The final collapse of a “stable” thoracolumbar burst fracture is difficult to predict.
This collapse was prospectively studied radiologically in patients with T12 or L1 burst fractures who, after evaluating the admission X-rays and the CT scan with the patients themselves, opted for a rigid thoracolumbar brace with support in the sternal manubrium (TLSO). On the other hand, patients with rigid braces sometimes have low back pain on follow-up (due to overload of the L5-S1 joints).
Hypothesis: the standing lateral X-ray with only a TLSO for support (intrinsic mechanical stability) provides information on the final collapse and could also provide information on the low back pain.
The study included 50 patients (20 males and 30 females, age: 63+14 years) admitted during 2011 and 2012, with 2 losses to follow-up. Variables: Farcy index and local kyphosis (Cobb at 3 vertebrae). X-rays: admission, with TLSO (immediate: Rx0), and at 3 and 6 months. They were compared with the final clinical and radiological results.
It was decided to surgically intervene in 4 patients after Rx0.
There were no painful sequelae at the fracture level, and 16/44 (31%) had low back pain.
Using linear regression mathematical models, the increase in the Farcy index (Rx0-Rx admission) was associated with the appearance of low back pain and with local kyphosis (Rx0-Rx admission), and with the final kyphosis.
It is advisable to perform a lateral standing X-ray after TLSO for information on the final collapse of the fracture and the appearance of accompanying low back pain.
No se sabe a priori el colapso final de una fractura estallido toracolumbar «estable».
Se estudia prospectivamente dicho colapso radiológico en pacientes con fracturas estallido T12 o L1 que, tras valorar las radiografías y TAC al ingreso junto con el paciente en sí, se optó por una ortesis rígida toracolumbosacra con apoyo en manubrio esternal (TLSO). Por otra parte, los pacientes portadores de corsés rígidos presentan a veces dolor lumbar bajo en el seguimiento (por sobrecarga de las articulares L5S1).
Hipótesis: la radiografía en bipedestación con TLSO nada más ponerla (estabilidad mecánica intrínseca) da información sobre el colapso final y pudiera darla sobre el dolor lumbar bajo.
Cincuenta pacientes (20 hombres y 30 mujeres, edad:63+14 años) ingresados durante 2011 y 2012, con 2 pérdidas de seguimiento. Variables: índice de Farcy y la cifosis local (Cobb a 3 vértebras). Radiografías: ingreso, con TLSO (inmediato: Rx0), a los 3 y 6 meses. Se compararon con el resultado final clínico y radiológico.
Tras la Rx0 se decidió intervenir quirúrgicamente a 4 pacientes.
No hubo secuelas dolorosas a nivel de la fractura; 16/44 (31%) presentaron dolor lumbar bajo.
El incremento del índice de Farcy (Rx0-Rx ingreso) se correlacionó con la aparición de dolor lumbar bajo y el de la cifosis local (Rx0-Rx ingreso) con la cifosis final, con modelos matemáticos de regresión lineal.
Se aconseja la realización de una radiografía lateral en bipedestación tras TLSO por la información acerca del colapso final de la fractura y de la aparición de dolor lumbar bajo que aporta.
Thoracolumbar fractures are the most common spinal column fractures and the most increasing in number. Of these, the most frequent are fractures at the thoracolumbar junction (T12 and L1), due to the stress-concentration effect produced by progression from kyphosis to lordosis and the loss of thoracic rib cage protection. In the long term, the most limiting sequela is the appearance of a post-traumatic kyphosis, which is difficult to correct and has a natural history of pain with possible spinal injury. In this case the spine fails to maintain its two physiological functions: a painless upright posture and protection of the spinal column.
White and Panjabi defined instability as the loss of the spinal column's ability to carry out the said physiological functions and described instability as neurological (where there is radiculomedullary injury), mechanical instability (cannot remain standing up without pain) and mixed instability (both conditions simultaneously).
Thoracolumbar fractures have been classified in many ways. Over the years, it has been observed that the major classifications have been offering new viewpoints over the pre-existing ones, based on an attempt to view natural history as a guide to treatment. Thus, in addressing their “stability” Nicoll, 1949,1 refers to stable and unstable fractures. Later studies talk about the anatomical injured areas of the spine, and of the two columns (Holdsworth, 1963: anterior – bodies, spinal disks and their ligaments – and posterior – facets, laminae, lumbar vertebrae and its ligaments)2 or three columns (Denis, 1984: concept of mid spine, posterior vertebral wall and combination of common vertebral posterior ligament and posterior fibrous ring).3 Subsequently, the underlying idea of classification was not just where the injury was but also what the state of the spine was after the injury: its morphological characteristics; the AO classification (Magerl, 1984),4 based on 3 categories: vertebral body compression, anterior and posterior element injuries with distraction and anterior and posterior element injuries with rotation resulting from axial torque. Another guideline is the distribution of load transmission (McCormack, 1994),5 which is based on the communition of the body in the CT scan, the apposition of bone fragments and the amount of post-operative correction performed (surgical or otherwise). Lately, TLICS classifications (Lee and Vaccaro, 2005)6 which are conceptually similar to that of Magerl have been made, with specific references to the posterior ligament complex and to neurological status, and very recently the AOSpine group (Reinhold, 2013; Vaccaro and AOSpine group of spine trauma and injury, 2013), classification was published where a morphological classification was added: (a) a finer neurological staging than that of the TLICS was made (including transient and radicular injury) and (b) modifiers due to the patient's state of health (e.g., ankylosing spondylitis or cutaneous burn) influencing decision-making regarding whether to perform surgery or to modify plans for surgery. Morphological classification staging of injury ranges from the most to the least severe (contrary to the previous ones). Firstly it must therefore be determined whether there is dislocation of the medullary canal or not, either due to angulation, translation, rotation, torsion or a combination of these mechanisms: if there is, then this is a type C, if not, we then verify if there is an anterior or posterior ligamentous distraction injury, in which case this would be a type B, and if there is not, the main injury would be assessed according to the degree of injury due to compression of the vertebral body (types A): if there is a burst fracture and this affects the two endplates then this is a type A4 (comminution of the body with fracture of the posterior wall and possible vertical fracture of the lamina, due to instantaneous separation of the pedicles from the energy produced by the body bursting), if the endplates are not affected it will be a type A3; if there is no burst fracture (posterior wall intact and no communition of the body) but there is coronal line linking both endplates (pincer fracture) this will be a type A2. If there is only collapse through endplate impaction this will be a type A1 and finally, if there is no injury of the vertebral body this will be a type A0 (e.g., an isolated transverse apophysis). In addition to this, thoracolumbar injuries may be described at several levels of the thoracolumbar spine, graded from greatest to least severity in the written description of patient injuries.
On the basis that there are no fully agreed surgical indications in trauma, except for progressive neurological injury, criteria have been defined to indicate which patients would benefit from surgical treatment, such a local kyphosis, the level of comminution of the vertebra, the involvement of the complex posterior ligaments, etc. but there is extensive debate in this regard, which extends far beyond the contents of this paper. We would only state that the concept of stability (mentioned above) is one idea; another is the radiological criteria which appear to detect a mechanical instability, and a further idea is that of surgical indications. There is a considerable amount of consensus regarding the first two, in fact, stability has a definition: the ability of the vertebral column to carry out its physiological functions. However, the great debate centers around indications for treatment, which some classifications (such as the TLICS) base on a points scale, but this appears to be a much more complex matter.
At present, the major question nobody appears to know the precise answer to is how a thoracolumbar fracture will develop, particularly those without any clear radiological signs of instability: basically posterior flexion injury or major communition of the vertebral body. Purely osteoporotic fractures have their “own identity” and their radiological criteria are more difficult to apply. Indeed, the classification used for this type of injury is that of Genant rather than those previously mentioned. It is based on vertebral body deformity from concavity in its endplates, due to a deforming force which does not cause fragmentation of the vertebral body, but plastic deformation of the whole vertebral body by impacted fractures of the degenerated trabecular bone complex. This is not a comparable natural history and this type of injury was excluded from our study.
Furthermore, in normal clinical practice it is not infrequent to see patients presenting with low back pain after a thoracolumbar fracture. One explanation for this may be that pain is irradiated from the thoracolumbar region, but in other cases there is a clear facet syndrome, which could stem from overload of the L5S1 diarthrodial joints (posterior facets) in cases of immobilization of the spine with a brace, particularly if it is a rigid back brace (also widely debated in literature): it seems reasonable to assume that partial immobilization of T12 to L5 must lead to a mechanical overload of L5/S1 joints. Fortunately this low back pain usually disappears on follow-up.
To conclude this introduction, the principal question concerning this study arises: can I predict to what extent will a thoracolumbar burst fracture treated with TLSO result in kyphosis?
The hypothesis is posed that it is possible that a “dynamic”, axial-loaded radiograph is a true test of the mechanical stability of a fracture controlled by a TLSO. Therefore, a standing X-ray was made immediately after fitting the brace on those patients considered suitable for treatment with TLSO and an assessment made of the information gained from the variation between the X-ray of the patient lying down and this Rx0: standing with TLSO, without resting in bed more than necessary to fit the TLSO. The hypothesis is that it will be sufficient to detect more subtle “instabilities” and will relate to the final level of collapse, of kyphosis.
Another question which arises in check-up appointments of these patients is: is there any way of knowing which patients will present with low lumbar pain on follow-up?
A secondary hypothesis puts forward the possibility that a spine in a less stable situation may generate more overload of joints L5S1, which contributes to the above-mentioned low back pain.
The study objectives were:
- (1)
Clinical predictive value of increased vertebral collapse between the supine X-ray on admission and the Rx0.
- (2)
Predictive value of this increase on the radiological result to the consolidation (kyphosis on the X-ray at 3 months).
A prospective study was made of patients with T12 or L1 burst fractures admitted to hospital between January 1, 2011 and December 31, 2012. Following the completion of the appropriate imaging tests in each case, it was decided that treatment with thoraco-lumbar-sacral type orthosis was the treatment of choice, with support in the sternal manubrium; the criteria for this were: Farcy index <25, communition on the sagittal CAT <33% and absence of neurological symptoms. Monitoring was extended until December 2013 (minimum: one year, maximum 2). The series was made up of 50 patients, who were given X-rays on admission (supine), followed by standing x-rays as soon as the TLSO (Rx0) was fitted and subsequently, at 3 months (consolidation and removal of brace), at 6 months and at one year (only when it was considered necessary), no new X-rays were made in successive clinical reviews up to 2 years later.
The variables used were as follows:
- (1)
Demographics: age and gender.
- (2)
Trauma energy, grouped as: (a) standing/low height fall, (b) height fall – precipitation – and (c) traffic accident/run over.
- (3)
Radiological: Farcy index and local kyphosis (Cobb at 3 vertebrae) in X-rays of the before-mentioned radiological protocol. Measurements were taken in the SECTRA computerized digital imaging reader, with the program tools.
- (4)
Clinical: regional pain at fracture level (from referral or through direct digital pressure) and low back facet pain.
The absolute values and increases in the before-mentioned radiological variables were studied, comparing them with the clinical ones. Patients were classified according to age and production mechanism.
Surgery was performed on 4 patients after a standing X-ray with TLSO (Rx0): an instrumented arthrodesis, a percutaneous fixation and two vertebral reinforcements (a kyphoplasty and a vertebtroplasty); this was due to a considerable increase in the Farcy index and/or the appearance of a severe local pain on standing which was relieved on lying down. There were also two follow-up losses: one death and one loss for social reasons. The statistical study was carried out with data from the 44 remaining patients in the hospital's Unit of Epidemiological Research using the R statistical package (ANOVA/Kurskall-Wallis, linear regression, selection of cut-off points, targeted effects).
ResultsAverage age was 62.8+14.5 (24–82), with major bias toward advanced ages, thus the percentiles 25, 50, and 75 of the series were: P25: 50 years of age, P50 (median): 67.5 years of age and P75: 75 years of age. Gender distribution was 30 males and 20 females.
Regarding the type of traumatism: 32 presented with standing/low height fall, 9 with precipitation and 9 with a traffic accident/run over. 36 L1 and 14T12 fractures were observed. Of the 50 patients, 27 were treated in 2012 and 23 in 2011.
The Farcy index on admission was 9.7+2.7 (5–19) and local kyphosis 9°+3° (3–21°).
No surgical intervention was made during follow-up, (which was undertaken in all cases in our center by the same doctor), nor was there any residual pain at thoracolumbar (locoregional) level. Low back pain presented with facet joint characteristics, diagnosed after specific examination in 16/44 patients (32%). Of these, two required a dorsal ramus block to the facet and 14 resolved spontaneously.
1st question: does the vertebral collapse variation on standing up with the brace predict anything about the clinical outcome?
In the linear regression study the only statistical relationship that presented was between the increase in the Farcy index from a recumbent to a standing position (Rx admission to Rx0) and the appearance of low back pain on follow-up (P=.0017) adjusted according to age and gender with neither variables being significant.
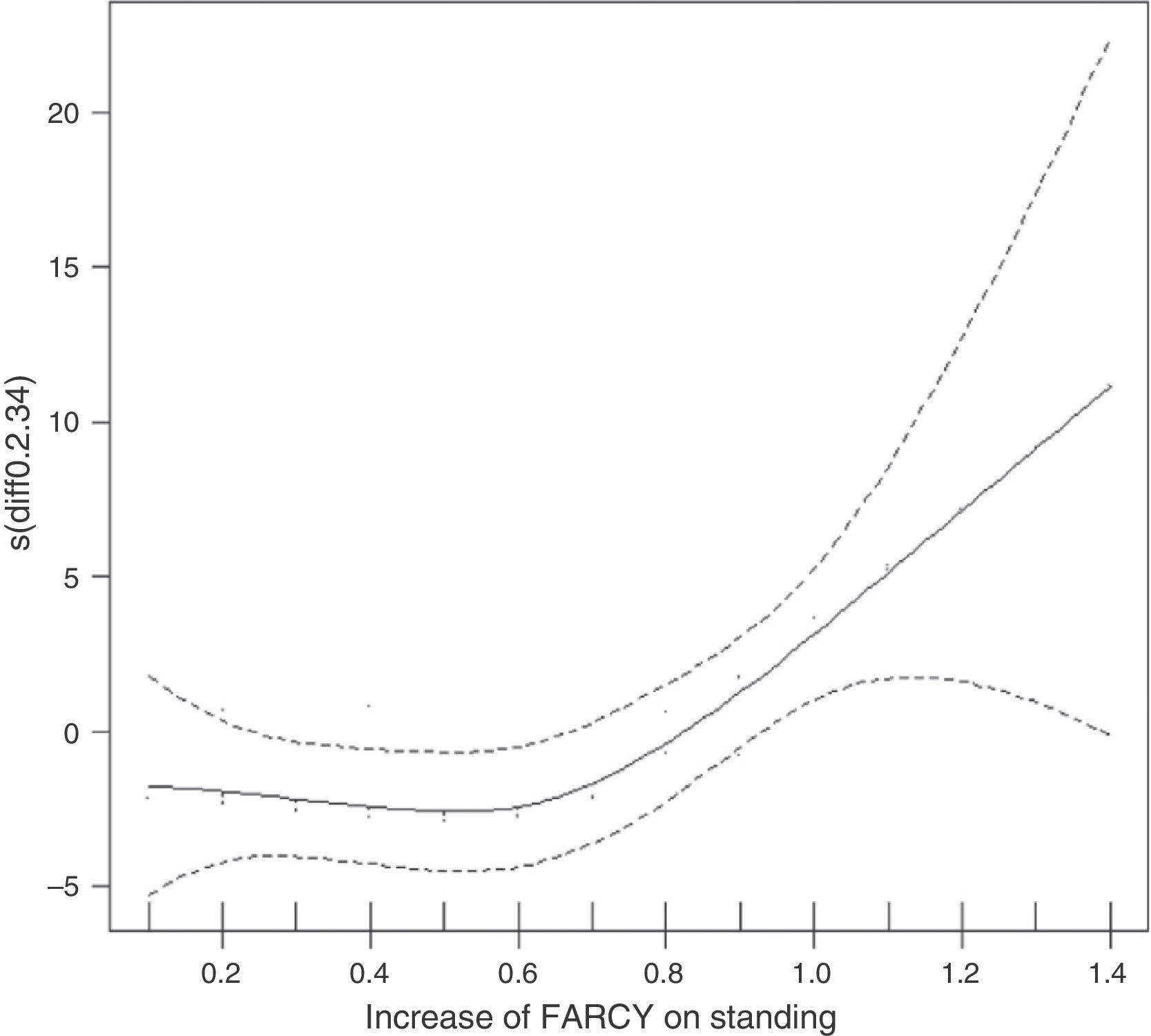
The study of targeted effects shows a cut-off point of 0.7; in other words, if the Farcy index increases by more than 0.7 it is progressively more probable that low back pain will appear in this patient on follow-up (Fig. 1).
2nd question: can final kyphosis be predicted?
On studying the subgroup with the two conditions from a fall from standing/low height and age >60, we observed that if the subgroup of <70 (n=14) was compared with that of >70 (n=19), the increase in Farcy's index was the same: 0.9; but this meant 38% from total collapse up to consolidation in <70years of age and only 25% in >70 years of age. Thus, from 70 years of age onwards the vertebra will collapse more during the first 3 months, taking the Rx0 imaging as reference; in other words, in a patient aged between 60 and 70 of this subgroup, almost half of the collapse up to consolidation (38%) is already visible on Rx0, whilst in patients over 70 only 25% of the predicted final collapse is visible: the fracture has to collapse 3 times more than it would have had the patient been standing up with their TLSO.
The linear regression study showed a correlation between the increase in local kyphosis Rx – admission to Rx0 (local kyphosis Rx0 – local kyphosis Rx admission) and enable any assertion index at 3 months (P=.0048); the correlation being:
Farcy's index at 3 months=10.2+2.8×(local kyphosis Rx0−local kyphosis Rx admission).
R2=0.13; which means the variance of said increase in local kyphosis explains the 13% of variability in the Farcy index and this means that the variable (increase in local kyphosis of Rx admission at Rx0) is a fairly important factor for explaining the changes in outcome (Farcy at 3 months).
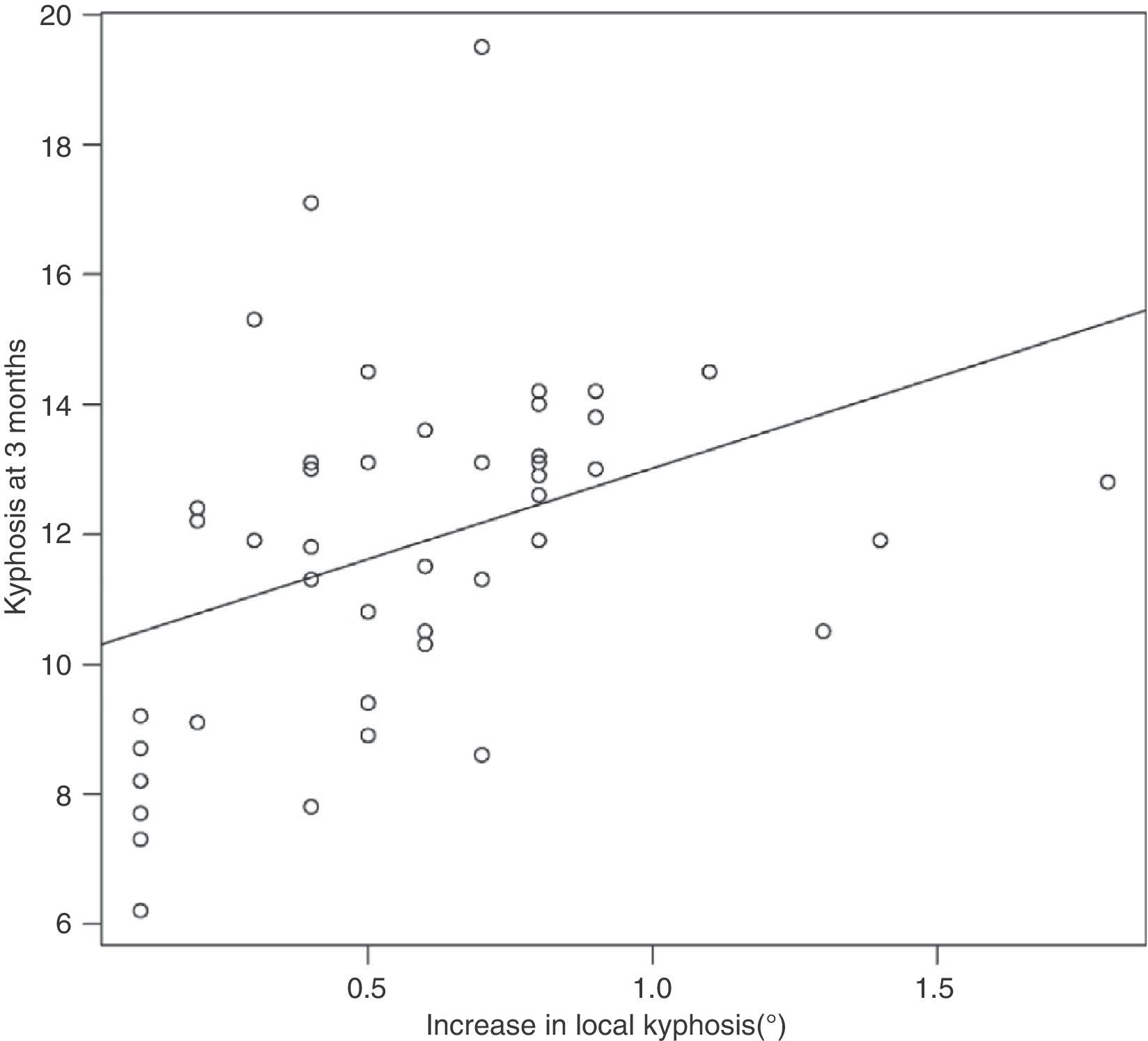
The correlation is even higher between the increase in the local kyphosis Rx admission to Rx0 (local kyphosis Rx0-local kyphosis Rx admission) and said local kyphosis at 3 months (P=.002); (Fig. 2):
Local Kyphosis at 3 months=8.6+4.1×(local kyphosis Rx0−local kyphosis Rx admission).
R2=0.18; therefore the variance of the increase explains the 18% of the variability in local kyphosis at 3 months and is an even more important factor when explaining local kyphosis at 3 months than explaining the Farcy index at 3 months.
Due to the above, it is reasoned that the two chosen ways of measuring kyphosis at 3 months are predictable due to the increase in local kyphosis measured in the supine X-ray on admission and the standing X-ray immediately after fitting the TLSO.
DiscussionIs it worthwhile carrying out a standing X-ray on a patient with a thoracolumbar burst fracture who we decide to treat with a TLSO immediately after fitting it?
Once assessment has been made of the patient with the thoracolumbar burst fracture, which is defined as comminution of the vertebral body with posterior wall fracture, and no neurological complications, and once their additional tests have been evaluated, the first question we must ask is whether the patient is eligible for surgical treatment or not, or better still, if it is worth offering surgical treatment to benefit the future of that patient. In a recent publication of the Cochrane Collaboration (Abodou),7 597 articles appear on initial search, which are only in English or Chinese, but after analysis of the articles, only two were selected: that of Wood from 20038 and that of Siebenga from 2006.9 A meta-analysis of Gnanenthrian,10 reached similar conclusions with the inclusion of another two works which Abodou rejected: there are no differences in clinical outcome at 4 years follow-up, there are further complications and a higher cost in the group of operated patients.
A number of distinctions may be made from reading the articles. Wood compares fractures of T10 to L2 with a kyphosis around 10° for 44 months and Siebenga compares patients with kyphosis at 15° for 4 years and mentions 3/32 L3 or L4 fractures. This very much limits the extrapolation of the study to the patients as a whole since: (a) fractures with this kyphosis are not normally regarded as surgical in the absence of posterior ligament injury (exclusion criteria in both series, together with osteoporosis and age above 60); (b) local kyphosis may have no clinical symptoms for up to 5–20 years,11 and therefore a follow-up of 4 years could be insufficient, and (c) non-surgical treatments are not all the same (plaster cast, orthosis).
In our series the mean of Farcy's index and of local kyphosis were <10 and <10°, with the result that none of them should have benefited from surgical treatment and even so, 4 patients eligible for surgical treatment were identified by standing X-ray with TLSO (Rx0) due to the collapse of their fracture, often accompanied by local pain: even with these levels of vertebral body collapse in the recumbent imaging on admission there could be patients susceptible to more aggressive treatment, in our series 4/50 (8%). It is also true that the aforementioned studies previously were carried out on patients who were 59 years of age at most; whilst in our study the mean age was 63 and the median (P50) was 67.5. Possibly for this reason the standing X-ray with TLSO (Rx0) we propose be introduced into the follow-up protocol of these patients would be even more pertinent in patients at the age of those in our series. Along these same lines, it was mentioned that amongst the patients with standing/low height falls there is at least a clear trend toward final collapse with stratification at 70 years of age, the highest collapse in patients >70 being between X-ray on admission and X-ray at 3 months; statistical significance does not permit any assertion, probably due to the number of patients, but it does tell us that the broken vertebra of a patient over 70 collapses more often than that of a patient between 60 and 70, which does appear to be a logical natural law.
Furthermore, we may roughly assume that there will be final collapse of a fracture, as in patients over 70 it will be 3 times that which has already occured in the standing position (25% on average of total collapse at 3 months has already occurred with the standing position), whilst for patients aged between 60 and 70 the figure is only a little higher (38% on average of total collapse at 3 months has already occurred with the standing position).
Another question which occurred to us even earlier, from a chronological point of view, in evaluating the patient and relevant to treatment, is the assessment of complementary tests. The question is: what is the most useful way of measuring kyphosis resulting from a fracture? Cobb's angle and Farcy's sagittal index were chosen, according to the definitions of the Spine Trauma Study Group,12 the former being the one which was agreed by this group and the latter the traditional one, which also compares the situation post-trauma with the normal anatomy in that area. In a recent publication13 the conclusion was reached that the two measurements least susceptible to error, regardless even of the experience of the research physician, are Farcy's index and Cobb's kyphosis between the cranial vertebra and caudal vertebra to the fractured vertebra (the recently-mentioned Cobb's angle), the latter is sometimes referred to as regional kyphosis, but to avoid confusion with regional kyphosis understood as lumbar kyphosis, we preferred not to use this terminology in our work. Our measurements of kyphosis due to fracture are therefore in keeping with what is most accepted and proposed in scientific literature and we consider them to be validated by it.
However, once we have: (a) measured the images in a validated manner, (b) decided that the patient does not require surgery due to the criteria described in Farcy's index, communition of the vertebral body (validated by Dai, from McCormack's classification, as the only parameter of said classification with a predictive value in patients treated without surgery) and absence of neurological symptoms (stability according to White and Panjabi) and (c) decided that the patient will be treated with a thoraco-lumbar-sacral type orthosis with support in the sternal manubrium, to increase the anti-kyphotic lever arm, since the Jewett brace does not seem sufficiently anti-kyphotic for these patients and the cases created with the Böhler brace were not studied in this series; the question underlying this study remains: can I predict the clinical and radiological outcome of the patient? The conclusions at the end of this discussion provide at least a partial response to this question.
Although it is true that the lumbar-sacral region may present sensitive irradiated symptoms in the thoracolumbar region through T10 to L214 spinal cord nerve branch endings of posterior branches, guided clinical examination may lead to the diagnosis of secondary facet syndrome after thoracolumar fractures. Facet syndrome is fairly frequent amongst the patients in our series (32%), who had all been treated with braces. This could explain an eventual mechanical overloading of the lumbar-sacral joint on reducing movement of the spine to L5. It was therefore observed that if Farcy's index increased by over 0.7 it is progressively more probable that low back pain appears. The situation can be explained to the patient, together with its naturally benign, almost always self-curative process.
The effect of targeted studies is to assess the relationship between two factors with significant association in the linear regression study, giving a zero value to the null effect, positive to a directly proportional relationship and vice verse. We may argue that increases are small, close to the measurement error, but precisely the fact that measurements are made by an independent traumatologist, and always the same person, who is also ignorant of the results, reduces this error. Moreover, the statistical significant differences in results, even with these low values (Farcy increase of >0.7), increase the value of the concept.
ConclusionsImmediate standing X-ray on fitting a TLSO, compared with supine X-ray, indicates:
- (1)
The appearance of lumbosacral pain on follow-up, when the variation in the Farcy index is >0.7.
- (2)
Final kyphosis, measured by the Farcy index and local kyphosis, with mathematical linear regression models.
For this: we recommend an X-ray in patients with a T12 or L1 burst fracture who are to be treated with TLSO as soon as they have adapted to it, probably particularly in patients aged 60 or above.
Level of evidenceEvidence level II.
Ethical responsibilitiesProtection of human beings and animalsThe authors declare that no experiments were performed on humans or animals for this investigation.
Data confidentialityThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Díez-Ulloa MA, Gallego-Goyanes A. Valor pronóstico de la radiografía lateral inmediata en bipedestación con TLSO en pacientes con fractura estallido toracolumbar. Rev Esp Cir Ortop Traumatol. 2015;59:179–185.