To describe our experience in the management of patients with osteogenesis imperfect (OI).
Material and methodsWe conducted a retrospective study of a series of cases affected with OI treated in the Clínica Univesidad de Navarra from 1980 to 2007, with a mean follow up of 17.3 years (7–27 years). We collected descriptive data of the sample, the fractures and the deformities, and the treatments given. The complications presented and the functional outcomes at the end of follow-up were also reviewed.
ResultsThe sample included ten patients. Approximately two-thirds (65%) of fractures were sustained in the lower limbs. One patient received medical treatment only. Three patients had combined medical and surgical treatment. Some type of surgical treatment was performed on 6 patients. The most common surgery was the Sofield-Millar performed on 37 occasions, with a third of them requiring revision surgery due to migration of the nails. There were 17 episodes of re-fracture. Complications such as non-union, iatrogenic fractures, and infections, were also observed. The functional outcome, according to the Hoffer-Bullock scale, at the end of follow-up was grade I/II in 7 patients.
ConclusionsDespite the need for multiple interventions and complications presented during follow up, the appropriate treatment of patients with OI can provide acceptable functional outcomes.
Describir nuestra experiencia en el manejo de los pacientes afectos de osteogénesis imperfecta (OI).
Material y métodosHemos realizado un estudio retrospectivo de una serie de casos afectos de OI tratados en la Clínica Universidad de Navarra desde 1980 hasta 2007 con un seguimiento medio de 17,3 años (7–27 años). Se han recogido los datos descriptivos, los referentes a las fracturas y a las deformidades observadas y los tratamientos realizados, las complicaciones presentadas y la capacidad funcional al final del seguimiento.
ResultadosLa muestra revisada consta de 10 pacientes. El 65% de las fracturas sufridas se encontraban en miembros inferiores. Un paciente recibió exclusivamente tratamiento médico. En 3 pacientes se asoció tratamiento médico y quirúrgico. En 6 pacientes se realizó algún tipo de tratamiento quirúrgico. La intervención quirúrgica más frecuente fue la de Sofield-Millar, realizada en 37 ocasiones. Un tercio de estas requirieron cirugía de revisión por migración de los clavos. Se observaron 17 episodios de refractura. Además, se han observado complicaciones como seudoartrosis, fracturas iatrogénicas e infecciones. La funcionalidad al final del seguimiento era de grado I o II según la escala de Hoffer y Bullock en 7 pacientes.
ConclusionesA pesar de la necesidad de múltiples intervenciones y de las complicaciones presentadas durante el seguimiento, el tratamiento adecuado de los pacientes afectos de OI puede proporcionar resultados funcionales aceptables.
Osteogenesis imperfecta (OI) is a bone dysplasia caused by an alteration in the synthesis of type I collagen, implying abnormal bone formation. The most outstanding of its clinical manifestations is progressive bone deformity, associated with fractures or not, delayed growth, the presence of bluish sclera, anomalies in the development of teeth and hearing loss.1
The classic clinical forms of OI comprise Lobstein's type and Vrolik's type. The first manifests in variable ways, with a greater or lesser degree of deformity and onset of fractures during growth and adulthood. The second is a severe form that is observable from birth, with frequent intrauterine fractures and a high mortality rate.1 Sillence et al.2 classified the disease into 4 types depending on symptom severity and progression. An additional four types have recently been described.1,3
The fundamental goals in terms of managing patients with this disease are: to increase the amount of bone formed and to improve its quality, to prevent the appearance of bone deformities and to treat fractures. Bisphosphonates are the only drug group seeming to have a beneficial effect on bone quality.1,4–6 Deformities can be prevented or treated by means of the use of orthesis7 and surgery.8
In 1959, Sofield and Millar5 described a technique to stabilize the bone and correct the deformity: successive osteotomies were performed on the long bones and associated with endomedullary nailing. Nowadays, a variation of this technique is applied using extensible endomedullary nailing thanks to which the adaptability of the implant to the bone is improved and the re-operation rate is reduced.9
The aim of the present paper is to describe the results obtained in the treatment of OI patients at our center.
Material and methodsWe have conducted a retrospective study of a case series of OI patients treated at our center from 1980 to 2007, with a mean follow-up of 17.3 years (7–27 years). The cases were taken continuously from the hospital's case history register, excluding those with a follow-up of less than 5 years.
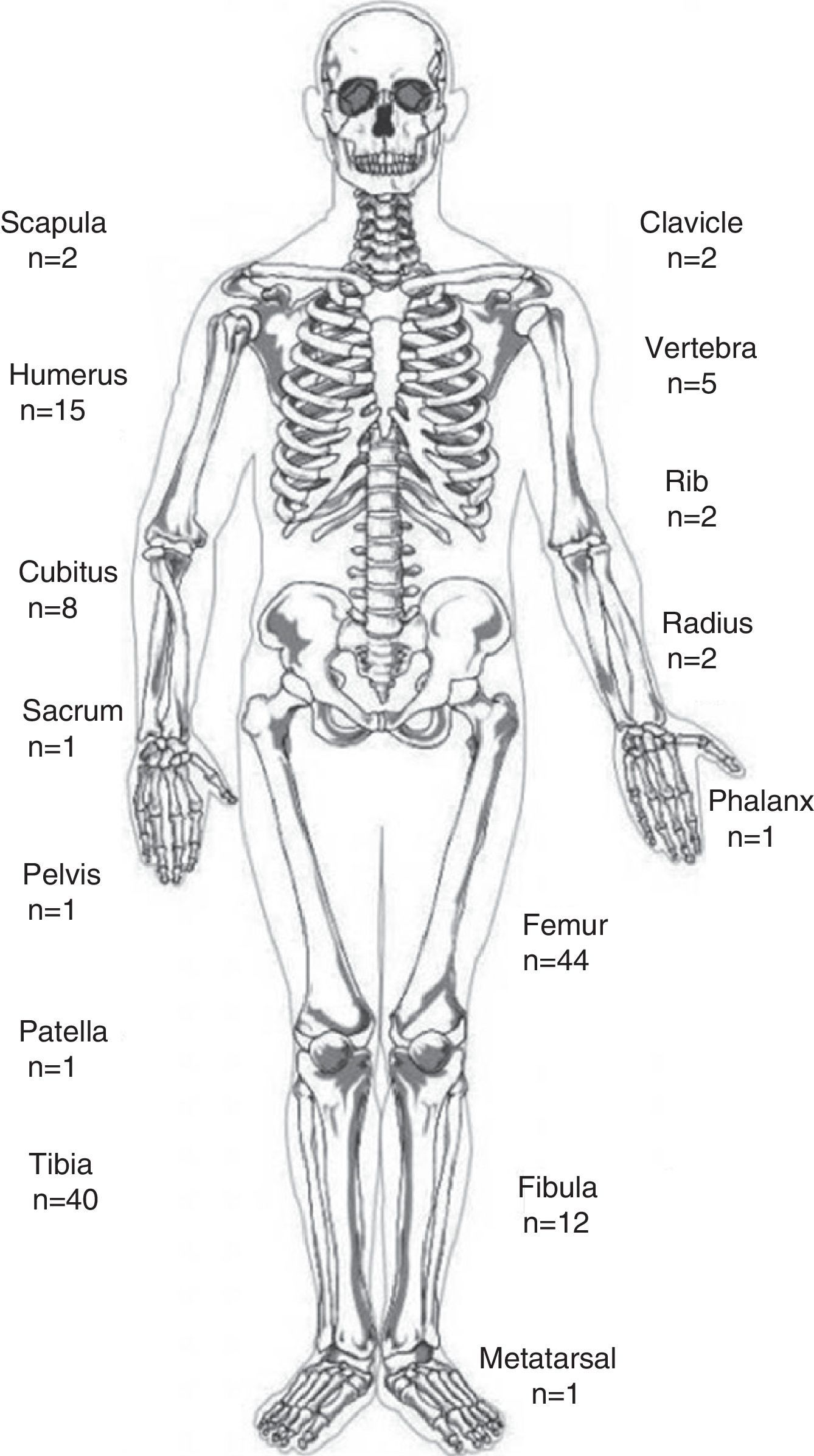
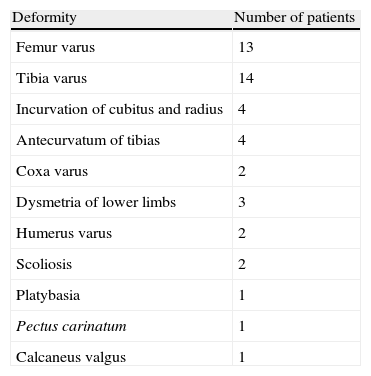
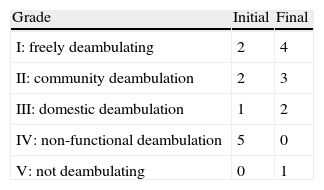
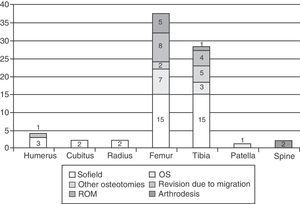
The sample in our study has a total of 10 patients with a mean age, at the moment of the first consultation, of 12.7 years (4–41). Eight of them were diagnosed as having the clinical form described by Lobstein, one with Vrolick's and one with Van der Hoeve's. Nine were diagnosed as having OI during the first year of life, whereas one was only identified in the fourth decade of life. The deformities observed in the long bones of the patients in the series are shown in Table 1. These included 149 fractures: 98 in the lower limbs, 40 in the upper limbs and 11 in bones in the axial skeleton. Their exact location is shown in Fig. 1.
The descriptions given cover the treatments applied, either medical or surgical (Sofield-Millar intervention, reintervention due to migration of nails, osteosynthesis with plates, simple corrective osteotomies and other procedures), their complications and the results in terms of the patients’ functional capacity according to the Hoffer-Bullock scale10 at the end of the follow-up. The study has evidence level IV.
ResultsFour patients were subjected to medical treatment through the administration of bisphosphonates (alendronate) during a mean period of 3.3 years (1–5 years). In 2 of these, calcitonin was associated for 2 and 3 years, respectively. All patients received this treatment during adolescence or adulthood and were patients affected by mild forms of the condition. The doses and administration of the anti-resorption treatments were adjusted for weight and age.
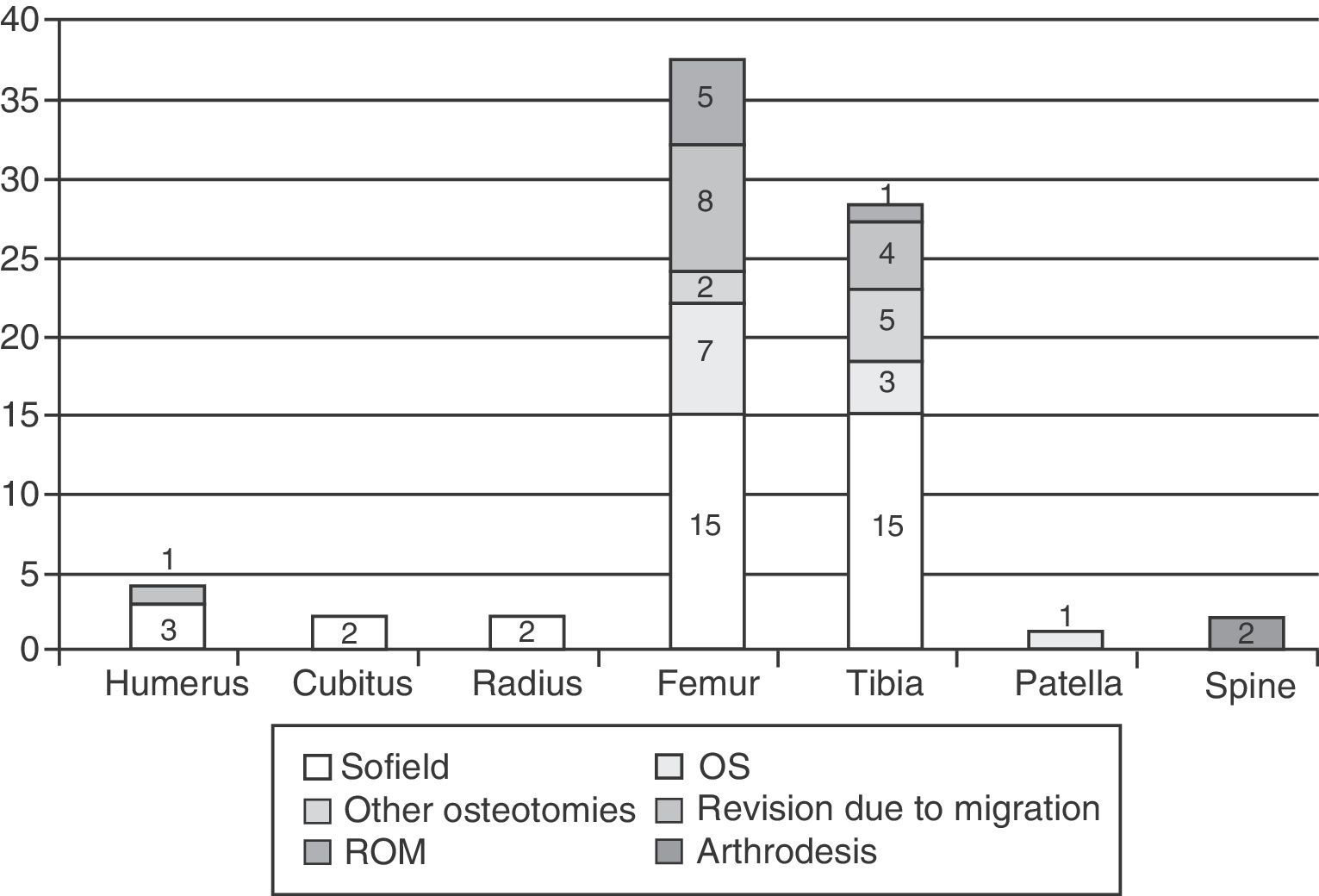
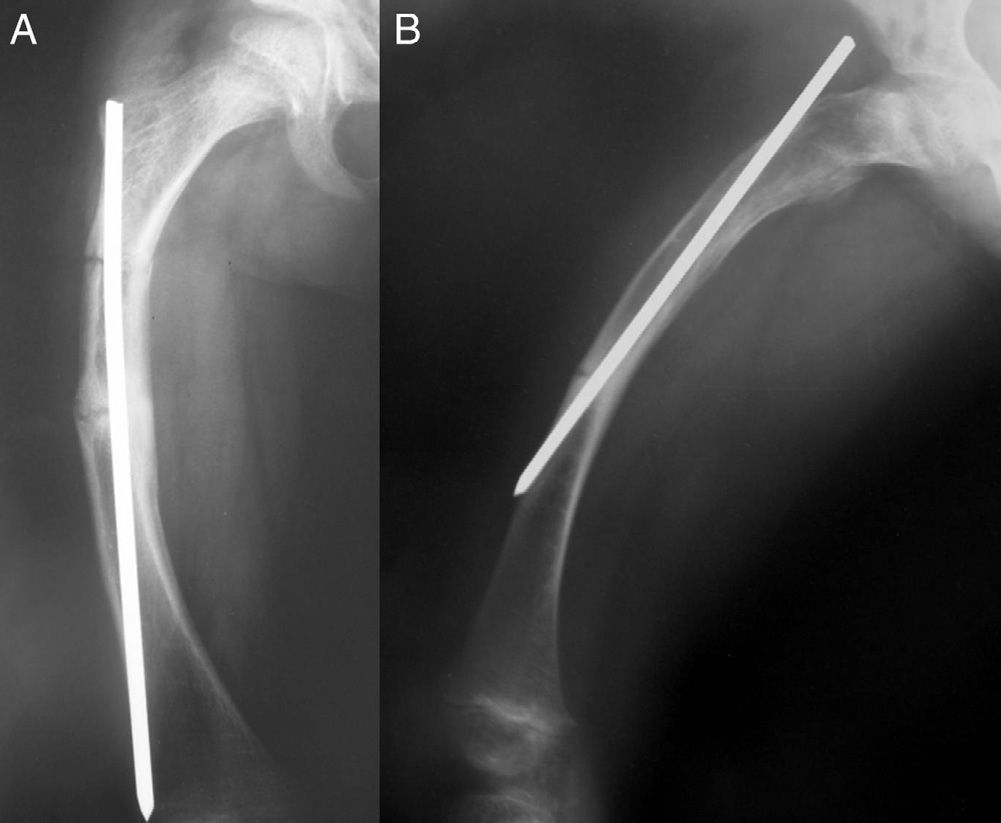
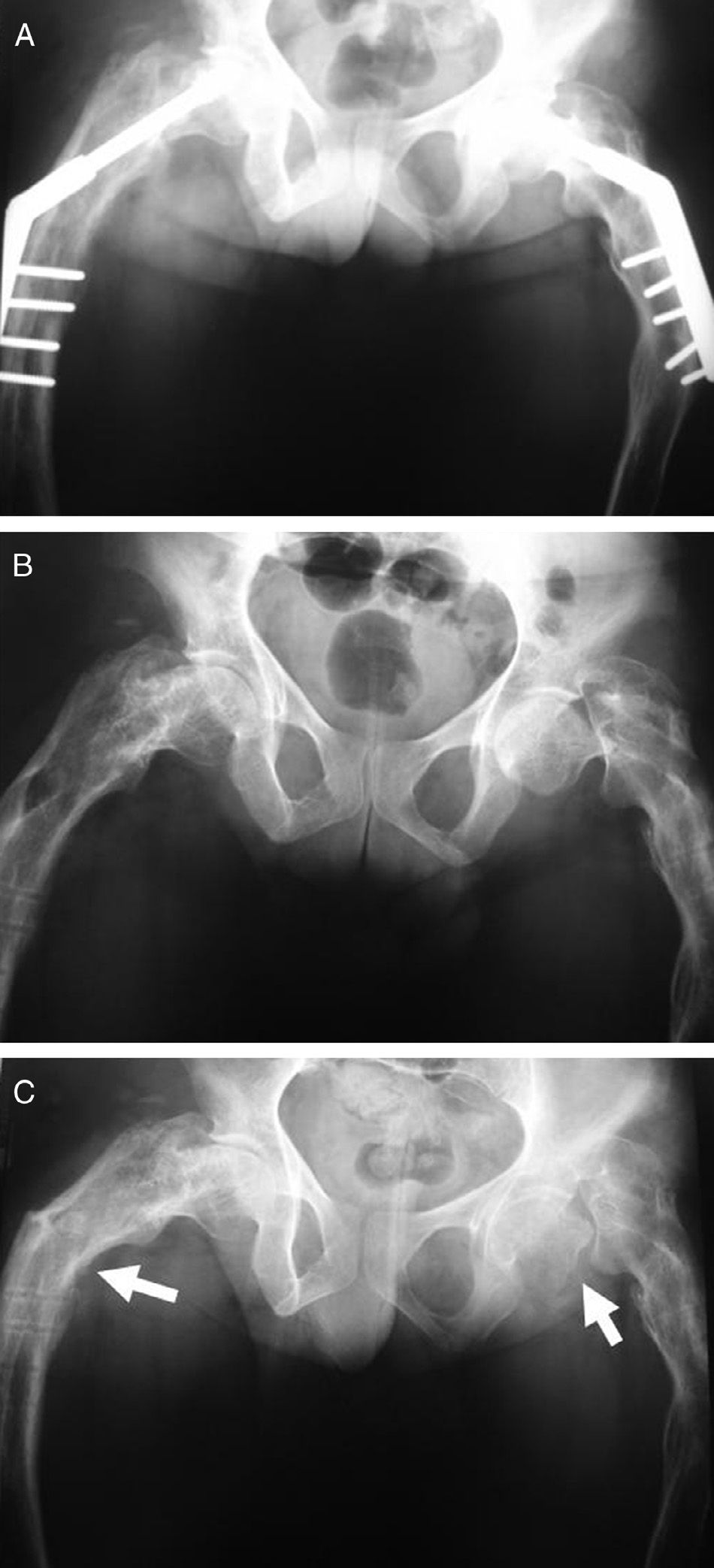
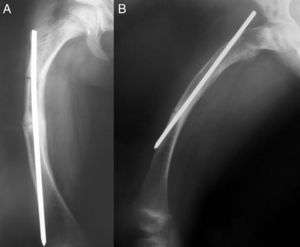
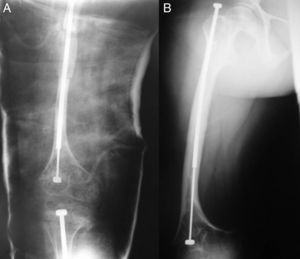
Seven patients underwent some kind of surgical treatment, with a total of 83 procedures being performed, 75 of them on the lower limbs (Fig. 2). The most frequent was the Sofield-Millar intervention, which was applied on 37 occasions: 33 with rigid endomedullary nails (Figs. 3 and 4) and 4 with extensible endomedullary nails. In 11 cases, an open reduction was performed followed by osteosynthesis with plate and screws. On 7 occasions, it was necessary to perform corrective osteotomies on deformities and 6 procedures were for the removal of osteosynthesis material. A total of 13 surgical revision procedures were required due to migration of the endomedullary nails.
Seven-and-a-half-year-old patient operated on with a telescopic endomedullary nail for correction of a deformity in the femur (A). At age 15, the nail has hardly migrated at all and the shaft has been lengthened to adapt to bone growth (B). The patient did not require reintervention at any time during follow-up.
Two patients were operated on for scoliosis using posterolateral arthrodesis and posterior hybrid instrumentation; on 4 occasions elongation was performed on the lower limbs secondary to dysmetria (3 in the tibia and one in the femur).
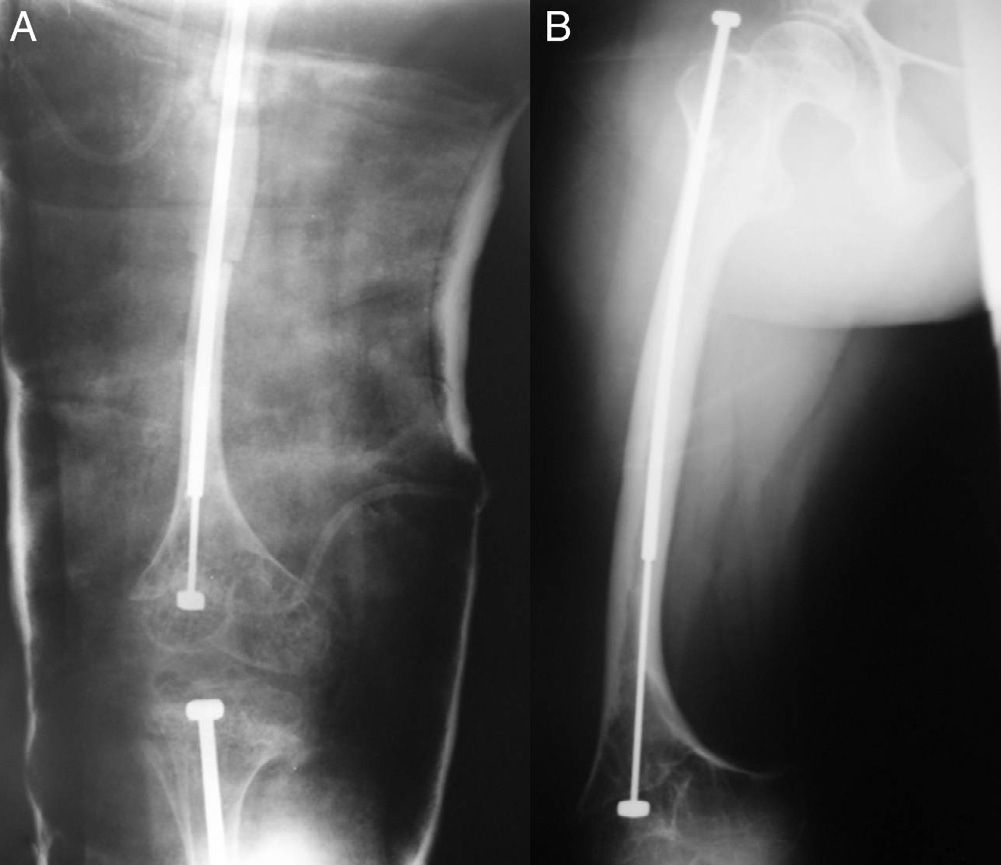
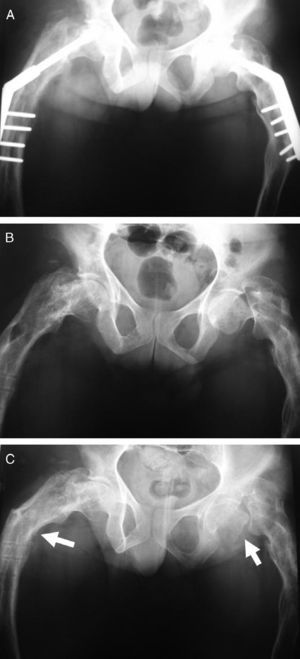
Other complications recorded, in addition to the migration of endomedullary nails, were 17 refractures: 13 following a Sofield-Millar intervention, all on long bones, 3 following elongation and one after removing osteosynthesis material (Fig. 5). The record also reflects 5 pseudoarthroses (3.5% of the total fractures), one infection of a surgical wound, one osteomyelitis treated with extensive debriding, and one recurrent seroma.
Thirty-year-old patient operated on for a fracture of the 2 proximal femurs with a bilateral screw and plate (A). Three months after removal of the osteosynthesis material she suffered a basicervical fracture of the left femur (B). One year later, the fracture is in pseudoarthrosis and there is a fracture in the contralateral femur. (C) The patient is incapable of deambulation.
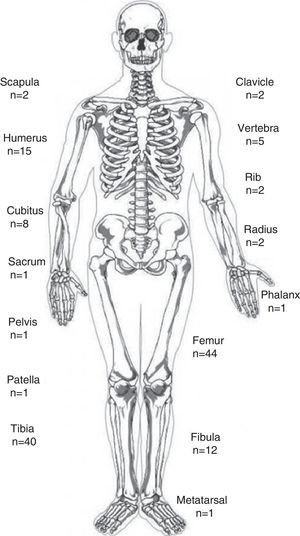
The treatment outcomes by patient functionality according to the Hoffer-Bullock scale10 are summarized in Table 2.
Evolution of patients’ deambulation abilities.
| Grade | Initial | Final |
| I: freely deambulating | 2 | 4 |
| II: community deambulation | 2 | 3 |
| III: domestic deambulation | 1 | 2 |
| IV: non-functional deambulation | 5 | 0 |
| V: not deambulating | 0 | 1 |
Source: based on the Hoffer-Bullock scale.10
Thanks to the development of genetic diagnosis, seven forms of OI have been described so far. Five have a known genetic origin and 2 correspond to patients presenting an OI phenotype without the characteristic mutations in the genes involved in this disease. Sillence types I–IV present mutations in some of the genes expressing type I collagen.1,3 In general, the mildest forms occur due to mutations of an allele in the COL1A1 gene and translates into a reduction of the synthesis of type I collagen; while the most severe forms synthesize a normal amount of structurally altered type I collagen.11 Despite the advances in understanding the disease's etiopathogenesis and discoveries in the field of genetics,4,5,11 the basis for treating this condition has remained unchanged in recent years.
The aim of treatment is to provide an acceptable functional capacity in the longer term, enable bipedestation and autonomous gait by patients.12 They must be handled by means of multidisciplinary teams due to the disease's complexity and wide variability.13 From a pharmacological standpoint, different strategies have been used, such as growth hormone, sodium fluoride or vitamins C and D among other molecules,6 although the results obtained have been discouraging.
The introduction of bisphosphonates for the treatment of OI has improved outcomes.4–6,14 The patients treated improve in both the illness's clinical expression and in the increase in the thickness of cortex bone and the densitometric parameters.1,6,14–16 Some authors have described a reduction in the early fracture rate in children with type III OI15 treated with endovenous bisphosphonates.17 In the same way, others have described a lower number of fractures, as well as improvements in gait and function in patients with type VI OI.1 The same treatment has also led to an improvement in densitometric parameters and the same decline in the incidence of fractures.14 So far, however, it is not been possible to demonstrate the efficacy of these drugs in the prevention of deformities.1 In our study, 4 of the 10 patients received medical treatment with oral bisphosphonates for periods of between one and five years. All patients received treatment during adolescence or in adulthood and suffered mild forms of the illness, so we can determine the beneficial effect of the measure.
In the most severe forms of OI, surgical treatment of fractures or deformities is occasionally necessary.18 One of the most common techniques is that described by Sofield and Millar,5 comprising the correction of the deformity and subsequent stabilization through implantation of an endomedullary device to act as an internal ferrule.19 The classical technique presented a high rate of complications related to the osteosynthesis material when migration or extrusion of the osteosynthesis material occurred, potentially causing additional fractures at the ends of the nail, and the possibility of recurrence of the bone deformity.5 New techniques have currently been developed to reduce the complications related to the surgical approach20 and implants. Thus, the improvement in telescopic nail design has represented a real revolution21,22 in comparison with previous designs.23
In our series, Sofield-Millar interventions were the most frequent. As with others,18,24 the bones most frequently operated on were those of the lower limbs, since they are load-bearing bones, and the correction of their deformities is decisive for ensuring bipedestation and deambulation. Some authors have presented re-intervention rates of up to 60%,19,20,24 with the main cause in the Sofield-Millar technique being the migration of endomedullary nails. In our experience, we have had to perform a second intervention in 35% of patients who underwent that technique, in contrast with migration-based revision rates in excess of 80% of cases with rigid nails, and refractures in 10% of cases in another study.20
In cases involving telescopic nails, we have observed the breakage of the distal shaft of one of the nails implanted and one case of refracture resolved with conservative treatment. Jerosch et al.18 observed refracture rates of 22% and Bailey and Dubow migration rates of 44% with telescopic nails, while Esposito and Plotkin19 presented a lower number of revisions with telescopic nails.
Patients who underwent osteosynthesis with plates represented 13% in our series. In one of the cases we observed a refracture adjacent to a prior osteosynthesis plate, while another suffered a refracture of the left femoral neck a few months after removing the osteosynthesis material from both hips and, one year later, suffered a sub-trochanter fracture of the contralateral femur (Fig. 5). Up to 69% of complications have been described in patients with type III OI treated with blocked osteosynthesis plates,25 casting doubt on the advantages of this kind of implant in the most severe forms of the disease.26
Bearing in mind that the main goal in treating these patients is to provide an acceptable functional capacity in the longer term in order to enable bipedestation and autonomous gait and, although there is a certain degree of variability in terms of the expected functionality, gait autonomy might range from 33% in patients with type III OI to 100% in type I.27 In our series, we have obtained functional outcomes that are comparable to those of other studies described in the literature.13,19
ConclusionsDespite the need for multiple interventions and the complications seen during follow-up, adequate treatment of patients with OI can provide acceptable functional outcomes.
Evidence levelEvidence level IV.
Ethical responsibilitiesProtection of persons and animalsThe authors declare that no experiments have been conducted on human beings or on animals for this research.
Data confidentialityThe authors declare that they have complied with the protocols in place at their workplace on the publication of patient data and that all the patients included in the study received sufficient information and gave their informed consent in writing to take part in this study.
Right to privacy and informed consentThe authors declare that no patient details appear in this article.
Conflict of interestThe authors have no conflict of interests to declare.
Please cite this article as: Escribano Rey RJ, Duart-Clemente J, Martínez de la Llana O, Beguiristáin Gúrpide JL. Osteogénesis imperfecta: tratamiento y resultado de una serie de casos. Rev Esp Cir Ortop Traumatol. 2014;58:114–119.