Remote cerebellar haemorrhage is a rare but serious complication after spinal surgery. Although the mechanism is not well known, it always occurs after loss of cerebrospinal fluid due to dural tear, not always identified, which produces remote venous bleeding. Prognosis depends largely on the severity of this bleeding.
We report a case of 67-year-old female who suffered a cerebellar and subarachnoid haemorrhage and subdural haematoma after elective lumbar fusion surgery and eventually required decompressive craniectomy.
La hemorragia cerebelosa (HC) distal es una complicación infrecuente pero grave tras cirugía espinal. Aunque el mecanismo de aparición sigue siendo desconocido, sucede tras la pérdida de líquido cefalorraquídeo (LCR) por desgarro dural, no siempre objetivado, lo que produce un sangrado venoso a distancia. El pronóstico depende en gran medida de la gravedad de dicha hemorragia.
Se presenta el caso de una mujer de 67 años que sufrió, además de HC, hemorragia subaracnoidea (HSA) y hematoma subdural (HS) tras artrodesis lumbar programada que requirió craniectomía descompresiva.
Several publications on remote cerebellar haemorrhage (CH) after spinal surgery have appeared since Chadduck reported this complication for the first time in 1981, with a mechanism that is still unknown. It is thought that intracranial hypotension due to intraoperative loss of the cerebrospinal fluid (CSF) following a detected fistula would lead to transitory venous occlusion followed by transformation into haemorrhage. This should be suspected in case of intense cephalea or unexplained neurological deterioration after the operation, with the finding in a computed tomography scan (CT) of a “zebra pattern” CH.
This describes the case of remote CH following spinal surgery, without the detection of an intraoperative fistula, that required decompressive hemicraniectomy. The early clinical suspicion and medical–surgical treatment of the complications were fundamental in minimising neurological sequelae.
Clinical caseA 67 year-old woman was operated, in programmed surgery, for L4–L5 lumbar arthrodesis. The surgery, in prone decubitus, took place without apparent dural opening or other anaesthetic-surgical incidents.
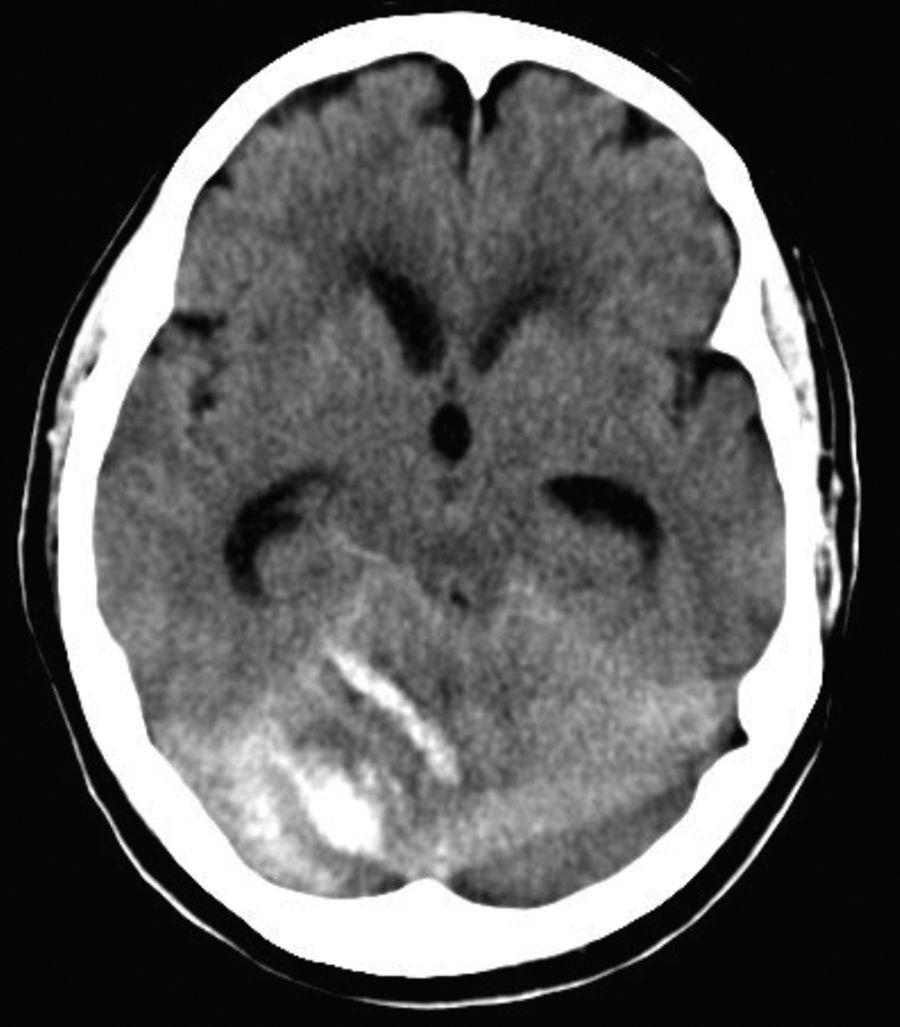
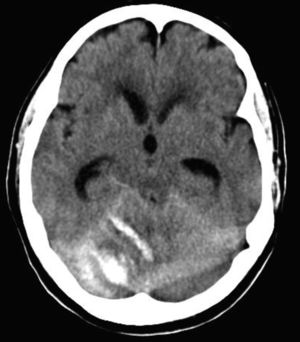
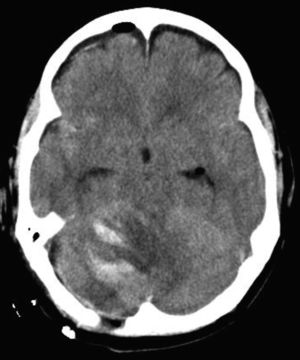
15h after surgery and in the hospitalisation ward the patient suffered sudden cephalea and progressive neurological deterioration. Cerebral CT (Fig. 1) showed one 17ml CH in the upper right hemisphere and another of 1.5ml, obstructive hydrocephaly and incipient cerebral oedema, together with diffuse subarachnoid haemorrhage (SAH) and right occipital subdural haematoma (SH).
An emergency operation was performed with occipital craniotomy to drain the SH and position an external ventricular drainage with an intracranial pressure sensor. The patient was then admitted to the intensive care unit (ICU) for clinical stabilisation and neurological monitoring.
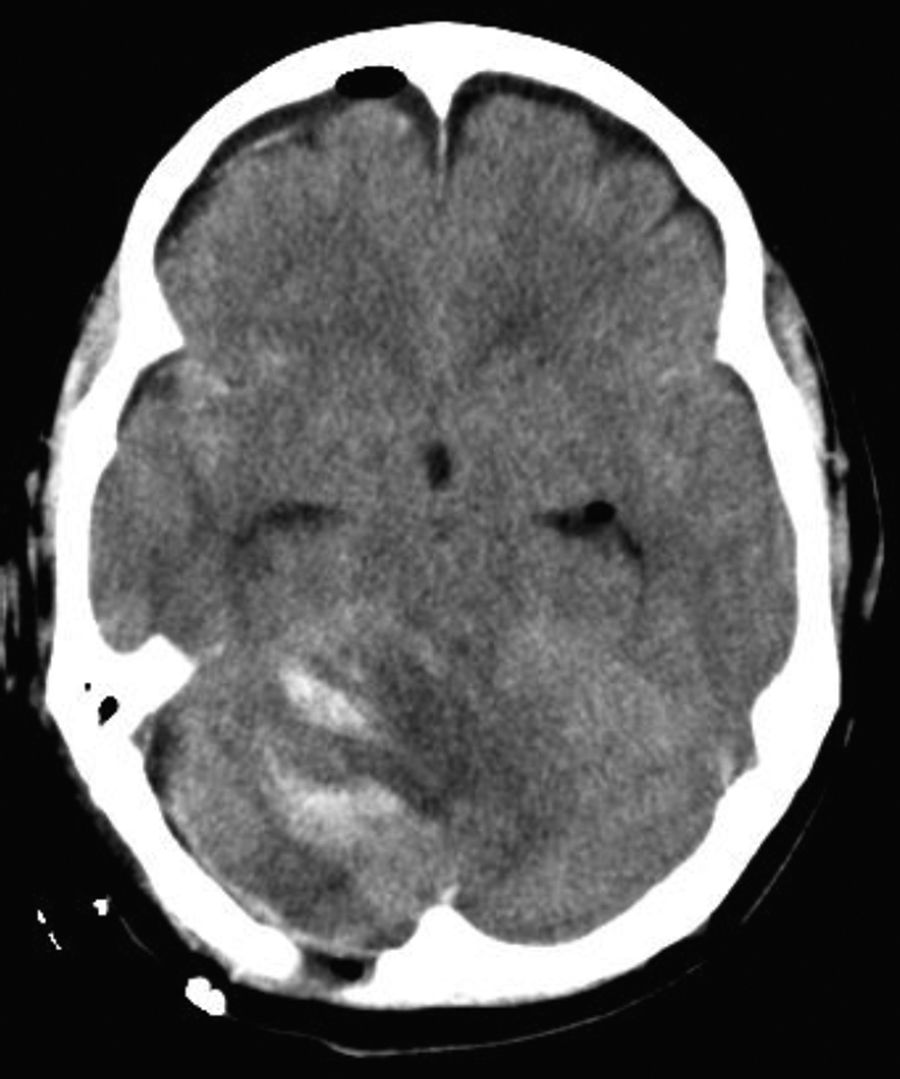
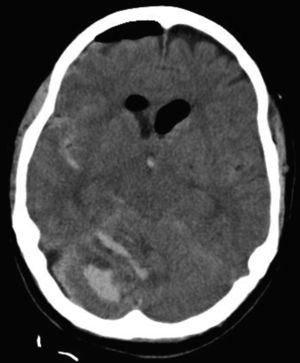
Twenty-four hours after the complication, as well as the haemorrhage and signs of brain stem compression, a new cerebral CT (Fig. 2) showed marked venous ingurgitation of the cervical venous sinuses and plexi. These findings supported the suspicion of craniospinal hypotension due to a dural fistula. All of this made urgent right occipital hemicraniectomy necessary (Fig. 3).
The progress of symptoms and radiological data initially led to the suspicion of accidental dural opening with the resulting internalised fistula. Given this clinical suspicion the decision was taken to treat the complications with conservative management of the supposed fistula, with lumbar repose and broad spectrum antibiotic therapy as prophylaxis against bacterial meningitis.
Forty days after admission to the ICU the patient was discharged to a hospitalisation ward to continue neuro-rehabilitation treatment. She had a good level of consciousness but also cerebellar ataxia and residual paresis of the lower limbs.
DiscussionChadduck reported the first case of remote CH in 19811 after a cervical laminectomy. This rare complication arose hours after the operation, and its mechanism of appearance is still unknown.1,2 The most widely accepted hypothesis is that of intracranial hypotension caused by the intraoperative loss of CSF due to a fistula, detected or hidden, that would cause the caudal displacement of the cerebellum and transitorily occluding the upper cerebellar veins by elongation, thereby causing an intraparenquimatose haemorrhaging venous infarct. The probability of this occurring is raised if the collateral veins are insufficient.1–5 In cases following spinal surgery no other causal factor has been described except for dural opening.3
Cerebral CT is the preferred diagnostic test. The finding of a haemorrhage in the cerebellar hemisphere with a “zebra” pattern (curved stripe-like areas with increased attenuation in the cerebellar folia) would lead to the suspicion of a CSF fistula.1,3–7 It should be pointed out that to date no description of SAH and SH with CH is found in the literature.
Initially and in the majority of cases a conservative attitude would be adopted, with rest for dural closure, close neurological monitoring and benign evolution, without sequelae or with slight neurological deficits, although in 10–12% of cases it will be mortal. The prognosis basically depends on the severity of the haemorrhage.1–3,5,7
ConclusionIt is of fundamental importance to prevent the loss of CSF and immediately repair the dura mater to avert CH after spinal surgery.1–5
CH must be suspected in case of intense cephalea or inexplicable neurological deterioration after the operation, even when no dural tear has been detected and a compatible CT confirms the CH. Early diagnosis, close monitoring and medical–surgical treatment of complications are all fundamental to minimise possible neurological sequelae.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed conform to the ethical norms of the responsible human experimentation committee, the World Medical Association and the Helsinki Declaration.
Confidentiality of dataThe authors declare that they followed the protocols of their centre of work regarding the publication of patient data.
Right to privacy and informed consentThe authors obtained the informed consent of the patients and/or subjects referred to in this paper. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
We would like to thank the Intensive Medicine, Neurosurgery and Radiology Departments of Miguel Servet University Hospital.
Please cite this article as: Val-Jordán E, Seral-Moral P, Novo-González B. Hemorragia cerebelosa distal por fístula dural oculta tras cirugía espinal. Rev Esp Cir Ortop Traumatol. 2018;62:228–230.