
It is true that the needle penetrates the meniscus within its thickness and that this should be taken into account when assessing the depth of penetration of a device. It is also true that in the case of vertical sutures, which have been proven to be biomechanically more resistant, the upper point of entry should be located directly above the joint capsule and, in this case, the distance should be measured from the meniscal wall, as in our study. Moreover, the external meniscus is more mobile and displaces in the posterior direction upon flexion by a mean distance of 11.2mm23 and could displace even further upon introducing the suture device. The technical difficulty to control this depth has been described previously, with cases of excessive penetration, even of the skin.20 On the other hand, reducing the length of penetration of “all-inside” suture devices could lead to implants being deployed before passing the meniscal wall, in an intraarticular position, where they would not fulfill their function and could even lead to chondral lesions.
One limitation of our work is that we have not taken into account the variation in the distance between knee flexion and extension, obtaining MRI images with the knees at 10° flexion, which is not the usual position in which to conduct a suture of the external meniscus. The question of whether the artery is clearly displaced in a posterior direction on flexion remains unanswered.24 Smith questioned this generalized belief and finds cases in which this distance decreases on flexion; describing the behavior of the artery in the flexion–extension range as unpredictable.13 Zaidi also observed anterior displacement of the artery, with an approximation to the plateau in knee flexion in 12 out of 20 cases.25 Eriksson described an approximation of 1mm when going from extension to flexion.14 Matava observed that the distance increased when going from a flexion of 90° to one of 110°, but not before that.26 Thus, it does not seem prudent to take for granted the fact that the artery will be displaced in a posterior direction and that we can, therefore, use greater depths with “all-inside” suture devices to perform suture in the “figure four” position, forcing flexion varus.
Another limitation is that we did not take into account the presence of arthroscopic fluid, which distended the joint capsule and, theoretically, could displace the artery and increase the distance.
In our series we did not find an association between the distance from the meniscal wall and the popliteal artery with weight, height and BMI. The absence of this association implies that the risk of vascular damage does not decrease in stout patients. It also means that a safe suture depth cannot be predicted and this cannot be taken into account when selecting one technique over another. Other authors have reported a relationship with the distance between the popliteal artery and the tibial plateau based on anthropometric parameters, like the circumference of the knee.21
We did not find any differences in the distance between the wall and the popliteal artery based on the presence or absence of a torn ACL. Certain studies have proven an increase of the distance between the popliteal artery and the posterior edge of the tibial plateau in patients with torn ACL compared to patients with intact ligaments.27 Neither did we find differences in the distance between the wall and the popliteal artery according to the presence or absence of a Baker cyst, which could displace the artery laterally provided its size were sufficiently large.11
In our series, the mean minimum distance from the posterior wall of the external meniscus to the CPN was of 17.4mm, which seems sufficiently safe to perform an “all-inside” suture in the proximity of the popliteal hiatus, taking into account this depth when placing our suture device directly over the joint capsule. The fact that this distance was not related to the height or diameter of the tibial plateau, but only to weight and BMI, and that this correlation was greater among females than males could be explained by the accumulation and distribution of the surrounding fatty tissue.
We verified that the artery would not be accessible with an “all-inside” suture device from the anteromedial portal, taking into account the limitation imposed by the external tibial spine, and neither would it be possible to gain adequate access to the medial area of the popliteal hiatus, closer to the root, in order to conduct the suture. On the other hand, the anterolateral portal afforded direct access to the popliteal artery in 100% of cases.
The use of “all-inside” devices directly from the anterolateral portal toward the posterior horn of the external meniscus entails a very high risk of damaging the popliteal artery.21 Other repair techniques for the posterior horn of the external meniscus have been described, using accessory portals to avoid this problem.28,29 It is also worth taking into consideration that certain authors recommend using only scraping for meniscal lesions medial to the popliteal hiatus, in order to avoid the risk of vascular lesions, in cases where these are not associated to reconstructions of the ACL, and have reported good results in this regard.30–32 However, if the lesion is complete, we consider it more advisable to perform meniscal suture.
When performing a suture of the posterior horn of the external meniscus, we can opt for performing an “inside–outside” suture through a counter-incision and using a specific separator33 to limit the sutures to the region adjacent to the popliteal hiatus and scraping in the more medial area, just anterior to the location of the artery,31,32 or else we can use specific “all-inside” suture systems, to pass sutures without an implant and limiting the progression of the recovery needle.34 We do not recommend performing “all-inside” sutures with devices that penetrate into the joint capsule in the area medial to the popliteal hiatus from the anterolateral portal.
The proximity of the artery to the posterior wall of the external meniscus must be taken into account when suturing the posterior horn. This distance is not related to height, weight, BMI, plateau diameter or the size of the external meniscus. This distance is within the recommended length range of “all-inside” suture devices.
Level of evidenceLevel of evidence III.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation adhered to the ethical guidelines of the Committee on Responsible Human Experimentation, as well as the World Medical Association and the Declaration of Helsinki.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestThe authors have no conflict of interests to declare.
The authors wish to thank Isabel Millán Santos, from the Biostatistics Unit at Hospital Universitario Puerta de Hierro, for her contribution.
Please cite this article as: Sanz-Pérez M, García-Germán D, Ruiz-Díaz J, Navas-Pernía I, Campo-Loarte J. Localización de la arteria poplítea y su relación con el riesgo vascular en la sutura del cuerno posterior del menisco externo. Rev Esp Cir Ortop Traumatol. 2015;59:165-171.