Surgical site infections (SSIs) are complications that predispose to a high risk of unfavourable surgical outcomes. The aim of this study was to assess the SSI rate in this type of patients and their prognosis with similar treatment.
Materials and methodsA retrospective case series of 799 patients above 18 years old with spinal instrumentation surgery, between January 2010 and December 2014 in the traumatology and orthopaedic surgery department of our institution. All patients with SSIs were treated by debridement, graft replacement, retention of the instrumentation and lengthy courses of antimicrobial therapy. The patients were followed up for a period of 12 months.
ResultsOf all the patients with arthrodesis, 32 (4%) had spinal SSIs. Three patients were lost to follow-up. The final sample analyzed comprised 29 cases, with a median age of 54.9 years (IQR, 45.7–67 years) and a Charlson comorbidity index of 2.0 (IQR; 0–3). A microbiological diagnosis was obtained in 75.8% of the cases. Of these, the ISSs were monomicrobial in 68.2% and polymicrobial in 31.8%. Once treatment had been completed, 96% were cured without sequelae, and the rate of recurrence and reoperation was 4%.
ConclusionsTreatment based on debridement, retention of the instrumentation, graft replacement and lengthy courses of antimicrobial therapy seems a very effective strategy in the treatment of patients with deep surgical site infection in spine surgery.
La infección profunda de la herida quirúrgica (IPHQ) es una complicación que predispone a un alto riesgo de fracaso en cirugía raquídea con fijación vertebral. El objetivo del presente estudio ha sido valorar la tasa de IPHQ en este tipo de pacientes y su pronóstico siguiendo un abordaje terapéutico homogéneo.
Material y métodoEstudio observacional retrospectivo en el que se incluyó a 799 pacientes mayores de 14 años, intervenidos de cirugía raquídea con fijación vertebral entre enero de 2010 y diciembre de 2014, en el Servicio de Traumatología y Cirugía Ortopédica de nuestro centro. Todos los pacientes diagnosticados de IPHQ fueron tratados de forma homogénea mediante desbridamiento, sustitución del injerto óseo, retención del implante y tratamiento antimicrobiano de 8 semanas. Tras finalizar el tratamiento, los pacientes fueron seguidos durante un periodo de 12 meses.
ResultadosDe total de los pacientes tratados mediante artrodesis, 32 (4%) tuvieron una IPHQ. Tres pacientes fueron perdidos en el seguimiento. La muestra final analizable fue de 29 casos, los cuales tenían una mediana de edad de 54,9 años (IQR: 45,7-67 años) y un índice de comorbilidad de Charlson de 2,0 (IQR: 0-3). El diagnóstico microbiológico fue establecido en el 75,8% de los casos. De ellos, la IPHQ fue monomicrobiana en el 68,2% y polimicrobiana en el 31,8%. Con el abordaje terapéutico aplicado curaron sin secuelas el 96% y la tasa de recidivas y reintervención fue del 4%.
ConclusiónEl tratamiento mediante desbridamiento, retención, sustitución del injerto y tratamiento antimicrobiano de 8 semanas parece una estrategia muy eficaz para los pacientes con fijación vertebral que desarrollan IPHQ.
The constant increase in spinal surgery with vertebral fixation, as well as the number and complexity of its indications, inevitably leads to a higher rate of complications. Of the complications that occur, infections are one of the most common and important types,1 not only because of their morbidity, but also because of the resulting major consumption in healthcare resources.2
The incidence of deep surgical wound infections (DSWI) in spinal surgery with implantation varies from 0.7% to 16%.2,3 This wide-ranging variability is associated with several factors, and these without doubt include the heterogeneous criteria used to define DSWI, factors that depend on patient comorbidities2,4,5 and others connected with the surgical procedure itself such as the duration of the operation, the amount of intra- and perioperative bleeding, a history of spinal surgery, the number of levels fixed and the type of procedure used.4,5
Although it is generally accepted that antibiotic therapy and wound debridement-washing are the fundamental treatments for DSWI, there is no agreement on the imperative need to remove implants and bone grafts6 to guarantee cure of the infection and prevent secondary problems with stability.6–8
The aim of this study is to describe our experience in the treatment of DSWI in patients treated by spinal instrumentation arthrodesis, using a strategy based on the broad debridement of the surgical wound and prolonged administration of antibiotic treatment, while keeping the instrumentation and replacing bone grafts.
Material and methodsStudy design, scope and populationThis observational retrospective study includes all of the patients who received spinal surgery with vertebral fixation during the period from 1 January 2010 to 31 December 2014, in the Trauma and Orthopaedic Surgery Department of our third level university hospital, which has a catchment area of 1,250,000 inhabitants.
Exclusion criteria and definitionsPatients aged less than 14 years old were excluded from the study. The diagnosis of DSWI was made using the criteria of the Centres for Disease Control and Prevention's National Healthcare Safety Network (CDC/NHSN).9 A patient was considered to have DSWI when they had the following criteria: clear signs of inflammation in the surgical wound, dehiscence or fistulisation, and signs of infection or suppuration during debridement that go beyond the muscle fascia and are in contact with implant material. DSWI was considered to be early onset when the symptoms or signs leading to diagnosis arose before one month after the operation, and late onset when they occurred after more than one month after the operation.
Procedures and preoperative prophylaxisAll of the initial surgical procedures took place under general anaesthetic with antibiotic prophylaxis administered 30min beforehand, consisting of a 2g perfusion of cefazolin, followed by 1g IV/8h during the following 24h. All of the patients were operated using a posterior approach and conventional surgical technique. An allograft was used for the arthrodesis except for occasional usage of iliac crest autograft. After the diagnosis of DSWI, drainage and broad debridement of all necrotic or devitalised tissue were performed as soon as possible, together with abundant washing and the removal of bone grafts, while always keeping vertebral instrumentation. In all cases, and depending on intraoperative findings, 3–5 deep representative samples were taken for culture. They were processed using normal microbiological techniques for the detection of aerobic or anaerobic flora.
Antimicrobial treatment and monitoringAfter drainage and debridement and sample-taking for culture the patients were initially treated empirically, followed by planned treatment until they had completed 8 weeks of treatment. Once treatment was completed the patients were followed-up for a period of 12 months.
Data recordingThe following variables were recorded: age, sex, reason for initial surgery, postoperative delay to the onset of symptoms, comorbidities, Charlson index, segment involved, number of vertebra fixed, duration of surgery and the need for transfusion. Records also included a complete haemogram, serum levels of creatinin, albumin and PCR, the results of cultures and prognosis, cure, failure or relapse.
Statistical processingData were entered in a suitable database and processed using version 23 of the SPSS software package (SPSS Inc., Chicago, IL, USA). Qualitative variables were expressed in percentages and quantitative variables were expressed as an average together with standard deviation (SD) or the mean and interquartile range (IQR), depending on the case in question. Quantitative variable distribution normalcy was studied using the Shapiro–Wilk test. The tests used to compare variables were the chi-squared test for qualitative variables and the Student t-test and Mann–Whitney U test for quantitative variables. A P value ≤.05 was considered significant.
ResultsThirty-two of the 799 patients included in the study were diagnosed with DSWI, so that the DSWI infection rate in our study amounted to 4%. 3 of these 32 patients (9.4%) did not complete follow-up and they were therefore excluded from the final analysis. The final sample was therefore composed of 29 patients. There were 15 women (51.7%) and 14 men (48.3%), with a mean age of 54.9 years old (IQR: 45.7–67 years old).
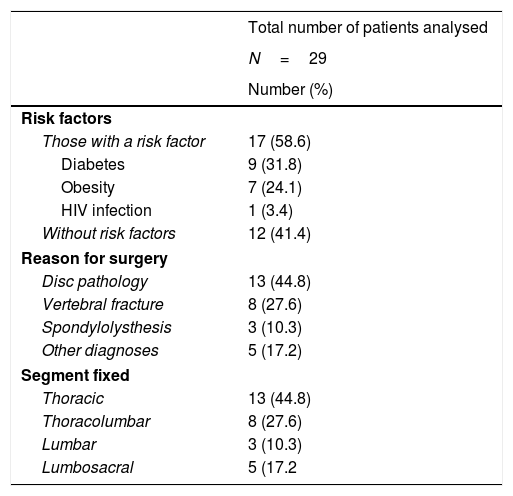
The DSWI was early onset in 26 cases (89.6%) and late onset in the remaining 3 (10.4%). The mean time period from surgery until diagnosis of DSWI was 19 days (IQR: 12–37). Table 1 shows he most relevant data respecting the diagnosis due to which arthrodesis was indicated, the spinal segments operated and patient comorbidities. It should be pointed out here that Charlson's comorbidity index mean value was 2 (IQR: 0–3).
Basal data of patients with DSWI.
| Total number of patients analysed | |
|---|---|
| N=29 | |
| Number (%) | |
| Risk factors | |
| Those with a risk factor | 17 (58.6) |
| Diabetes | 9 (31.8) |
| Obesity | 7 (24.1) |
| HIV infection | 1 (3.4) |
| Without risk factors | 12 (41.4) |
| Reason for surgery | |
| Disc pathology | 13 (44.8) |
| Vertebral fracture | 8 (27.6) |
| Spondylolysthesis | 3 (10.3) |
| Other diagnoses | 5 (17.2) |
| Segment fixed | |
| Thoracic | 13 (44.8) |
| Thoracolumbar | 8 (27.6) |
| Lumbar | 3 (10.3) |
| Lumbosacral | 5 (17.2 |
An average number of 4 vertebral bodies were treated by fixation (range 2–14). In 5 cases 2 vertebral bodies were fixed (17.24%), 3 were fixed in 15 cases (51.72%), 4 were fixed in 4 cases (13.79%) and more than 4 vertebrae were fixed in the 5 remaining cases (17.24%). The average duration of surgery was 145.77min (SD 59.64).
At the moment of diagnosis 14 patients (48.2%) had leukocytosis; nevertheless, 27 of the 29 patients (93.1%) had raised levels of PCR, with a mean value of 64.9mg/L (IQR: 16–109mg/L). Only 2 patients had normal serum PCR levels (≤3mg/L). Their cultures were negative in both cases, although they had inflammatory macroscopic data that strongly suggested infection.
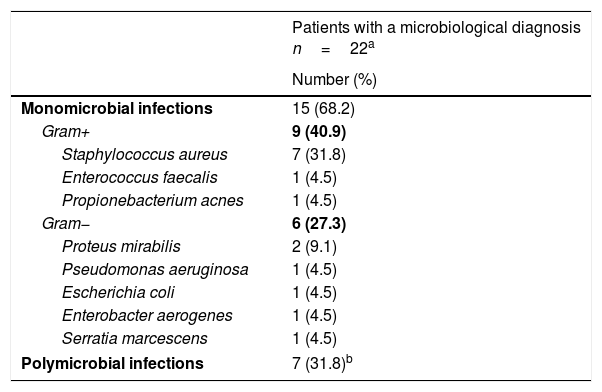
The cultures were positive in 22 cases (75.8%). The flora was monomicrobial in 15 of these 22 cases (68.2%) with a positive culture, while in the remaining 7 it was polymicrobial. The most frequent causal agent was Staphylococcus aureus, and this was isolated in 7 of the 29 patients with DSWI (24.1%), always alone. In 6 of the 7 patients with polymicrobial infections (85.7%) the cultures contained anaerobic microorganisms, while in the 3 in which Bacteroides spp. was isolated the lumbosacral segment had been operated. Table 2 shows the most relevant microbiological findings.
Microbiological findings.
| Patients with a microbiological diagnosis n=22a | |
|---|---|
| Number (%) | |
| Monomicrobial infections | 15 (68.2) |
| Gram+ | 9 (40.9) |
| Staphylococcus aureus | 7 (31.8) |
| Enterococcus faecalis | 1 (4.5) |
| Propionebacterium acnes | 1 (4.5) |
| Gram− | 6 (27.3) |
| Proteus mirabilis | 2 (9.1) |
| Pseudomonas aeruginosa | 1 (4.5) |
| Escherichia coli | 1 (4.5) |
| Enterobacter aerogenes | 1 (4.5) |
| Serratia marcescens | 1 (4.5) |
| Polymicrobial infections | 7 (31.8)b |
Due to the microbiological diagnosis the treatment was specific in 22 patients (75.8%) and completely empirical in the remaining 7 (24.2%). The planned 8-week treatment was completed in 25 patients (86.2%). Treatment was suspended in 2 patients (6.8%) after 4 weeks because of severe side effects, while treatment failed in one case, clinical and biological progress was highly positive in the second. Treatment in the remaining 2 cases had to be prolonged until week 12, as although the response was slow it was eventually positive.
Of the 25 patients treated during the planned 8 weeks, 24 (96%) had a favourable prognosis and one patient with S. aureus infection relapsed 9 months after the end of treatment: it was necessary to remove all of the fixation material and undertake a new cycle of treatment.
DiscussionThe development of a DSWI in an operated patient with vertebral fixations is a severe complication that seriously compromises the success of the previous surgery due to several reasons. Firstly, the proximity or even contact of the infection with osteosynthesis material not only hinders consolidation but also opens a route through which the infection may enter the bone, which would create the possibility of progression to post-surgical vertebral osteomyelitis. Secondly, infection of the still unabsorbed graft favours the development of a bone sequestrum that hinders treatment of the infection. Thirdly, and as a result of the first 2 possibilities, the main aim, i.e., the stability of the fixed segment of the spine, will be severely compromised.
Due to the above reasons, in our study we describe our experience with a therapeutic strategy that by debridement and the withdrawal of unabsorbed graft prevents the formation of a sequestrum, and which by prolonged antimicrobial treatment protects bone tissue with absorbed graft against the development of vertebral osteomyelitis, all without compromising the stability of the fixed segment.
A 4% rate of DSWI such as that found in our study is in line with the rates reported by other authors,2,3 and it strongly expresses the importance of energetic treatment in this type of increasingly frequent surgery.
The comorbidities of our DSWI patients and their levels of albumin do not differ substantially from those reported in other large series in the literature.2–5,10–12 Nevertheless, it should be pointed out that, unlike our study, the majority of the others did not measure Charlson comorbidity index, which is a highly reliable and standardised overall parameter for evaluating the frailty and life expectancy of patients.
It is a well-known fact that the serum PCR level is a highly sensitive inflammation marker and an extremely useful parameter for monitoring postoperative evolution. This is because after rising immediately after surgery, it normalises from day 10 to day 15; this either does not occur or the level swiftly rises if there is an active infection.6 In our study the mean level of PCR values was 64.9mg/L, which is a similar figure to those reported in other studies.6,12 This is a far more sensitive parameter than the total number of leukocytes, which was not raised in half of our patients with DSWI. It should be underlined that, in 2 cases of DSWI PCR levels were normal. This fact, which may be surprising, has already been reported by other authors. Thus Collins et al.13 advise that when diagnosing DSWI, PCR levels should be interpreted in a clinical sense, as they may often be normal in the presence of an active infection caused by pathogens with a low level of virulence. Both patients in our study with normal PCR levels had negative cultures together with the presence of unmistakeable signs of infection in debridement. It is possible that these cases were caused by pathogens which are hardly aggressive, such as Propionibacterium acnes, which live on the skin and habitually cause infection in patients with osteosynthesis material. It is sometimes difficult to isolate these pathogens as they require a prolonged incubation.
Respecting the microbiological findings of our study, 75.8% of the patients had positive cultures, 2/3 of them with monomicrobial infections and one third with polymicrobial infections. These rates are similar to others reported in the literature,6,14 as is the fact that the microorganism isolated the most often was S. aureus15 followed by the GNB, and that the polymicrobial infections by enteric flora were most frequent in the patients operated in the lumbosacral segment. Nor should it be forgotten that some flora required special sample processing to be isolated, and the main cause of negative cultures is still the widespread practice of administering antimicrobial treatment to patients before debridement and sample taking for culture.
If we assume that, as occurred in our study, more than 90% of the patients who had a DSWI after vertebral fixation surgery will be diagnosed in the first month after the operation, during which implant removal is not indicated,7,15 the strategy used in our study is shown to be especially positive, as it achieves a cure in 96% of the patients treated with surgical debridement of the wound and replacement of the bone graft while keeping the instrumentation, with 8 weeks of antibiotic therapy. These results are similar to those achieve with withdrawal of the fixation, and with the additional advantage that spinal stability is maintained.13–16
This study has a series of limitations that should be taken into account when evaluating its results. Firstly, the fact that it is retrospective prevents rigorous analysis of the risk factors associated with suffering a DSWI. On the other hand, the limited size of its sample makes it impossible to relate the results of the suggested strategy with the different epidemiological variables, the segment involved or the causal microorganism. Thirdly, the follow-up period of one year may not be sufficient to rule out late relapses. Lastly, it may be impossible to extrapolate the external validity of our results to patient cohorts with a higher rate of comorbidities, or to hospitals with less experience in spinal surgery with vertebral fixation or those which do not have a permanent expert consultant in infectious diseases. To conclude, in spite of these limitations the robustness of our results could justify trialling this therapeutic strategy in broader multicentre studies.
Level of evidenceLevel of evidence III.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Gómez Cáceres A, Lucena Jiménez JS, Reyes Martín ÁL, Moriel Durán J, Sobrino Diaz B, García de Quevedo Puerta D. Pronóstico de la infección profunda en la cirugía raquídea con implante, tratada mediante retención, retirada del injerto óseo y antibioterapia prolongada. Rev Esp Cir Ortop Traumatol. 2019;63:7–11.