To evaluate the functional and subjective results of the Sauvé-Kapandji procedure as a treatment for distal radioulnar joint disorders.
Materials and methodsA retrospective study was conducted on 27 patients treated using the Sauvé-Kapandji technique from January 2001 to March 2012. The aetiología, age, sex, laterality, articular movement, radiographical signs of joint degeneration, and cubitus varus, were analyzed. The Mayo Clinic wrist assessment scale and the DASH questionnaire were used for the postoperative evaluation. The mean follow-up was 24 months (6–48 months). The mean age was 47.2 years, with 66.7% females, and 55% the dominant side.
ResultsAt one year after surgery, 16 cases had mild or no pain (59.2%), 8 cases with moderate (29.6%) and 3 cases with severe pain (11.1%). The pronation–supination went from a pre-operative average of 96.8° to 136.4° postoperative, operatorios, which was a significant statistical difference (Wilcoxon test). The radioulnar ratio went from a pre-operative average of +2.6mm to −0.39mm postoperative. Full functional recovery was observed in 48%. A grip strength of 50.6%, compared to the contralateral wrist was achieved.
ConclusionsThe Sauvé-Kapandji technique could avoid the complications common in other procedures, such as cubital-carpal migration. Our study agrees with that in the literature with good results as regards the range of joint movement, with an acceptable improvement in pain compared to the previous stage, but it also demonstrates the frequent loss of grip strength and instability of the proximal radio-ulnar joint.
Evaluar los resultados funcionales y subjetivos del procedimiento de Sauvé-Kapandji como tratamiento de los trastornos de la articulación radiocubital distal.
Material y métodoRealizamos un estudio retrospectivo de 27 pacientes sometidos a la técnica de Sauvé-Kapandji desde enero de 2001 a marzo de 2012. Analizamos la etiología, edad, sexo, lateralidad, balance articular, signos radiográficos de degeneración articular y varianza cubital. Para la evaluación postoperatoria se utilizó la escala de valoración de muñeca de la Clínica Mayo y el cuestionario DASH. El seguimiento medio fue de 24 meses (6–48 meses). La edad media fue de 47,2 años. El 66,7% fueron mujeres y el 55,5% lado dominante.
ResultadosAl año de la cirugía 16 casos presentaron dolor leve o ausente (59,2%), 8 casos moderado (29,6%) y 3 casos severo (11,1%). La pronosupinación pasó de un promedio preoperatorio de 96,8° a 136,4° postoperatorios, resultando esta diferencia estadísticamente significativa (prueba de Wilcoxon). La relación radiocubital pasó de un promedio preoperatorio de +2,6mm a −0,39mm postoperatorios. La recuperación laboral sin limitación fue posible en el 48%. Se consiguió una fuerza de prensión del 50,6% respecto a la muñeca contralateral.
ConclusionesLa técnica de Sauvé-Kapandji podría evitar complicaciones frecuentes de otros procedimientos como la migración carpiana cubital. Nuestro estudio coincide con la literatura en los buenos resultados respecto al rango articular con aceptable mejoría del dolor respecto al estado previo, pero también demuestra la frecuente pérdida de fuerza de prensión e inestabilidad del muñón cubital proximal.
The distal radioulnar joint is part of the complex forearm joint structure which acts as a pivot allowing pronosupination.1
A combination of rotation and translation movements occurs during forearm rotation in a trochoid diarthrodial joint surface, enabling displacement of the ulnar head on the sigmoid notch.2 Thus, the head of the ulna is located on the dorsal and distal region of the joint during pronation, and in the palmar and proximal region during supination.
Lesions at this level, whether traumatic or degenerative, are often difficult to diagnose.3 Symptomatic dysfunction of the distal radioulnar joint following a wrist injury is not infrequent, especially when associated with distal radius fractures,4 leading to the presence of pain in the ulnar region of the wrist, as well as a limitation of forearm rotation.5
There is still considerable controversy regarding the ideal method to address this problem.6,7 Multiple surgical techniques have been described aimed at treating this disease in cases where previous conservative treatment has been ineffective. One of the most common procedures involves resection of the distal part of the ulna (Darrach technique1 and modifications8), but there are still multiple doubts surrounding the effectiveness of this technique due to its possible sequelae, which include frequent ulnocarpal instability and grip weakness.6 Other surgical options range from malunion in the distal ulna as described by Baldwin4 in 1921 or hemiresection-interposition arthroplasty as described by Bowers,9 to distal radioulnar arthroplasty and hemiarthroplasty techniques which are used in extreme cases.
At present, a valid alternative for distal radioulnar degeneration in patients with high functional wrist demands,10 particularly in those with post-traumatic etiologies, is that described by Sauvé and Kapandji11 in 1936. This was subsequently modified by several authors, such as Kapandji12 in 1986. This technique consists of the fusion of the distal radioulnar joint, along with the creation of a pseudoarthrosis (or nonunion) in the distal ulna, proximal to the arthrodesis (or fusion) zone.
The aim of our study was to evaluate the functional and subjective results of the Sauvé-Kapandji procedure used for the treatment of disorders in the distal radioulnar joint which showed no improvement in spite of conservative treatment.
Materials and methodsWe conducted a retrospective analysis of 27 patients who were intervened using the Sauvé-Kapandji technique at our hospital between January 2001 and March 2012. The mean postoperative follow-up period was 24 months (range: 6–48 months). The mean age was 47.2 years (range: 25–71 years). There were 9 male patients (33.3%) and 18 female patients (66.7%). Of the total cases, 15 involved the dominant wrist (55.55%) and 12 the non-dominant (44.45%).
These patients suffered pain in the distal radioulnar joint and limitation of forearm supination caused by degenerative disease (6 cases), rheumatoid arthritis (1 case), painful sequelae following fracture of the distal radius (17 cases), instability at the level of the distal radioulnar joint (2 cases) and anatomical abnormalities at that level (1 case of distal radioulnar synostosis).
Patients were considered candidates for the Sauvé-Kapandji technique when they presented chronic pain located in the distal radioulnar joint together with radiographic signs of joint degeneration, associated or not to limitation of the forearm supination arc or instability at the level of the distal radioulnar joint.
The treatment was applied after explaining to patients the risks and benefits of the technique and after obtaining their approval and a signed informed consent form. All procedures were performed by the same surgical team.
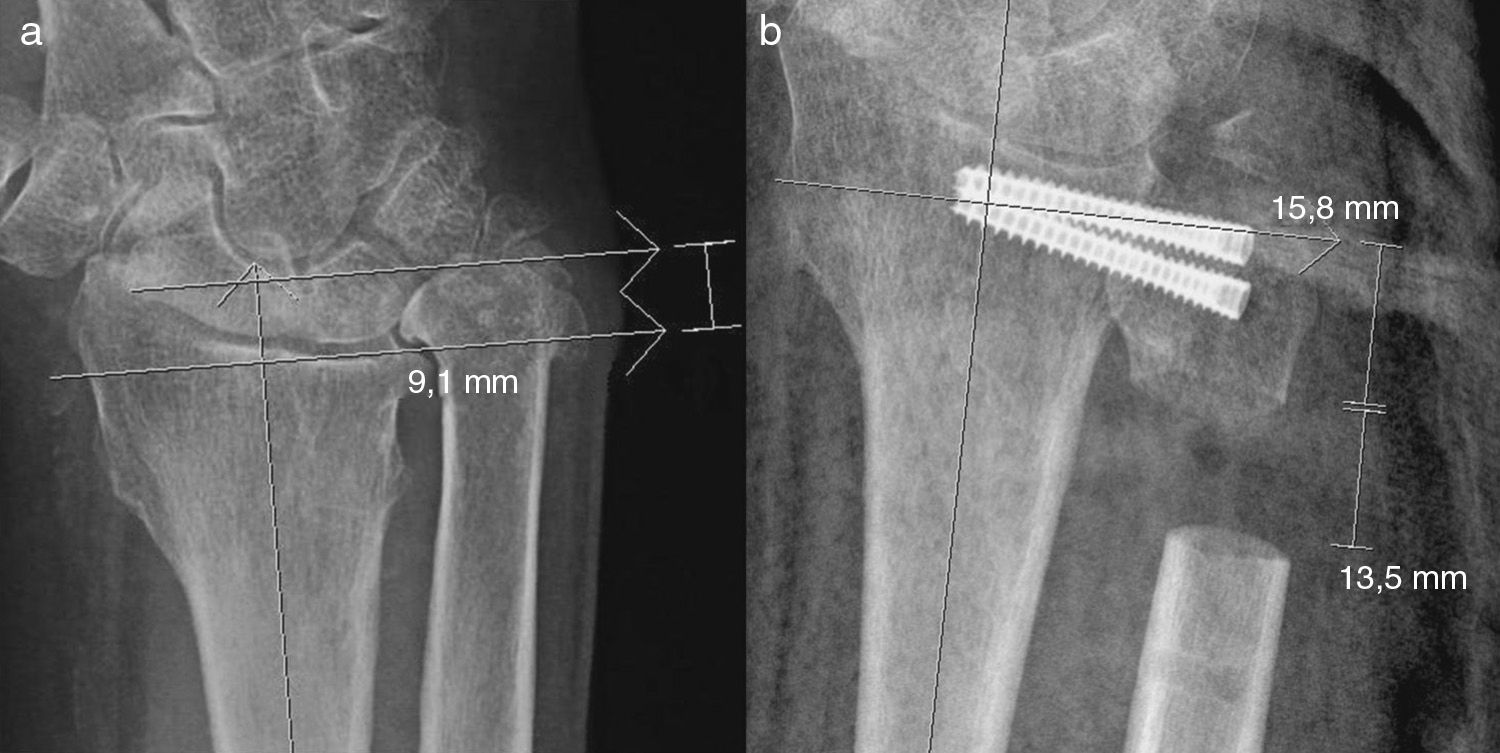
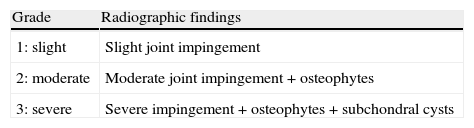
The preoperative radiological study for the assessment of joint degeneration of the distal radioulnar joint was based on the radiographic criteria described by Knirk and Jupiter13 (Table 1), and it enabled the measurement of the preoperative radioulnar ratio (Fig. 1a). The postoperative radiographic study enabled assessment of the consolidation of the arthrodesis, variation of the radioulnar ratio, appearance of ossifications and degenerative changes at the level of the distal radioulnar joint.
Radiographic assessment criteria for the distal radioulnar joint.
| Grade | Radiographic findings |
| 1: slight | Slight joint impingement |
| 2: moderate | Moderate joint impingement+osteophytes |
| 3: severe | Severe impingement+osteophytes+subchondral cysts |
The measurement of dorsal flexion, palmar flexion, radial tilt, ulnar tilt and pronosupination in the preoperative period and at the time of the assessment was carried out with a manual goniometer.
The postoperative evaluation of the results was conducted using objective and subjective criteria for the clinical assessment of pain, functional capacity, joint balance and grip strength, as well as the use of the ‘Disabilities of the Arm, Shoulder and Hand’ (DASH) scale, which measures the perception by patients of inability to perform certain activities due to pain, stiffness and muscle weakness.14 Postoperative pain was classified as absent, mild, moderate or severe according to the need for analgesic medication and its interference with activities of daily living (Table 2).
Clinical criteria for postoperative pain staging.
| No pain | Absence of pain |
| Mild | No limitation for activities of daily living.Requires medication occasionally. |
| Moderate | Some limitation for activities of daily living.Requires continuous medication. |
| Severe | Disabling for activities of daily living.Requires new surgical intervention. |
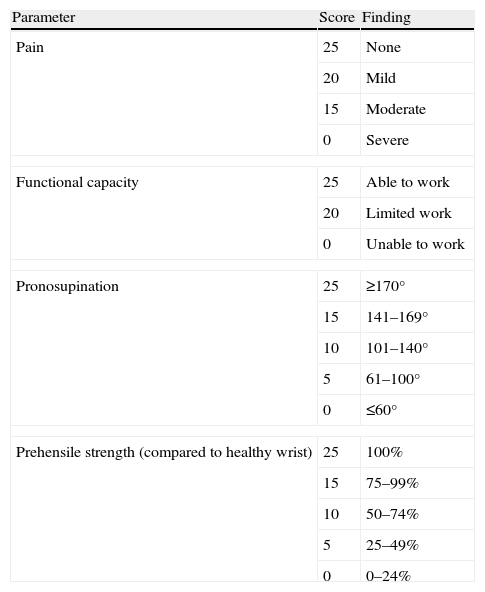
We used the Mayo Clinic ‘Modified Wrist-Scoring System’ for the objective assessment of results. This scale measures residual postoperative pain, the ability to return to previous daily activities, the pronosupination arc and grip strength compared to the healthy, contralateral wrist (measured using a Jamar®-type dynamometer). A final score between 90 and 100 points was considered as an excellent result, between 80 and 89 points a good result, between 65 and 79 points a moderate result and a score below 65 points was considered as a poor result (Table 3).
Mayo Clinic wrist assessment scale (Modified: Wrist-Scoring System).
| Parameter | Score | Finding |
| Pain | 25 | None |
| 20 | Mild | |
| 15 | Moderate | |
| 0 | Severe | |
| Functional capacity | 25 | Able to work |
| 20 | Limited work | |
| 0 | Unable to work | |
| Pronosupination | 25 | ≥170° |
| 15 | 141–169° | |
| 10 | 101–140° | |
| 5 | 61–100° | |
| 0 | ≤60° | |
| Prehensile strength (compared to healthy wrist) | 25 | 100% |
| 15 | 75–99% | |
| 10 | 50–74% | |
| 5 | 25–49% | |
| 0 | 0–24% | |
The analysis of preoperative and postoperative joint balance, after verifying that the sample had a non-normal distribution by applying the Kolmogorov-Smirnov and Shapiro-Willis tests, was done through the Wilcoxon test for nonparametric tests and paired variables to confirm the existence of a significant difference of means with an error probability below the threshold established (P<.05).
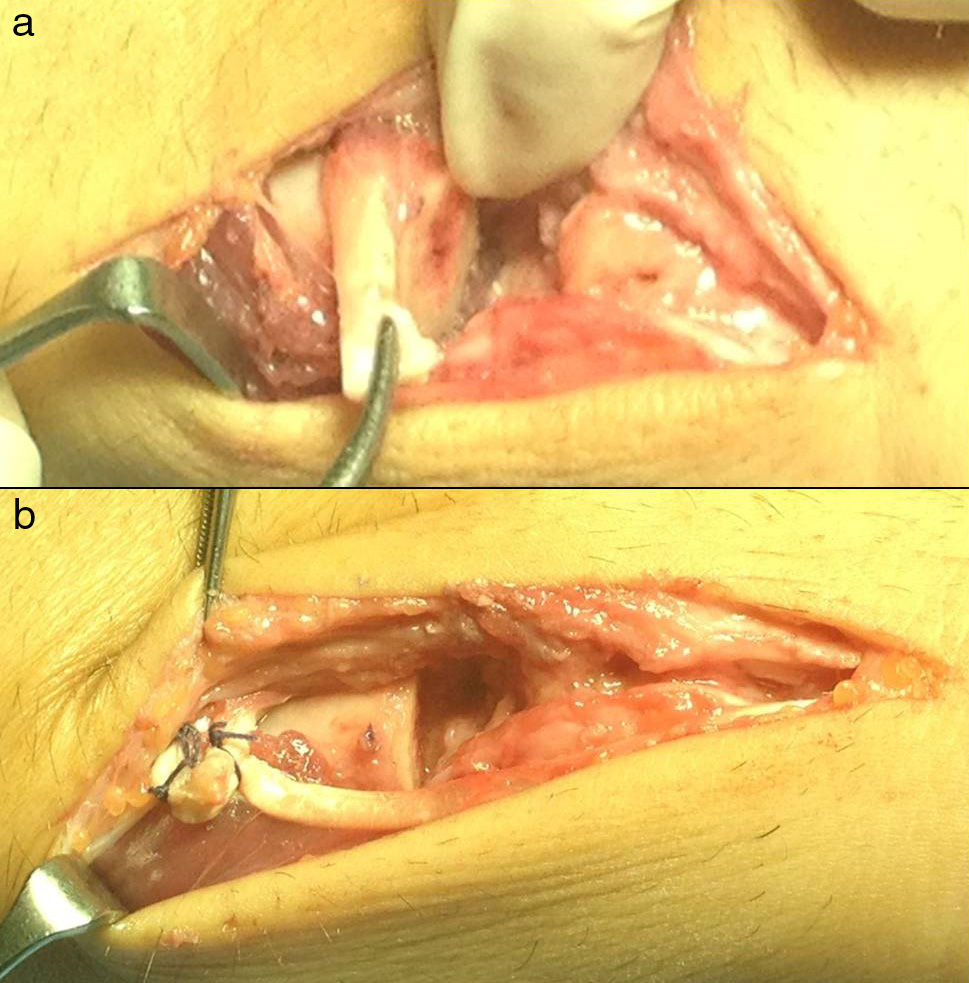
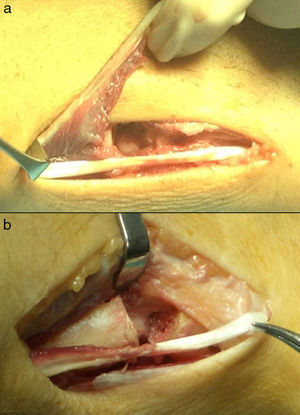
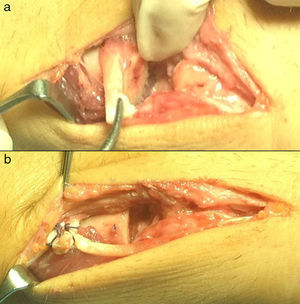
Surgical technique and postoperative treatmentWe performed a longitudinal incision on the sixth extensor compartment from the ulnar styloid up to 4cm proximal to it, thus avoiding the dorsal sensory branch of the ulnar nerve, which remained distal to the incision.
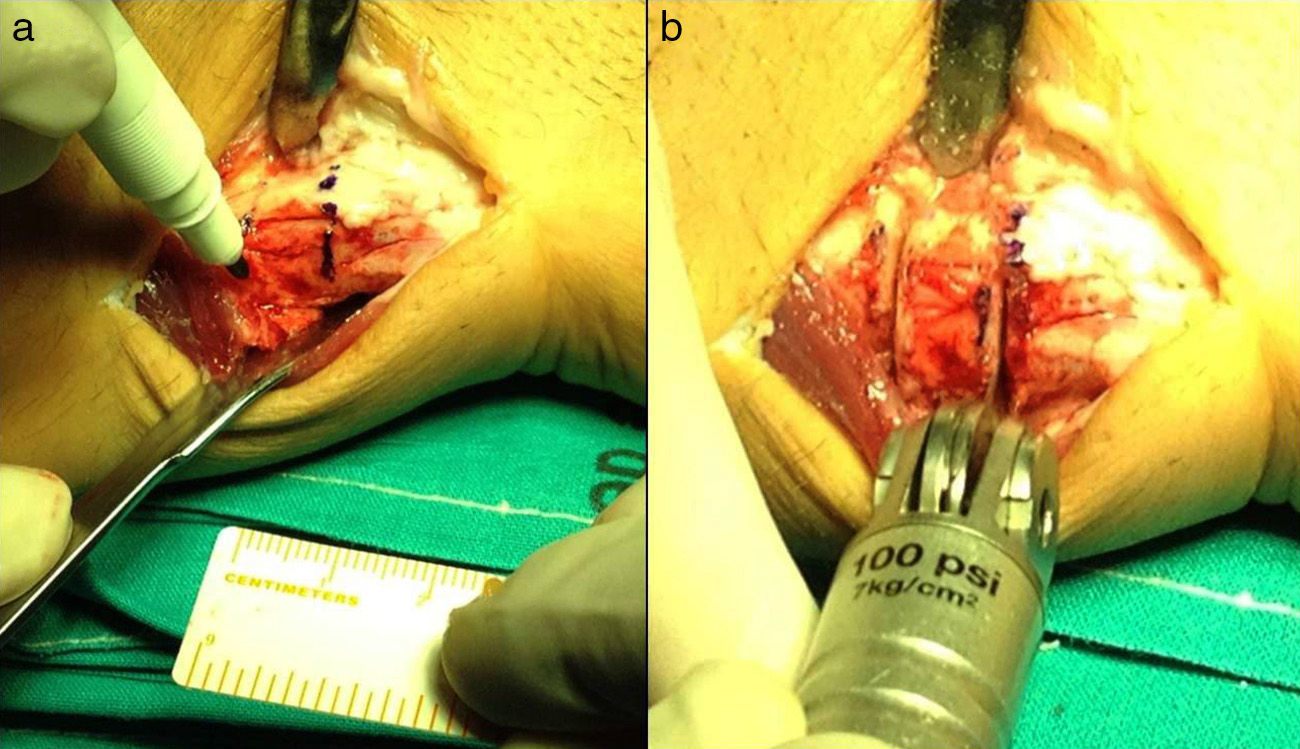
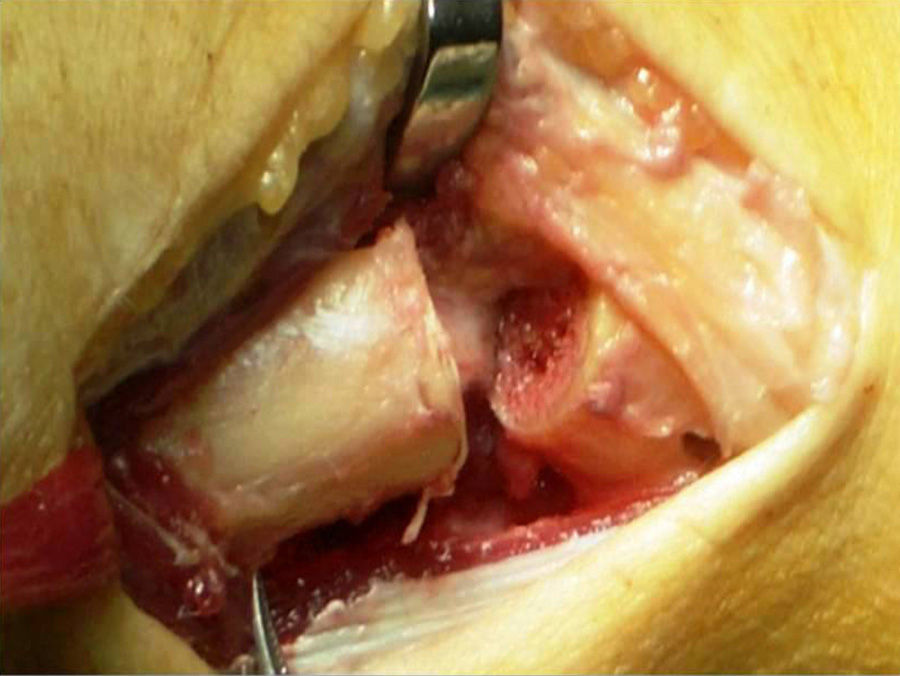
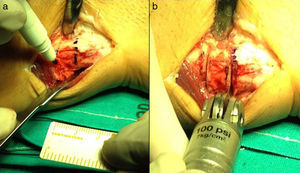
The sixth extensor compartment was displaced radially to expose the distal end of the ulna and the fifth extensor compartment was opened to retract the extensor digiti minimi. We performed a capsulotomy like an L-type flap in the ulnar base, proximal to the triangular fibrocartilage, and excised the periosteum around the neck of the ulna. Subsequently, we marked and resected a 10mm segment of the distal diaphyseal portion of the ulna up to 10–15mm from the distal joint surface of the ulna (Fig. 2), whilst also correcting the ulnar length if necessary (Fig. 3). It was important to correctly denude the cartilage of the sigmoid cavity of the radius and the articular surface of the ulnar head to achieve arthrodesis.
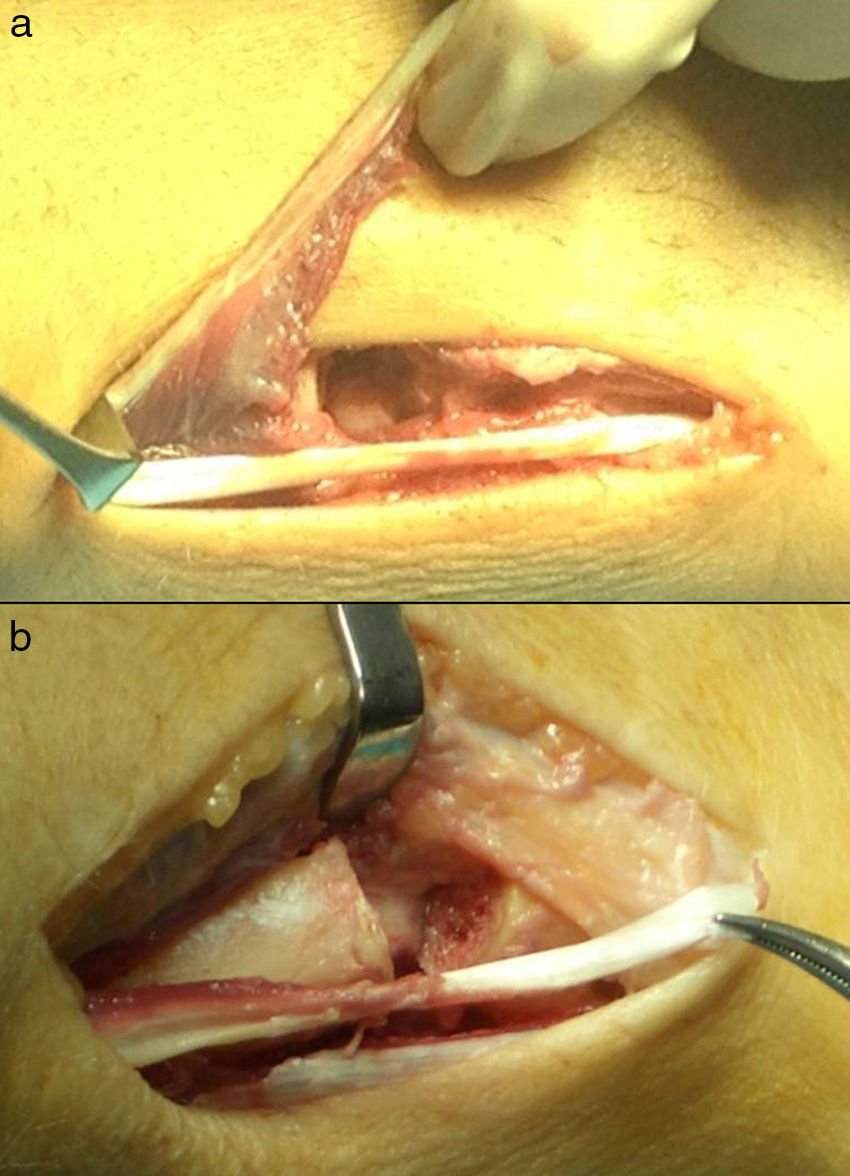
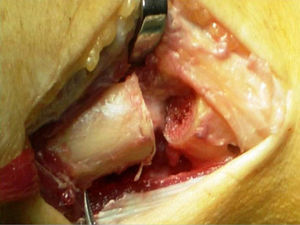
We proceeded to fix the ulnar head with 2 cannulated compression screws or, failing that, a single, standard, 3.5mm Acutrak screw (Acumed®, USA) and a 1.8mm Kirschner wire to prevent rotation of the distal segment during screw insertion. We employed a variation of the technique described by Minami et al.15,16 to stabilize the proximal ulnar stump, using a hemitendon band of the extensor carpi ulnaris (ECU) (Fig. 4) to perform an interposition plasty, like a tie or scarf over the proximal ulnar stump and suturing the tendon on itself (Fig. 5), instead of making a bone tunnel in the ulna to suture the plasty. Lastly, we partially placed the pronator quadratus at the resection site to achieve pseudoarthrosis. During the postoperative period we used a forearm splint for 3–4 weeks, after which we began a protocol of active wrist rehabilitation.
As complications, 6 patients suffered symptomatic instability of the proximal ulnar stump (2 of them required a new surgical intervention associating a combined stabilization technique through the ECU and the flexor carpi ulnaris [FCU]), 1 patient presented postoperative sensory alterations in the area of the ulnar dorsal cutaneous branch, 2 patients presented absence of fusion of the arthrodesis after 1 year follow-up which required a new surgical intervention to achieve fusion, and 1 patient continued to suffer pain at the distal radioulnar level which required another intervention for the implantation of a distal, radioulnar Aptis®-type Scheker prosthesis.
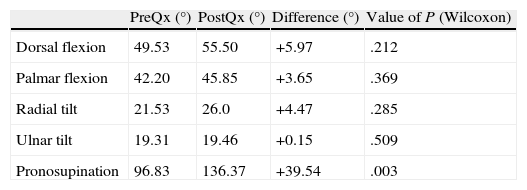
The mean preoperative dorsiflexion of the wrist was 49.5°, which varied to 55.5° at the time of the review. Mean preoperative palmar flexion was 42.2°, which varied to 45.9° at the time of assessment. Mean ulnar tilt varied from 21.5° preoperatively to 26.0°, whilst radial tilt increased from 19.3° preoperatively to 19.5° at the time of the review. None of these variations was statistically significant. The pronosupination arc increased from a mean preoperative value of 96.8° to a mean postoperative value of 136.4° (Table 4). This increase was statistically significant according to the Wilcoxon test (P=.003).
Mean degrees of joint balance.
| PreQx (°) | PostQx (°) | Difference (°) | Value of P (Wilcoxon) | |
| Dorsal flexion | 49.53 | 55.50 | +5.97 | .212 |
| Palmar flexion | 42.20 | 45.85 | +3.65 | .369 |
| Radial tilt | 21.53 | 26.0 | +4.47 | .285 |
| Ulnar tilt | 19.31 | 19.46 | +0.15 | .509 |
| Pronosupination | 96.83 | 136.37 | +39.54 | .003 |
P: statistical significance; PostQx: postoperative mean; PreQx: preoperative mean.
One year after surgery, 16 patients (59.2%) reported suffering mild or no pain, and no limitations for activities of daily living, 8 patients (29.6%) reported moderate pain requiring continuous medication, whilst 3 patients (11.1%) suffered a level of pain which was severe and disabling for activities of daily living.
Mean grip strength was maintained at 50.6% compared to the healthy contralateral wrist at 6 months follow-up. Return to work without limitations was possible in 13 patients (48.15%), 10 patients (37.04%) returned to their previous work with some restrictions, and 3 patients were unable to return to work (11.11%).
According to the radiological criteria of Knirk and Jupiter, the preoperative radiograph showed severe degenerative changes in 11 cases, moderate in 11 cases and mild or absent in 5 cases (although these presented symptoms of distal radioulnar degeneration and a positive friction test). The radioulnar ratio increased from a mean preoperative value of +2.6mm (−9.1mm to +8.4mm) to a mean postoperative value of 0.39mm (−6.4mm to +2.0mm), with this variant resulting postoperatively neutral or negative in 23 cases. The mean length of the osteotomy was 13mm (8–18mm). The control radiograph performed at 8 weeks after surgery showed radiographic consolidation of distal radioulnar arthrodesis in 25 cases, whilst there were 2 cases with no clinical or radiographic evidence of fusion.
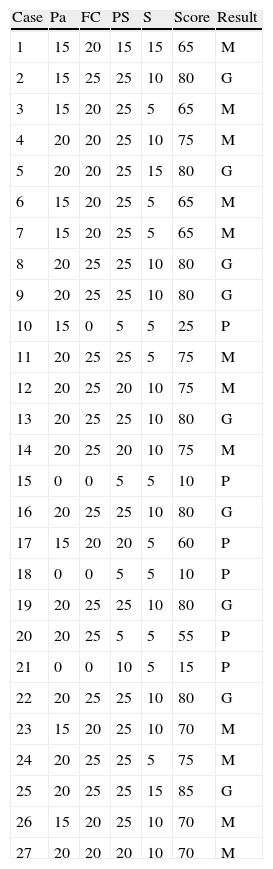
According to the Mayo Clinic wrist rating scale there were no excellent results in any case, good results were obtained in 9 cases (33.33%), moderate in 12 cases (44.44%), and poor in 6 cases (22.22%), with a mean score of 64.62±17.6 points out of 100 (Table 5). The DASH functional test obtained a mean score of 41.32 points (range: 0–77.5 points) in the postoperative period.
Mayo clinic wrist assessment scale results individualized by each patient.
| Case | Pa | FC | PS | S | Score | Result |
| 1 | 15 | 20 | 15 | 15 | 65 | M |
| 2 | 15 | 25 | 25 | 10 | 80 | G |
| 3 | 15 | 20 | 25 | 5 | 65 | M |
| 4 | 20 | 20 | 25 | 10 | 75 | M |
| 5 | 20 | 20 | 25 | 15 | 80 | G |
| 6 | 15 | 20 | 25 | 5 | 65 | M |
| 7 | 15 | 20 | 25 | 5 | 65 | M |
| 8 | 20 | 25 | 25 | 10 | 80 | G |
| 9 | 20 | 25 | 25 | 10 | 80 | G |
| 10 | 15 | 0 | 5 | 5 | 25 | P |
| 11 | 20 | 25 | 25 | 5 | 75 | M |
| 12 | 20 | 25 | 20 | 10 | 75 | M |
| 13 | 20 | 25 | 25 | 10 | 80 | G |
| 14 | 20 | 25 | 20 | 10 | 75 | M |
| 15 | 0 | 0 | 5 | 5 | 10 | P |
| 16 | 20 | 25 | 25 | 10 | 80 | G |
| 17 | 15 | 20 | 20 | 5 | 60 | P |
| 18 | 0 | 0 | 5 | 5 | 10 | P |
| 19 | 20 | 25 | 25 | 10 | 80 | G |
| 20 | 20 | 25 | 5 | 5 | 55 | P |
| 21 | 0 | 0 | 10 | 5 | 15 | P |
| 22 | 20 | 25 | 25 | 10 | 80 | G |
| 23 | 15 | 20 | 25 | 10 | 70 | M |
| 24 | 20 | 25 | 25 | 5 | 75 | M |
| 25 | 20 | 25 | 25 | 15 | 85 | G |
| 26 | 15 | 20 | 25 | 10 | 70 | M |
| 27 | 20 | 20 | 20 | 10 | 70 | M |
FC: functional capacity; G: good; M: moderate; P: poor; Pa: pain; PS: postoperative pronosupination; S: grip strength compared to healthy, contralateral wrist.
The congruence between the sigmoid notch and the joint surface of the ulnar head enables a combination of rotation and translation movements during forearm pronosupination. Changes in the distal radioulnar ratio during supination justify the importance of conducting a proper AP radiograph of the wrist. However, a recent study has shown that the changes in ulnar variance were minimal throughout the rotation arc of the forearm, with a difference of only 0.6mm between pronation and supination.2
When the distal radioulnar joint shows signs of arthropathy or an alteration in its morphology there is no ideal procedure that can restore its anatomy and function. The existence of multiple surgical options leads to a discussion about the most effective method in the treatment of this condition. At present, the use of the Darrach technique has been restricted to rheumatic hands with instability secondary to carpal supination. Goncalves17 (1974) analyzed a series of 22 cases treated using the Sauvé-Kapandji technique and consistently obtained better results than those described historically with the Darrach technique. However, recent studies18 reported similar results after comparing both techniques.
The Sauvé-Kapandji procedure represents a useful alternative in the treatment of disorders of the distal radioulnar joint, albeit not an infallible one.19,20 Taleisnik20 (1992) described a series of 24 patients in whom he managed to restore forearm rotation and minimize pain with a low complication rate with a minimum follow-up period of 1 year. The benefits of the Sauvé-Kapandji technique could be due to several factors: the distal radioulnar arthrodesis for pain relief, the distal resection of the ulna to correct the distal radioulnar ratio and pseudoarthrosis to maintain forearm pronosupination. Most authors refer to the importance of maintaining the ulnar head,21,22 which would imply a number of advantages brought about by stabilization of the posterior ulnar tendon in its compartment, preservation of the ulnar-carpal ligaments and a normal aesthetic aspect of the wrist.
Regarding joint balance, in accordance with the findings reflected by previous studies,23,24 our study found a statistically significant improvement in the pronosupination arc (P=.003). When assessing the score obtained for the DASH scale, we must bear in mind that this scale is based on subjective parameters, also analyzing shoulder and elbow function that the results were not comparable according to whether the limb is dominant or not and that our study did not include preoperative measurements which enabled us to assess the evolution, so we do not believe that it was overly valuable to draw conclusions, despite showing similar results to those reflected in the literature.25
The main complication described for the Sauvé-Kapandji technique is the appearance of instability in the proximal ulnar stump due to the damage suffered by the radioulnar stabilizers.26 Our study showed a similar rate of occurrence of this complication to that reported by other authors,26,27 although it was not always symptomatic. Multiple modifications of the original technique have been described in order to reduce such instability, including the use of the ECU, the FCU or combined techniques, with all of them reporting discrete outcomes.17,28 In our study, the length of the ulnar osteotomy decreased gradually with the level of experience, as there are now some studies that advocate osteotomies not exceeding 10mm in order to minimize radioulnar impingement during pronosupination.29
We believe that the high number of patients who suffered postoperative pain after 1 year (11 patients, 40.7%) could be explained by the high number of complications reported, such as 6 patients with instability of the proximal stump despite performing a variation of the Minami technique (2 of which required subsequent surgeries) and 2 cases of distal radioulnar nonunion (which we believe might be explained by an insufficient denudation of the cartilage of the sigmoid cavity of the radius and the joint surface of the ulna) and other causes, such as bursitis caused by ECU snapping. Nevertheless, 23 patients (85.2%) reported an improvement of pain compared to their previous condition.
In conclusion, we can highlight that our study was consistent with the literature regarding the positive results obtained for improvement of the pronosupination arc,19 with an acceptable improvement of the pain level compared to the previous condition. However, it also showed the frequent loss of grip strength and the frequent occurrence of pain and instability in the proximal ulnar stump.
Level of evidenceLevel of evidence iv.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation adhered to the ethical guidelines of the Committee on Responsible Human Experimentation, as well as the World Medical Association and the Declaration of Helsinki.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: García-López M, Pareja-Esteban JA, Valmaña-de la Sotilla JM, Jiménez-Alcázar LC, Martínez-Calvo MA, Plasencia-Arriba MA. Procedimiento de Sauvé-Kapandji en los trastornos de la articulación radiocubital distal. Rev Esp Cir Ortop Traumatol. 2013;57:340–347.