To assess the clinical validity of two new recently described parameters (spinal-sacral angle (SSA) and spinal inclination angle (SIA)) in adult scoliosis (AS) for evaluating the spinal-pelvic sagittal profile, as well as their still undefined role in AS.
Material and methodA non-concurrent prospective radiographic and clinical study was conducted on 59 primary surgeries of AS (Cobb>40°), with a minimum of 2 years follow-up. The available X-rays and health questionnaires of 49 patients were used in the study. The changes in X-ray parameters after surgery were evaluated (Wilcoxon test), as well as the correlations as regards the clinical-radiography-age parameters (Spearman test and multiple linear regression).
ResultsThe median post-surgical follow-up was 8.5 years, and the median age of the patients was 49.5 years. There was a statistically significant change with the surgery in the SSA and SIA (less than 5° in both), thoracic kyphosis, lumbar lordosis (LL), pelvic rotation, sagittal balance (SB) and frontal Cobb. There was no correlation between pain and SSA-ST. There was a significant relationship between activity and SSA, ST, LL, SB, and age. After the multivariate analysis only age (not SSA or SIA) remained as a possible predictor of lower activity.
DiscussionWhen frontal deformity predominates, the sagittal radiographic parameters, including the newest angles, although they have an influence patient activity when analysed individually, they lose this influence when they are analysed together and with other clinical parameters.
ConclusionsThe SSA and SIA hardly change with surgery. They only correlate with activity, but cannot be considered predictors of this. Thus they do seem to be useful measurements in AS.
Evaluar la validez clínica en EA de 2 nuevos parámetros (ASS y ST) descritos recientemente para la evaluación del perfil sagital espinopélvicos, y cuyo papel en EA no está aún definido.
Material y métodoAnálisis prospectivo (no concurrente) radiográfico y clínico de 59 cirugías primarias de EA (Cobb>40°), mínimo 2 años de seguimiento. Para este trabajo dispusimos de radiografías y cuestionarios de salud de 49 pacientes. Se evaluó el cambio de los parámetros radiográficos tras cirugía (test Wilcoxon) y la correlación resultados clínicos-radiográficos-edad (test de Spearman y regresión lineal múltiple).
ResultadosMediana de seguimiento postoperatorio 8,5 años. Mediana edad 49,5 años. Hubo cambio estadísticamente significativo con la cirugía en ASS y ST (en ambos inferior a 5°), cifosis torácica (CT), lordosis lumbar (LL), rotación pélvica (RP), balance sagital (BS) y Cobb frontal. No hubo correlación entre dolor y ASS-ST. Hubo correlación significativa entre actividad y ASS, ST, LL, BS) y edad. Tras análisis multivariante solo la edad (ni ASS ni ST) persistió como posible predictor de menor actividad.
DiscusiónCuando predomina la deformidad frontal, los parámetros radiográficos sagitales, incluidos los más novedosos ángulos, si bien sí influyen en la actividad del paciente cuando se analizan de forma aislada, pierden esta influencia cuando se analizan en conjunto y junto a otros parámetros clínicos.
ConclusionesLos valores de SSA y ST varían escasamente con la cirugía. Solo se correlacionan con la actividad pero no pueden considerarse predictores de la misma. No parecen pues medidas de utilidad en EA.
The role of spinal alignment in the sagittal plane is increasingly gaining importance in pathologies of the vertebral spine, as in the case of adult deformities.1–5 Different studies have highlighted the correlation between clinical results and the value of the sagittal vertical axis or sagittal balance (SB),3 lumbar lordosis (LL)4 and pelvic parameters (pelvic rotation).5
However, at present there is no exact definition of adequate sagittal balance and each new day brings new concepts and radiographic measurements to be used in everyday clinical practice. In this respect, 2 new sagittal parameters have been recently described6,7 whose role in the treatment of adult scoliosis (AS) has not yet been determined. These 2 parameters are the spinal-sacral angle (SSA) and the spinal inclination or tilt angle (SIA or ST).
The aim of this review is to evaluate the clinical validity of the SSA and ST: to study how they vary with surgery and their correlation with clinical outcomes.
Material and methodsThe study was designed as an analysis (nonconcurrent and prospective) of a series of consecutive patients who met the following inclusion criteria:undergoing operation for idiopathic or degenerative scoliosis; primary surgery taking place after the age of 21 years; patients presenting a deformity of over 40° in the coronal plane; at least 4 levels (5 vertebrae) fused using segmental instrumentation; minimum postoperative follow-up period of 2 years; and all patients agreeing to an update of the studies on their current clinical and radiographic condition. We included a total of 59 patients, of which we used 49 in the present review (10 patients were excluded due to preoperative radiographs of inadequate quality to measure angles).
During the study period, medical records were updated through a clinical interview with patients:they completed the SRS228,9 and SF3610,11 tests and pain was assessed through a visual analogue scale (VAS) which reflected the intensity of pain indicated by patients on a subjective scale from 0 to 10, with 0 representing no pain and 10 representing the worst pain imaginable.12
We analysed the preoperative and final follow-up radiographs in the anteroposterior and lateral projections (including spine and pelvis) whilst standing (with hands resting on clavicles and shoulders at 45° anterior elevation).13 The radiographic study was updated when necessary. At our centre, clinical and radiographic reviews of adult patients intervened for scoliosis are obtained at 2, 6 and 12 months postoperatively, then annually until the fifth year and biannually thereafter. Therefore, those subjects who had been operated more than 5 years earlier, from whom an X-ray had been obtained in the past 24 months and with no clinically significant changes did not undergo a new radiographic study in order to avoid unnecessary radiation. Thus, no radiographic studies were conducted without a clinical indication.
We measured the SSA and ST values6,7 (Fig. 1), in addition to the radiographic parameters normally used14 to evaluate sagittal balance: thoracic kyphosis (TK), lumbar lordosis (LL), sagittal vertical axis (SB) and sagittal pelvic parameters (pelvic incidence, pelvic rotation and tilt of the sacrum). We also collected the frontal Cobb value and age of each patient at the time of responding to the clinical tests. All were continuous variables.
Spinal tilt (a) and spinal-sacral angle (b). A line is traced from the centre of the C7 vertebra to the centre of the sacral plate. The angle formed by this line with the sacral plate is the SSA, whilst the angle formed with the horizontal is the ST. They represent the position of C7 with respect to what should be the support base of the spine (pelvis).
We used the Wilcoxon nonparametric test for related measurements to evaluate the evolution of the continuous variables between the postoperative and final values. We used the Spearman correlation coefficient to evaluate the linear association between continuous variables. We also conducted multiple linear regression analysis to jointly assess the effect of statistically significant variables in the univariate analysis.
ResultsWe reviewed 49 patients (42 females and 7 males). The median postoperative follow-up period was 8.5 years (range: 4–12.6 years). The median age at follow-up was 49.5 years (range: 37.7–60 years). The aetiology was idiopathic in 39 cases and degenerative in 10 cases. The median preoperative value of the main curve Cobb was 58° (range: 44–75°) and the final value was 29° (range: 18–37°), thus showing a significant improvement with surgery (p<0.000).
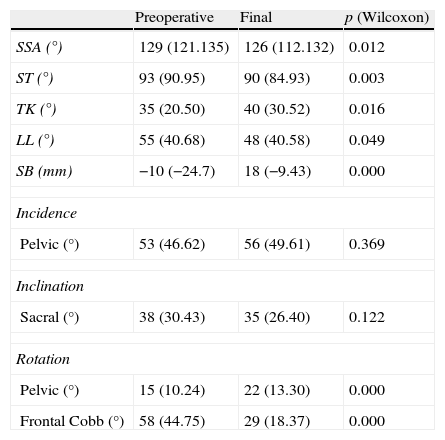
There was a statistically significant change with surgery in SSA values (p=0.012) and ST values (p=0.003). However, we believe that it holds no clinical significance, since the variation did not even reach 5°. The rest of the parameters evaluated also varied significantly with surgery, except for pelvic incidence and sacral tilt (Table 1).
Variation of the radiographic parameters in the final postoperative period.
| Preoperative | Final | p (Wilcoxon) | |
| SSA (°) | 129 (121.135) | 126 (112.132) | 0.012 |
| ST (°) | 93 (90.95) | 90 (84.93) | 0.003 |
| TK (°) | 35 (20.50) | 40 (30.52) | 0.016 |
| LL (°) | 55 (40.68) | 48 (40.58) | 0.049 |
| SB (mm) | −10 (−24.7) | 18 (−9.43) | 0.000 |
| Incidence | |||
| Pelvic (°) | 53 (46.62) | 56 (49.61) | 0.369 |
| Inclination | |||
| Sacral (°) | 38 (30.43) | 35 (26.40) | 0.122 |
| Rotation | |||
| Pelvic (°) | 15 (10.24) | 22 (13.30) | 0.000 |
| Frontal Cobb (°) | 58 (44.75) | 29 (18.37) | 0.000 |
Median (25 percentile and 75 percentile); p: statistical significance; LL: lumbar lordosis; SB: sagittal balance; SSA: spinal-sacral angle; ST: spinal tilt; TK: thoracic kyphosis.
There was a significant improvement in pain (p<0.00). The preoperative VAS value was 7 (3.8) and the final was 3.5 (1.5). There was no correlation between pain scores and the SSA and ST angles in the preoperative period or at the end of evolution.
The results of the quality of life tests at the end of the follow-up period are shown in Table 2.
Quality of life tests (median, 25–75 percentiles).
| Median | 25 percentile | 75 percentile | |
| SRS function | 3.4 | 2.8 | 4.1 |
| SRS pain | 3.2 | 2.2 | 4.2 |
| SRS self image | 3.5 | 3.0 | 4.0 |
| SRS mental health | 3.6 | 3.0 | 4.0 |
| SRS satisfaction | 4.0 | 3.5 | 4.8 |
| SRS total | 3.6 | 2.9 | 4.0 |
| SF36 physical function | 60.0 | 35.0 | 75.0 |
| SF36 physical role | 50 | 0 | 100 |
| SF36 pain | 51.0 | 22.0 | 72.0 |
| SF36 general health | 47.0 | 35.0 | 74.5 |
| SF-36 vitality | 45.0 | 30.0 | 62.5 |
| SF36 social function | 75.0 | 50.0 | 87.5 |
| SF36 emotional role | 100 | 0 | 100 |
| SF36 mental health | 64.0 | 52.0 | 75.0 |
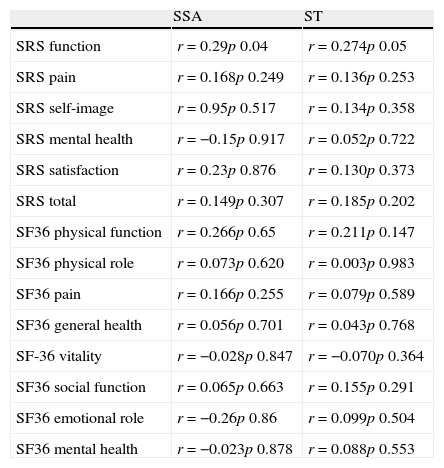
There was a significant correlation in the final follow-up between the SRS activity subscale and SSA (p=0.04; r=0.29) and ST (p=0.05; r=0.27). No other SRS22 nor SF36 subscale correlated with SSA or ST values (Table 3).
Correlation between quality of life tests and SSA/ST.
| SSA | ST | |
| SRS function | r=0.29p 0.04 | r=0.274p 0.05 |
| SRS pain | r=0.168p 0.249 | r=0.136p 0.253 |
| SRS self-image | r=0.95p 0.517 | r=0.134p 0.358 |
| SRS mental health | r=−0.15p 0.917 | r=0.052p 0.722 |
| SRS satisfaction | r=0.23p 0.876 | r=0.130p 0.373 |
| SRS total | r=0.149p 0.307 | r=0.185p 0.202 |
| SF36 physical function | r=0.266p 0.65 | r=0.211p 0.147 |
| SF36 physical role | r=0.073p 0.620 | r=0.003p 0.983 |
| SF36 pain | r=0.166p 0.255 | r=0.079p 0.589 |
| SF36 general health | r=0.056p 0.701 | r=0.043p 0.768 |
| SF-36 vitality | r=−0.028p 0.847 | r=−0.070p 0.364 |
| SF36 social function | r=0.065p 0.663 | r=0.155p 0.291 |
| SF36 emotional role | r=−0.26p 0.86 | r=0.099p 0.504 |
| SF36 mental health | r=−0.023p 0.878 | r=0.088p 0.553 |
R: correlation coefficient; p: statistical significance; SSA: spinal-sacral angle; ST: spinal tilt.
We also found a correlation between the SRS activity subscale and the following final parameters: lumbar lordosis, sagittal balance, pelvic rotation (Table 4) and age (p=0.001; r=−0.46).
Correlation of SRS activity with sagittal radiographic parameters.
| Thoracic kyphosis | Lumbar lordosis | Sagittal balance | Pelvic incidence | Pelvic rotation | Sacral tilt | |
| SRS 22 activity | r=−0.024p 0.871 | r=0.316p 0.029 | r=−0.430p 0.002 | r=−0.281p 0.05 | r=−0.467p 0.001 | r=0.254p 0.078 |
R: correlation coefficient; p: statistical significance.
Since a significant correlation was observed between the SRS activity scores and several of the variables analysed in the univariate analysis, we decided to conduct a multivariate analysis. We performed multiple linear regression, including the final SRS22 activity score as dependent variable and patient age, SSA, ST, SB and pelvic rotation as independent variables in the maximum model. In the final model, only patient age remained as a possible predictor of activity (0.026). The adjusted r2 was equal to 0.165 (16.5% of the total variability observed in SRS22 activity would be due to age; p=0.002).
DiscussionThe search for correlations between radiographic measurements and clinical tests is a constant in current clinical practice.1–5 The goal is to associate objective radiographic measurements with subjective clinical results in order to determine which “radiographic figures” we must achieve through surgery to ensure a satisfactory clinical outcome.
The literature indicates that sagittal, rather than frontal, radiographic parameters correlate with clinical outcomes,1,3–5 but paradoxically there is no clear definition of what a “normal” sagittal balance is. A wide range of values are considered normal and there is no complete agreement on which are the best radiographic parameters to use.15,16 The French school has recently described 2 new angles (SSA and ST) and suggested their use as the best way to assess overall, spinal-pelvic sagittal balance.6,7,17 We have not found any works which have evaluated the variation of these angles with scoliosis surgery in adulthood or, more importantly, which have correlated them with clinical condition (pain, quality of life test results). Following a line of work18–22 started at our centre some years earlier in order to analyse the surgical treatment of scoliosis in adulthood, and given the importance which the literature1–5 confers to the sagittal plane in this pathology, we decided to analyse the relationship of the SSA and ST parameters with scoliosis surgery in adults.
At this point we should mention that the clinical and radiographic results obtained in our patients were similar to those found in the literature for adult deformity surgery,23–26 including variations occurring in TK, LL, SB, and pelvic parameters.23,26–28 We have not found any publications with which to compare changes in SSA and ST. Our results indicate that changes in SSA and ST are not clinically significant (<5°), probably because precisely in scoliosis the values of sagittal measurements in older populations do not hold as much importance as has been indicated in recent years.22,29
As for the correlation of these angles with symptoms, we did not observe a correlation with pain at any time during the evolution. The only significant correlation was with patient activity, but this significance was low, the correlation coefficient was very small and the correlation was lost when analysed in conjunction with other variables. In short, it was not clinically relevant.
Of course, it would be desirable to have a higher number of patients, since the size of the sample limits the power of the study.
However, we had a group of patients with homogeneous diagnoses, long follow-up periods and updated clinical and radiographic studies. Moreover, we analysed the role of the SSA and ST using multivariate analysis for the first time, which had not been done in most published correlation studies.
With the specified limitations and based on our results, we can indicate that the SSA and ST angles do not seem clinically useful measurements in AS.
Level of evidenceLevel of evidence III.
Ethical responsibilitiesProtection of people and animals. The authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of data. The authors declare that they have followed the protocols of their workplace on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consent. The authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Gómez-Rice A, et al. Correlación de resultados clínicos y perfil sagital en escoliosis del adulto. Valor del ángulo espinosacro y del ángulo de inclinación del raquis. Rev Esp Cir Ortop Traumatol. 2012;56:426–31.