To assess fusion rates and functional outcomes in patients undergoing anterior cervical discectomy and fusion by using a vertebral body autograft for interbody filling and anterior cervical plate fixation.
Material and methodsThe study included a total of 102 patients, 54 men and 48 women, who underwent surgery between 2006 and 2010 on patients with degenerative disease, cervical disk herniation and radiculopathy, and who had failed standard conservative treatment (3 months). The study was limited to patients with fusion levels 1–3. The mean patient follow-up was 44 (24–96) months. Their mean age was 48.8 years.
ResultsThe clinical variables analyzed were duration of symptoms (>12 months), smoking (31% smokers), employment status (76% active), average days of hospitalization (2.2 days), operation time (62min), etiology (100%, degenerative disease), notable comorbidities (28%), fusion levels (42% 1, 49% 2, 9% 3), and symptoms of radiculalgia or axial pain. The functional variables analyzed scores (preoperative and postoperative scores) were VAS (8.6–1.32), Neck Disability Index (37.7–5.8), and Odom criteria (76% reflected excellent results after surgery). Finally, radiological variables were also analyzed: anterior reactive osteophytosis (16%), significant collapse (0%), and fusion rate (98%). There were 4 cases of acute postoperative complications, and 4 chronic, none of them were related to the surgical technique.
DiscussionThe use of autograft bone of the vertebral body itself reduces comorbidities associated with the use of the iliac crest of the patient. Our results using the technique described are comparable to those in the literature, with a fusion rate of 98% and a mean of 62min duration of the procedure.
Evaluar tasas de fusión y resultados funcionales en pacientes intervenidos de discectomía y fusión cervical anterior empleando autoinjerto de cuerpo vertebral para el relleno del dispositivo intersomático, y fijación anterior con placa cervical.
Material y métodosCiento dos enfermos, 54 varones y 48 mujeres, intervenidos entre 2006 y 2010. Se incluyeron pacientes con patología degenerativa, hernia discal cervical y radiculopatía, en los que había fracasado el tratamiento conservador habitual (3 meses). Se incluyeron pacientes con fusión de 1–3 niveles. El seguimiento medio fue de 44 (24–96) meses. Su edad media era de 48,8 años.
ResultadosLas variables clínicas analizadas fueron: tiempo de evolución de los síntomas (>12 meses), tabaquismo (31% fumadores), situación laboral (76% activos), estancia hospitalaria (2,2 días), tiempo quirúrgico (62 minutos), causa de la cirugía (100%, patología degenerativa), comorbilidades destacables (en el 28%), niveles fusionados (42% 1, 49% 2, 9% 3), clínica asociada (radiculalgia o dolor axial). Variables funcionales analizadas (puntuación pre y postoperatoria): EVA (8,6–1,32), Neck Disability Index (37,7–5,8), criterios de Odom (76% reflejaron resultados excelentes tras la cirugía). Variables radiológicas analizadas: osteofitosis reactiva (16%), colapso (0%), tasa de fusión (98%). Se produjeron 4 complicaciones agudas postoperatorias y 4 crónicas, ninguna relacionada con la técnica quirúrgica.
DiscusiónEl empleo de autoinjerto óseo del propio cuerpo vertebral reduce las comorbilidades asociadas al uso de cresta ilíaca del propio enfermo. Nuestros resultados son comparables a la literatura, con una tasa de fusión del 98% y un promedio de 62 minutos de tiempo quirúrgico.
The surgical procedure of discectomy and anterior cervical arthrodesis was first described in 1950 by Smith, Robinson and Cloward. It is the standard technique for the surgical treatment of degenerative and traumatic cervical pathologies.1
The original description of the technique is characterized by the use of tricortical autografts from the iliac crest, which represents the gold standard and ideal type of graft due to its properties. The cortical component confers mechanical stability, whilst the cancellous provides excellent osteoconductive and osteoinductive properties.
However, obtaining iliac crest grafts is associated to morbidity in the donor area, along with an increase in the duration of surgeries.
In these circumstances, various alternatives, such as the new tantalum cages, allografts, demineralized bone matrix and bone substitutes, have been discussed as filling materials for new interbody devices. Use of these materials eliminates morbidity at the donor site and provides good osteoconductive properties, although poor osteoinductive ones.2,3
The objective of our study was to evaluate the rates of fusion and functional results in a series of patients who underwent discectomy and anterior cervical fusion through the use of a vertebral body autograft to fill the interbody device with anterior fixation using a cervical plate.
Material and methodsWe conducted a descriptive, retrospective study, with prospective data collection. Our population was comprised of 110 patients, 54 males and 56 females, who were intervened at our center (Fundación Alcorcón University Hospital, Madrid) between 2006 and 2010. The inclusion criteria were: patients with degenerative pathology, cervical disk herniation and radiculopathy, in whom the usual conservative treatment, which except in the case of progressive neurological involvement being carried out for at least 3 months, had failed. We excluded patients with a history of trauma, infection, neoplasms and hematological diseases, as well as those in whom we could not study all the variables for any reason. After applying these criteria, the population was limited to 102 patients (4 were excluded due symptoms caused by trauma and another 4 due to a lack of full radiographic monitoring). We included patients with interventions to fuse 1–3 levels. The mean follow-up time of the patients was 44 months (range: 24–96 months) and the mean age of the sample was 48.8 years.
The data were collected based on the electronic clinical history and the questionnaires completed by patients before and after the intervention.
In all cases the interbody cages employed were PEEK type (poly ether ether ketone) with anterior cervical plates from different commercial manufacturers, but with the same technical characteristics (SC-Acufix Slimline®, Vectra®, Sonoma®).
The clinical variables analyzed were the following:
- 1
Time of evolution of the symptoms: the time of evolution of the symptoms was over 1 year in all cases.
- 2
Smoking: 31.3% of the patients (32 cases) were active smokers.
- 3
Employment status: 76% of the patients (78 cases) were actively employed.
- 4
Average days of admission: 2.2 days.
- 5
Duration of surgery: 62.3min (mean duration).
- 6
Etiology of the intervention: 102 patients (100%) suffered a degenerative pathology.
- 7
Comorbidities: 28% of the patients (29) associated significant comorbidities. Pathologies considered included ischemic cardiopathy, neoplasms and inflammatory diseases (diabetes mellitus, rheumatoid arthritis and autoimmune diseases).
- 8
Number of levels intervened: 1 level: 42% (43 patients); 2 levels: 49% (50 patients); 3 levels: 9% (9 patients).
- 9
Associated symptoms: all patients presented the symptoms of radiculalgia and/or cervical axial pain.
- 10
Visual analog scale (VAS).
Functional scales analyzed: Neck Disability Index (NDI) and Odom criteria.
Radiographic variables studied were analyzed based on the first and last postoperative radiographs of the patient (anteroposterior and lateral projections) and examined by 2 observers.
- •
Fusion: defined as the existence of clearly observable bone bridges through radiography, absence of mobilization of the implant and, above all, absence of observable radiolucent lines. Dynamic radiographs were analyzed in cases where there were reasonable doubts between the 2 observers.4
- •
Anterior reactive osteophytosis: we aimed to assess the appearance of anterior osteophytes in the intervened level (secondary to obtaining autografts from the uncinate processes) or in adjacent levels.
- •
Significant collapse: more than 2mm collapse in the arthrodesis segment when comparing both radiographs.
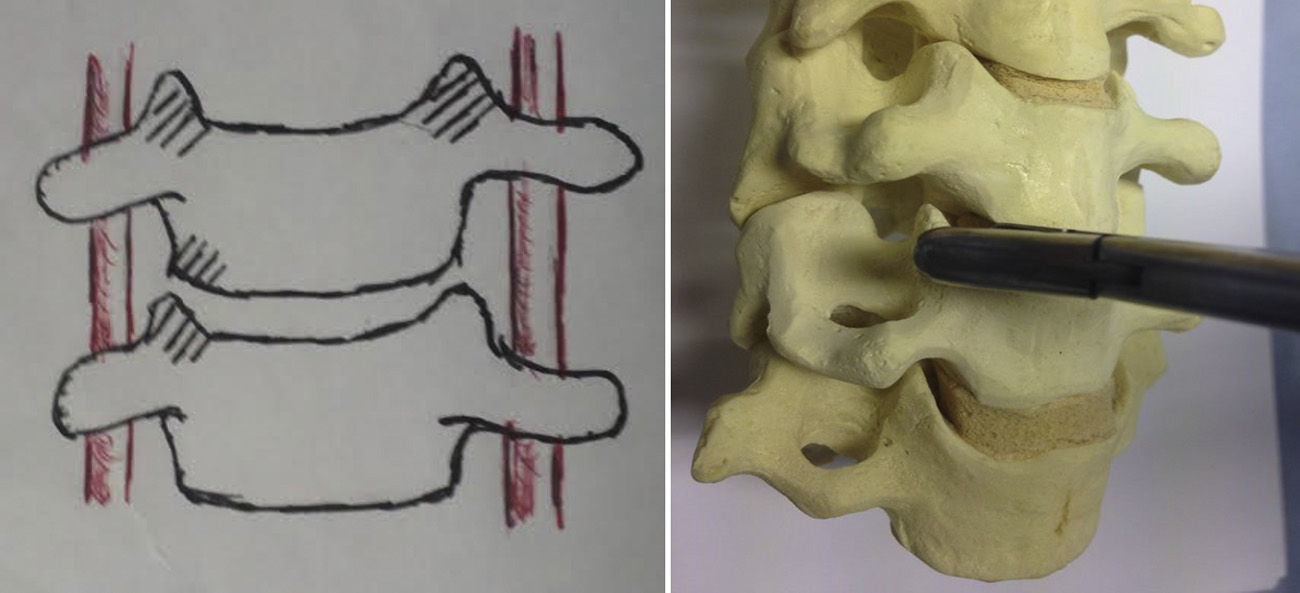
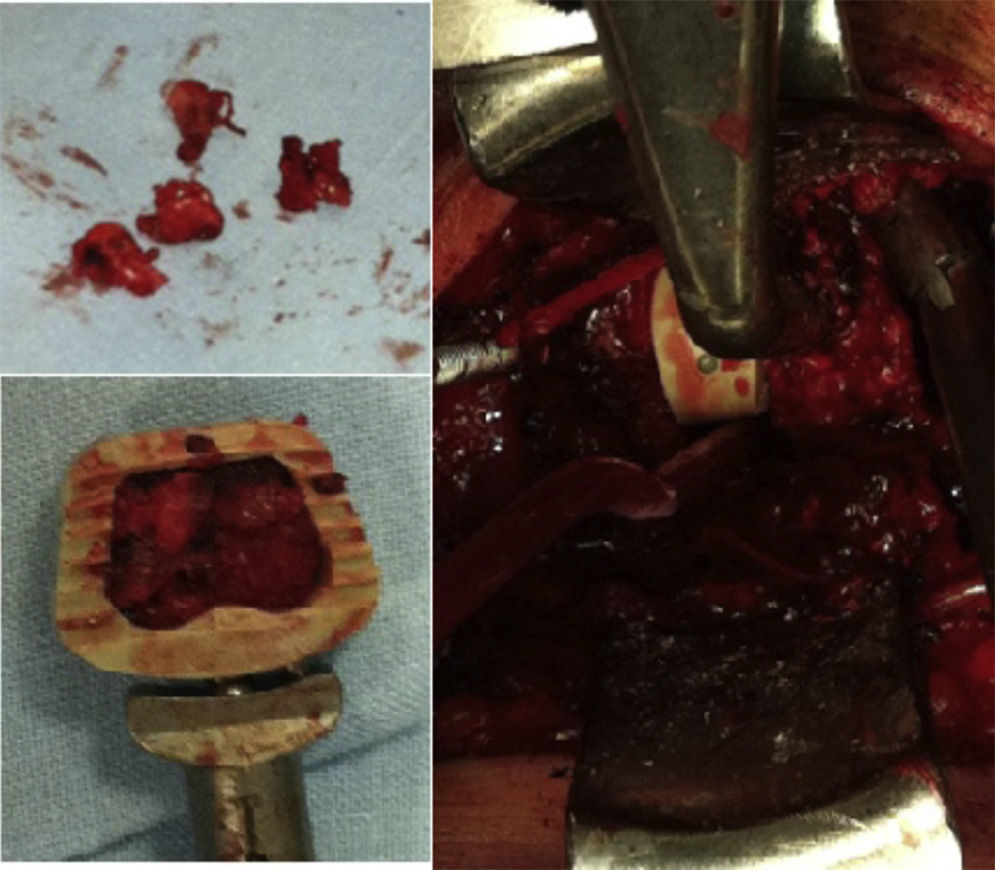
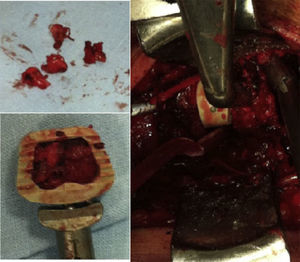
The surgical technique employed consisted in the usual anterolateral approach, generally from the left side, and after locating the levels to be intervened through radioscopy, a Caspar distractor was used to conduct discectomy, resection of the posterior common vertebral ligament and posterior osteophytectomy, followed by drilling of the vertebral plates, up to bleeding points, without reaching the cancellous region of the bone. The autografts taken from the vertebral body to fill the interbody device were obtained from the local decompression conducted and, especially, from the common area of the uncinate processes (Fig. 1). A careful dissection was carried out using bipolar forceps, separating the musculature of the longus colli and exposing the superior and inferior uncinate processes on both sides, without reaching the vertebral artery and nerve root. Subsequently, the bone was extracted with small gouge forceps directly from the specified area at the necessary levels, so as to obtain the required amount to fill the device without the need to take a graft from the iliac crest of the patient and without requiring the use of allografts from the tissue bank or bone substitutes. We filled the interbody cages as shown in Fig. 2, placed them in the discal space, released the distraction with the Caspar distractor and then placed an anterior self-blocking plate. Subsequently, the platysma and skin were closed under aspirative drainage.
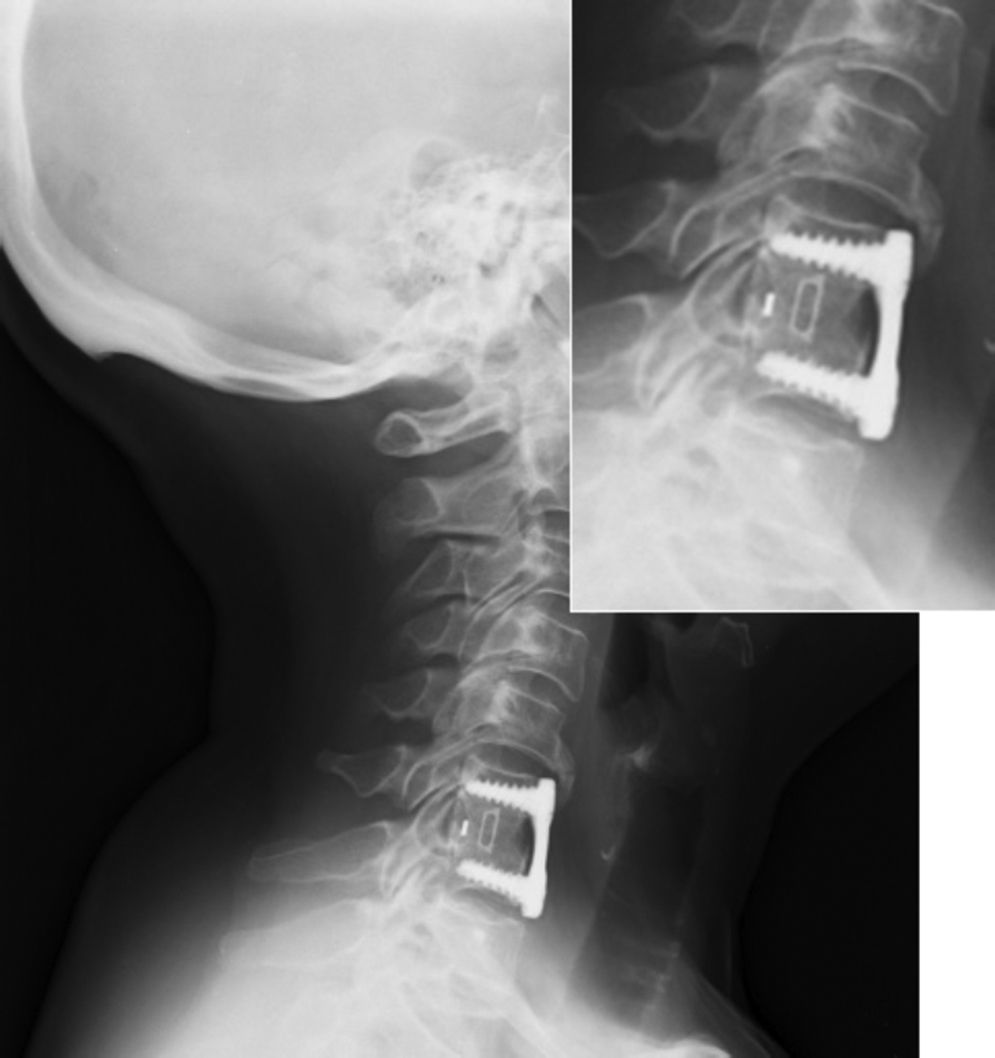
The patients were mobilized on the following day without the need for orthesis and were usually discharged after 48h, following a radiographic control (Fig. 3).
Patients were told to resume their daily life activities immediately, without making considerable efforts, and follow-up visits took place after 1, 3, 6 and 12 months. Return to work varied according to the type of activity of each patient.
ResultsOur results, from the standpoint of analysis of clinical variables, were the following:
Postoperative improvement of symptoms (radicular or axial pain):
A total of 85 patients experienced a complete improvement of symptoms, compared to 13 with partial improvement, 3 with no postoperative improvement and 1 with recurrence of radicular symptoms after an initial postoperative improvement.
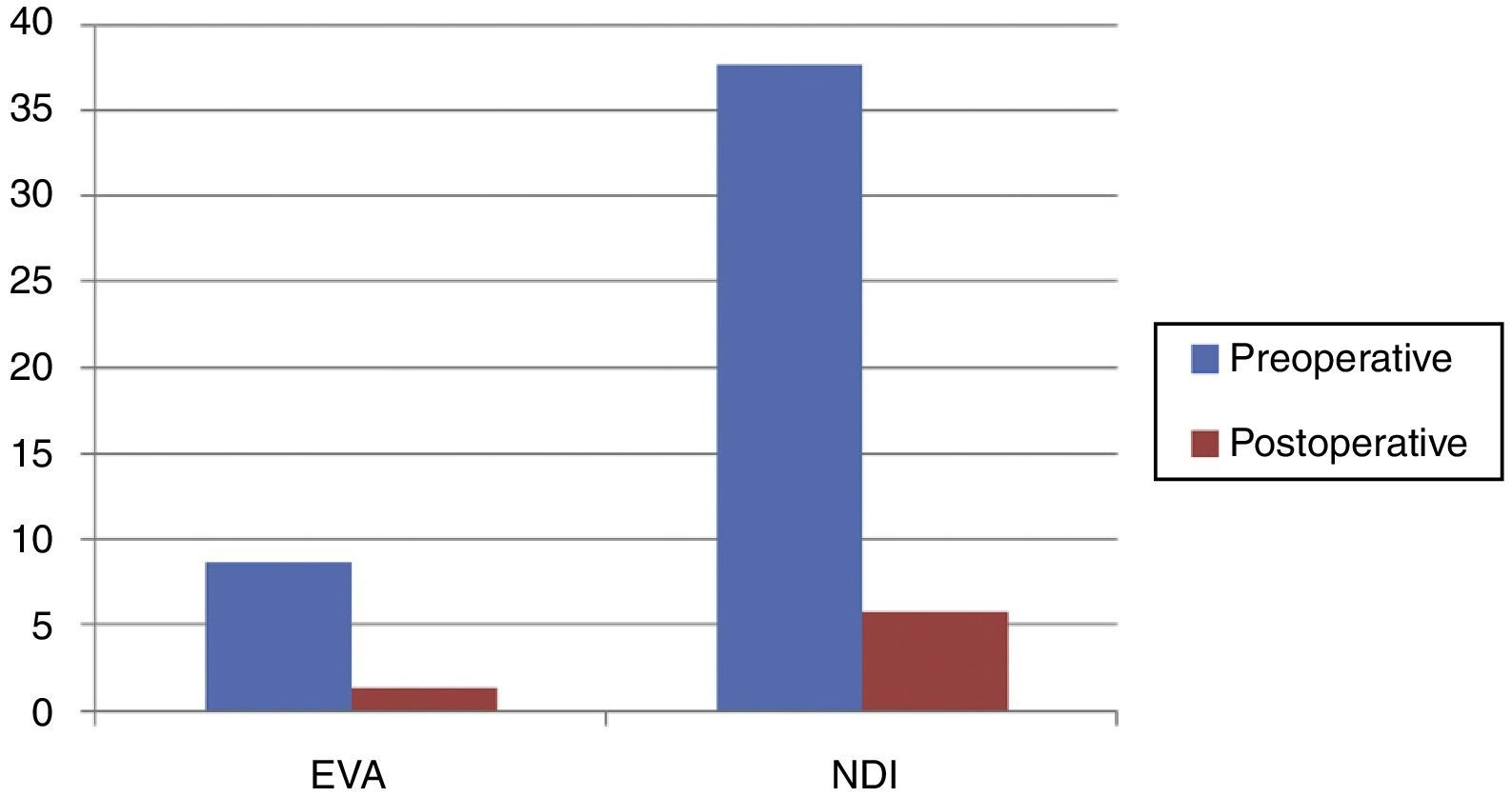
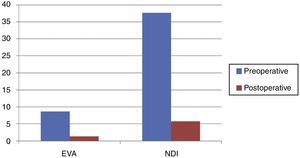
The assessment of patients on the VAS scale before and after the surgery was the following: mean value of 8.6 points in the preoperative vs 1.32 points in the postoperative assessment.
Functional resultsPreoperative assessment of the patients was based on the Neck Disability Index: 37.7 points vs 5.8 points in the postoperative functional assessment.
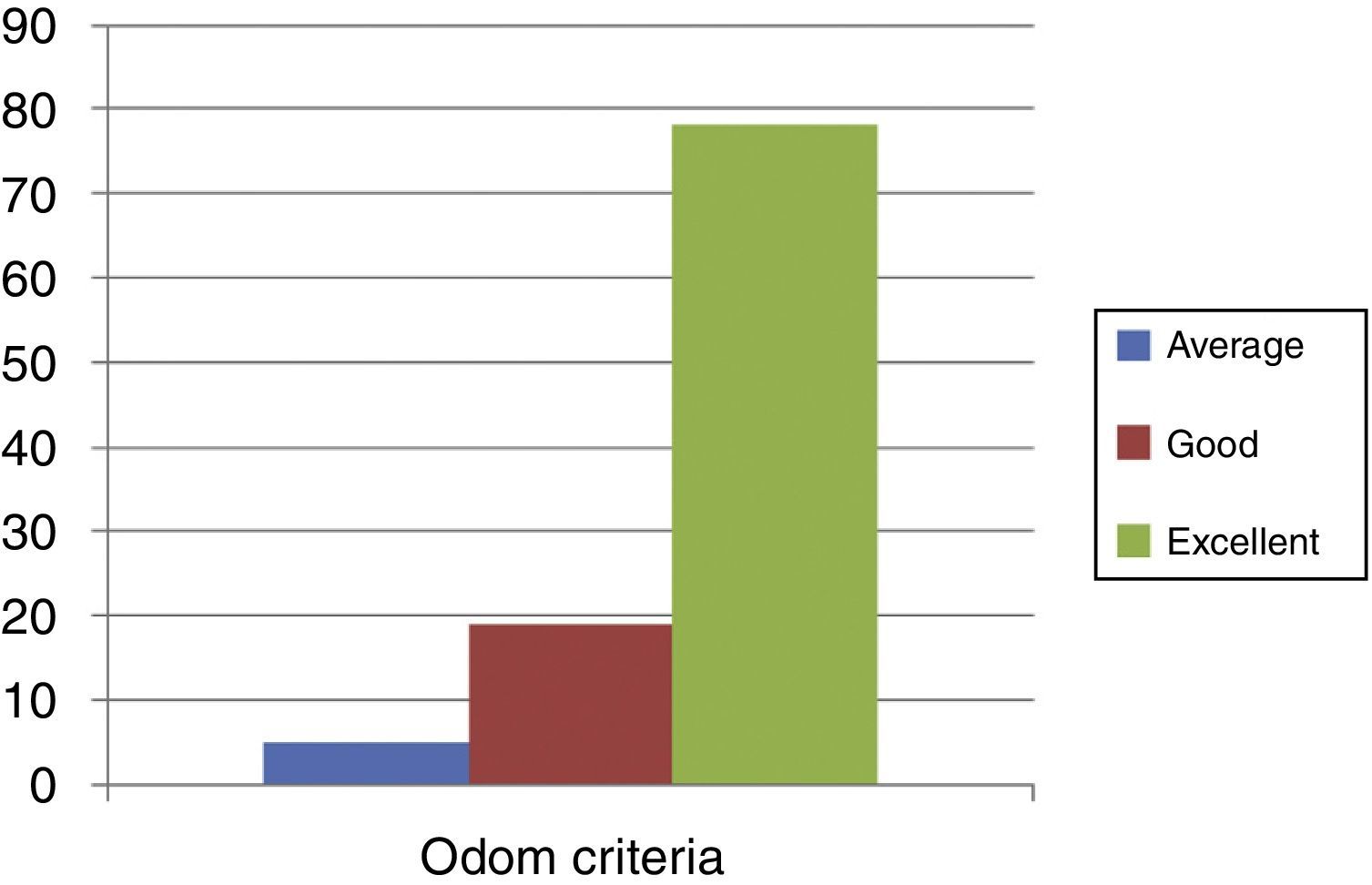
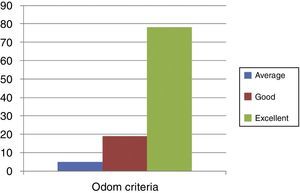
Assessment of postoperative functional results in terms of Odom criteria: 76.4% (78 patients) described their results as excellent, 18.6% (19 patients) as good, 4.9% (5 patients) as average and none of the patients described their results as poor in terms of the Odom criteria (Figs. 4 and 5).
Radiographic results obtained:
- •
Anterior reactive osteophytosis (Fig. 6): 16.6% (17 patients), with the majority being anterior osteophytes which appeared in the superior or inferior adjacent vertebral body, as a reactive process to the anterior cervical plate which was, in some cases, excessively long. Therefore, this was not clearly related to the graft donor areas.
- •
Significant collapse: there were no cases.
- •
Radiographic solid fusion: 98%; there were 2 cases of images with doubtful lithic lines (Fig. 7) in the anteroposterior and lateral projections during the last postoperative radiographic control, which in no case presented clinical correlation or required a surgical reintervention.
Regarding the complications which took place in our series, the results were the following:
- •
Acute (4 cases): 2 subcutaneous hematomas requiring surgical review (no cases of active arterial bleeding), 1 case of significant transient dysphagia, and 1 case of tetraparesis probably secondary to ischemia which improved progressively although with residual sequelae.
- •
Chronic (4 cases): 2 cases of mobilization or discomfort related to the arthrodesis material which required its extraction and 2 cases of new disk herniation in an adjacent level (both reintervened).
None of the complications observed were related to the surgical technique employed.
DiscussionThere is scarce literature regarding the use of autografts taken from the vertebral bodies to fill the interbody devices in cervical arthrodesis.
In our study, the entire population (102 patients) underwent the procedure of discectomy and anterior cervical fusion, with interposition of interbody cages filled with autograft obtained from the vertebral body and anterior fixation with a plate. The rates of fusion were 98%, with 0% collapse. The mean duration of surgery in our series was 62.3min.
The study developed in China by Zhaoyu Ba et al.5 was based on a series of 207 patients who underwent discectomy and anterior cervical arthrodesis with a cervical plate, using PEEK-type cages filled with bone obtained from the local decompression and removal of the anterior hypertrophic osteophytosis. The rates of fusion reported reached 100% at the end of the follow-up period, with postoperative clinical results described as excellent or good in 97% of cases.
Hyun-Woong et al.6 (South Korea) also employed chips of vertebral autograft obtained from the local decompression, in this case also associating demineralized bone matrix (BMPs) in a series of 31 patients. They filled the PEEK cages with the mentioned material and did not use an anterior cervical fixation plate. Their rates of fusion 1 year after surgery were 97%. Regarding the clinical results, there was a significant improvement of the cervicalgia and brachialgia symptoms (preoperative cervical VAS 7.1 vs postoperative 1.6; preoperative brachial VAS 7.7 vs postoperative 2.1).
Some results described in the literature for other current cervical arthrodesis techniques include:
Cho et al. conducted a comparative study among 40 patients who underwent cervical arthrodesis with PEEK cages filled with iliac crest autograft (cases), compared to a control group undergoing discectomy and anterior cervical fusion with tricortical crest autograft (controls). The rates of fusion in the group of cases were 100% vs controls with a rate of fusion of 93%.
Hacker et al. compared the use of 2 types of cages (covered with hydroxyapatite or not) filled with autograft or allograft, versus the standard technique described by Smith, Robinson and Cloward (tricortical iliac crest autograft), and found rates of fusion of 98% in the first case versus 90% in the second. They also found differences in terms of duration of surgery, with a mean duration of 92min in the first group vs 123min in the second group.
Sugawara et al.7 attempted to compare the use of 2 types of bone substitutes to fill the titanium cages and employed beta-tricalcium phosphate and hydroxyapatite. The first group included 57 patients and the second 48. The rates of fusion were similar in both cases (94% in the first group and 90% in the second), and the mean duration of surgery was 109min.
Fernández-Fairen et al.8 compared the use of tantalum cages (28 patients) vs use of tricortical crest autografts associated to an anterior cervical plate (33 patients). The results of this study were 10.7% pseudoarthrosis in the group with tantalum cages vs 15.2% in the group with tricortical crest graft. In addition to the higher rate of pseudoarthrosis, the group which used tricortical crest autograft also showed a rate of pain of 21.2% at the graft donor site.
Regarding the use of iliac crest autograft, its possible associated comorbidities are well-known (Arrington et al., Silber et al.9):
- •
Acute or chronic pain at the graft donor site.
- •
Surgical wound complications (infection, hematoma, seroma, dehiscence, etc.).
- •
Functional repercussions (basic activities of daily life, work activity, sexual life, sport, etc.).10
As we can judge from the literature regarding this matter, our results in terms of fusion rates (98%) were similar to those observed in other series, with a significant reduction of the duration of surgery (which in our case had a mean value of 62min), in addition to a suppression of comorbidities in relation to the graft donor region (in cases where iliac crest autografts were used). Logically, savings were obtained by not using bone substitutes or grafts from the tissue bank.
To our knowledge, our study is the only one to consider the possibility of taking the graft from the region of the uncinates with no repercussions for implant stability, no significant collapse and no evident reactive osteophytes in the graft donor region. Taking grafts from a region distant to the support area for the interbody device contributed to this initial stability, as was also the case significantly with the anterior plate. All this enabled early patient mobilization, as well as the clinical and radiographic results that have been mentioned.
We believe that this technique is feasible, reproducible and useful in the majority of cases in which, due to a degenerative pathology, patients require a surgical intervention.
The main limitations of this work were the retrospective nature of the study (despite the prospective collection of data from patients) and the need to exclude 8 patients (4 due to not fulfilling the inclusion criteria and another 4 due to the absence of data for the studied variables).
ConclusionsThe functional results of our series in discectomy and anterior cervical fusion, with the use of vertebral body autograft to fill the interbody devices and anterior fixation with a cervical plate, were satisfactory in 95% of cases, with fusion rates of 98%, comparable to those reported in the literature, and complications which were not related to the surgical technique in any case.
The advantages of the technique employed include:
- •
Use of autograft.
- •
Suppression of the morbidity associated to the use of iliac crest autograft.
- •
No requirement for allograft and bone substitutes, leading to a significant reduction of the costs and risks that their use entails.11
- •
Reduction of the duration of surgery (compared to the use of iliac crest autograft).
Level of evidence IV.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestThe authors have no conflict of interests to declare.
Please cite this article as: Ferrete-Barroso AM, González-Díaz R, Losada-Viñas JI. Artrodesis cervical anterior con empleo de autoinjerto de cuerpo vertebral. Rev Esp Cir Ortop Traumatol. 2015;59:172–178.