Patellar tumours are rare. They typically appear in young patients, and present with a non-specific pain in the knee.
Giant cell tumours (GCT) are benign, but locally aggressive.
Although they are usually found around the knee (40–60%), those affecting the patella have been classically described in the literature as uncommon.
We describe the case of a 19-year-old male complaining of pain in his knee, whose clinical examination suggested a meniscal tear. Plain radiological examination, as well as MRI, revealed a well-circumscribed lytic lesion within the patella.
The patient underwent arthroscopic surgery, during which an incisional biopsy was performed.
Following pathology reports, which confirmed the suspected GCT, definitive surgery was performed.
At 56months after the surgery the patient remains asymptomatic and free of disease.
Los tumores en la rótula son poco frecuentes. Suelen afectar a pacientes jóvenes y se presentan como dolor inespecífico en la rodilla.
El tumor de células gigantes (TCG) del hueso es un tumor benigno, pero localmente agresivo.
Aunque la localización alrededor de la rodilla es muy frecuente, llegando a ser de hasta el 40–60%, la afectación de la rótula se ha descrito clásicamente en la literatura como casos aislados.
Presentamos el caso de un varón de 19 años de edad, que acude a nuestra consulta presentando clínica meniscal. En el estudio radiológico se descubre de forma incidental una lesión lítica en la patela.
Tras el estudio mediante resonancia magnética nuclear (RMN), se confirma el carácter benigno de la lesión, y en el mismo acto quirúrgico extraemos una biopsia incisional de la rótula.
El estudio histológico confirma la sospecha de TCG, por lo que en un segundo tiempo quirúrgico se realiza el tratamiento definitivo.
El paciente a los 56 meses de la intervención está asintomático y libre de enfermedad.
Patellar tumours are rare and usually affect young patients. They are frequently benign, in a proportion of 70%,1,2 with osteosarcoma being the most frequent malignant entity, in 6% of cases. The most common types found in this location are giant cell tumours (GCT) and chondroblastomas.1,2
GCT of the bone is a benign tumour, albeit locally aggressive, with a high recurrence rate, in up to 65% of cases, and the ability to metastasise, in about 1%–2% of cases, mainly in the lung and after several surgeries by haematogenous dissemination.3,4 In addition, it may become malignant into sarcoma in up to 5%–10% of cases, so it is considered as an intermediate grade tumour. In general, involvement of the patella has been described in the literature as isolated cases.1,2
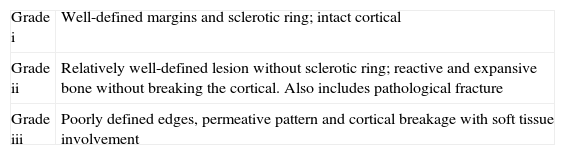
Its diagnosis requires a bone biopsy2,4–10 and its definitive treatment requires radiological staging as described by Campanacci et al. (Table 1).4 Moreover, treatment should also take into account the Enneking radiological stage for musculoskeletal tissue benign tumours.11
Radiographic staging.
| Grade i | Well-defined margins and sclerotic ring; intact cortical |
| Grade ii | Relatively well-defined lesion without sclerotic ring; reactive and expansive bone without breaking the cortical. Also includes pathological fracture |
| Grade iii | Poorly defined edges, permeative pattern and cortical breakage with soft tissue involvement |
The aim of this treatment is to eliminate the tumour with the lowest possible recurrence rate, as well as to obtain optimal and early function.5,7,9 At present, the most common options proposed are intensive curettage with a high-speed bone mill, use of chemical or thermal adjuvants and filling with a bone graft or polymethylmethacrylate (PMMA) in some Campanacci degree III cases.7–9
We report this case due to its anecdotal GCT patellar involvement, its incidental diagnosis and to rule out the need for thorough treatment in order to prevent recurrences.
Case reportThe patient was a 19-year-old male who was admitted to our clinic presenting right gonalgia with several months of evolution secondary to indirect trauma.
Upon examination, the patient presented positive signs of medial meniscus tear, without pain upon palpation and mobilisation of the patella.
A radiological study showed an excentric lytic lesion, well defined and with a sclerotic ring which occupied the upper 2/3 of the patella (Campanacci grade I) and with Enneking stage I (latent) (Fig. 1A).
A study by nuclear magnetic resonance (NMR) revealed a lesion of low to moderate intensity on T1-weighted sequences and heterogeneous on T2-weighted sequences (Fig. 1B), which occupied the upper 2/3 of the patella without invading the cortical or the articular cartilage. This confirmed the benign nature of the lesion, as well as a tear in the red zone of the posterior horn of the medial meniscus.
With this diagnosis, we proceeded to request an analysis to determine the serum calcium and phosphorus contents. Both were reported as normal, thus ruling out primary hyperparathyroidism which may be associated with a brown tumour.
An intact patellar cartilage was observed during knee arthroscopy, conducted in a first surgical stage, as well as a detachment of the posterior horn of the internal meniscus which was sutured by 2 anchors. After closing the arthroscopic portals, we proceeded to perform an incisional biopsy of the patella, using a 2.5 drill.
Once we obtained histological confirmation (Fig. 2), we conducted a bone scintigraphy scan to rule out a multicentric nature of the tumour, common in atypical locations. We also obtained a chest radiograph to exclude the possibility of lung metastases.
After 2 weeks without load and limitation of joint balance to 0–90° due to meniscal suture, we proceeded to perform definitive surgery.
Intensive curettage was performed through a wide anterior window. We removed the tissue and referred it for pathological anatomy (Fig. 3).
Subsequently, we completed curettage with a high-speed mill and, after protecting the surrounding soft tissues, applied phenol with a sterile swab for 5min. Next, we neutralised this compound by washing with alcohol and abundant saline solution. After obtaining an iliac crest graft from the patient, we proceeded to fill the cavity and reinforce it with a polydioxanone (PDS) tape cerclage.
The patient was immobilised with an inguinal-foot cast for 3 weeks and no load, and subsequently started rehabilitation for 2 months.
After 15 days, we removed the stitches without observing foci of necrosis in the surgical wound. Follow-up consultations took place at 6 weeks, 4 months and annually thereafter. A chest radiograph was obtained after 1 year, which ruled out the presence of metastasis. Moreover, annual radiology and MRI monitoring revealed no signs of tumour recurrence (Fig. 4).
At 56 months after surgery, the patient remains asymptomatic and free of disease.
DiscussionTumours in the patella are rare. In their series from 2001, Mercuri and Casadei1 conducted a literature review from 1900 to 2000 and found 384 patients described as isolated cases.
The most common are GCT and chondroblastomas, with percentages of 33% and 16%, respectively.
Clinically, they appear as nonspecific pain in the knee, and in the radiological study they are excentric, radiolucent lesions. Therefore, lateral and anteroposterior radiographs of the knee are recommended in patients with these symptoms.1,2
Although, as previously mentioned, GCT is the most common neoplasm in the patella, patellar involvement is anecdotal in extensive series of this tumour.3–7,9,12,13
Diagnosis is usually obtained by nonspecific pain symptoms in the knees of young patients,1,2 unlike our case, who presented meniscal symptoms relative to a previous trauma, and whose discovery was an incidental radiographic finding.
The radiological study revealed an excentric and expansive lytic lesion, with more or less defined margins, which was classified according to the staging of Campanacci et al.4 to determine its degree of aggressiveness (Table 1). Liquid levels were observed in the tumour and considered secondary to an aneurysmal bone cyst (ABC) component.10
The study should be expanded with magnetic resonance imaging (MRI) or computed tomography (CT) scans, in order to determine if there is involvement of the soft tissues or joints, as well as calcium and phosphorus serum level analysis to rule out primary hyperparathyroidism which could indicate a brown tumour.1,2,4,5,8,14 A bone scintigraphy scan is also recommended so as to rule out multicentric involvement, which may appear with this tumour.12,15
A bone biopsy is the fundamental test to confirm the histological diagnosis before definitive surgery.5,7,9,16 It can be conducted by puncture with trocar biopsy, recommended in locations with difficult surgical access,16 although this may not obtain the amount of tissue required for diagnosis, or by incisional biopsy, as in our case.
Wurtz8 recommends performing an intraoperative bone biopsy and waiting for histological confirmation before deciding on the treatment to be performed.
Mercuri and Casadei1 discuss controversies in obtaining a biopsy. They prefer frozen sections, but note the possibility of contamination. Sample collection with a needle may obtain insufficient tissue, so they recommend incisional biopsy whenever diagnostic doubt exists, always being careful not to affect the patella, quadriceps tendon, joint cavity and synovial membrane, so as to prevent haematogenous spread.
Other authors such as Jain et al.16 recommend needle aspiration for the diagnosis of GCT in unusual locations.
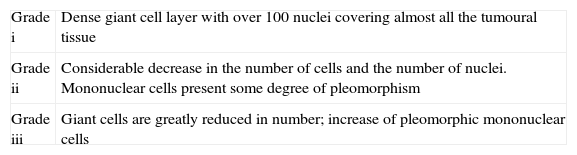
Attempts to correlate tumour histology with its behaviour have been unworkable, and many authors agree that GCT grading is useless, since the prediction of evolution based on histological appearance is impossible. The classical authors describe 3 histological grades (Table 2).17
Histological grades.
| Grade i | Dense giant cell layer with over 100 nuclei covering almost all the tumoural tissue |
| Grade ii | Considerable decrease in the number of cells and the number of nuclei. Mononuclear cells present some degree of pleomorphism |
| Grade iii | Giant cells are greatly reduced in number; increase of pleomorphic mononuclear cells |
In the past, it was considered as a very aggressive tumour, so a radical resection was performed, based primarily on limb amputation.5,18,19 Blodgood, in 1912, was the first author to propose graft curettage for treatment of GCT, obtaining a recurrence rate of 40%–60%, which reached up to 85% in cases affecting the hand. In a review conducted in 2008 by the German group of tumours, Ghet was not able to determine the tumour presentation factors which indicated more aggressiveness, and therefore recommended limb preservation as a priority.7
At present, the recurrence rate varies between 27% and 50% in cases where simple curettage is performed, with or without graft filling.7–9
Intensive curettage consists in performing a wide bone window to expose the tumour, curettage with high-speed mill, use of adjuvants which enhance the resection margins (1.5–2mm in spongy tissue and 0.5mm in cortical tissue) and filling the cavity with bone graft or PMMA.3,5–9,13,20 Protection of the soft and adjacent tissues is essential when using these adjuvant compounds, in order to avoid complications due to the necrosis which they cause.7,9 Regarding the type of adjuvants, these may be chemical, such as phenol and cryotherapy with liquid nitrogen and thermal, such as PMMA. Phenol was introduced by McDonald et al. in 1986,21 obtaining a decrease in the recurrence rate from 50% to 25%. Cryotherapy22 is associated with a low recurrence rate, ranging between 11% and 36%, but has been linked to a high rate of complications, such as soft tissue necrosis. Therefore, in our case we used phenol as an adjuvant. Due to the youth of our patient, and after assessing the treatment by Pury et al.13 in children and adolescents, we decided to fill the cavity with iliac crest autograft, leaving the use of PMMA as an alternative for possible recurrences.
The postoperative follow-up of these patients should be careful, with reviews at 6 weeks, every 4 months during the first 2 years, every 6 months until the fifth year and annually until the tenth year, obtaining a chest radiograph every year.7–9
Our patient has followed such reviews without signs of metastasis or recurrence, and after 56 months is currently asymptomatic and free of disease. This is an excellent result when compared with the latest published studies, which found a recurrence rate between 27% and 50%,7–9 thus supporting the need for a thorough treatment in order to prevent recurrence of this lesion.
ConclusionsGiven a lytic lesion in the patella we should consider the possibility of a GCT and thus obtain a biopsy to confirm it. Intensive curettage associated with phenol and filling the cavity with bone graft has proven an effective treatment in this case.
Ethical responsibilitiesProtection of human and animal subjects. The authors will declare that the procedures followed were in accordance with the regulations of the responsible Clinical Research Ethics Committee and in accordance with those of the World Medical Association and the Helsinki Declaration.
Confidentiality of Data. The authors will declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consent. The authors must have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence must be in possession of this document.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Escribano Rueda LC, et al. Tumor de células gigantes en rótula: a propósito de un caso y revisión de la literatura. Rev Esp Cir Ortop Traumatol. 2012;56:486–90.