Triquetral fractures are the second most common fractures of the carpal bones, following those of the scaphoid bones. They represent approximately 3%–5% of the fractures of the bones comprising the carpus,1 reaching 15% of the fractures in this anatomical area in some series.2 It is extremely rare for it to present bilaterally. The cause is generally a fall with support of the hand in hyperextension and cubital deviation.
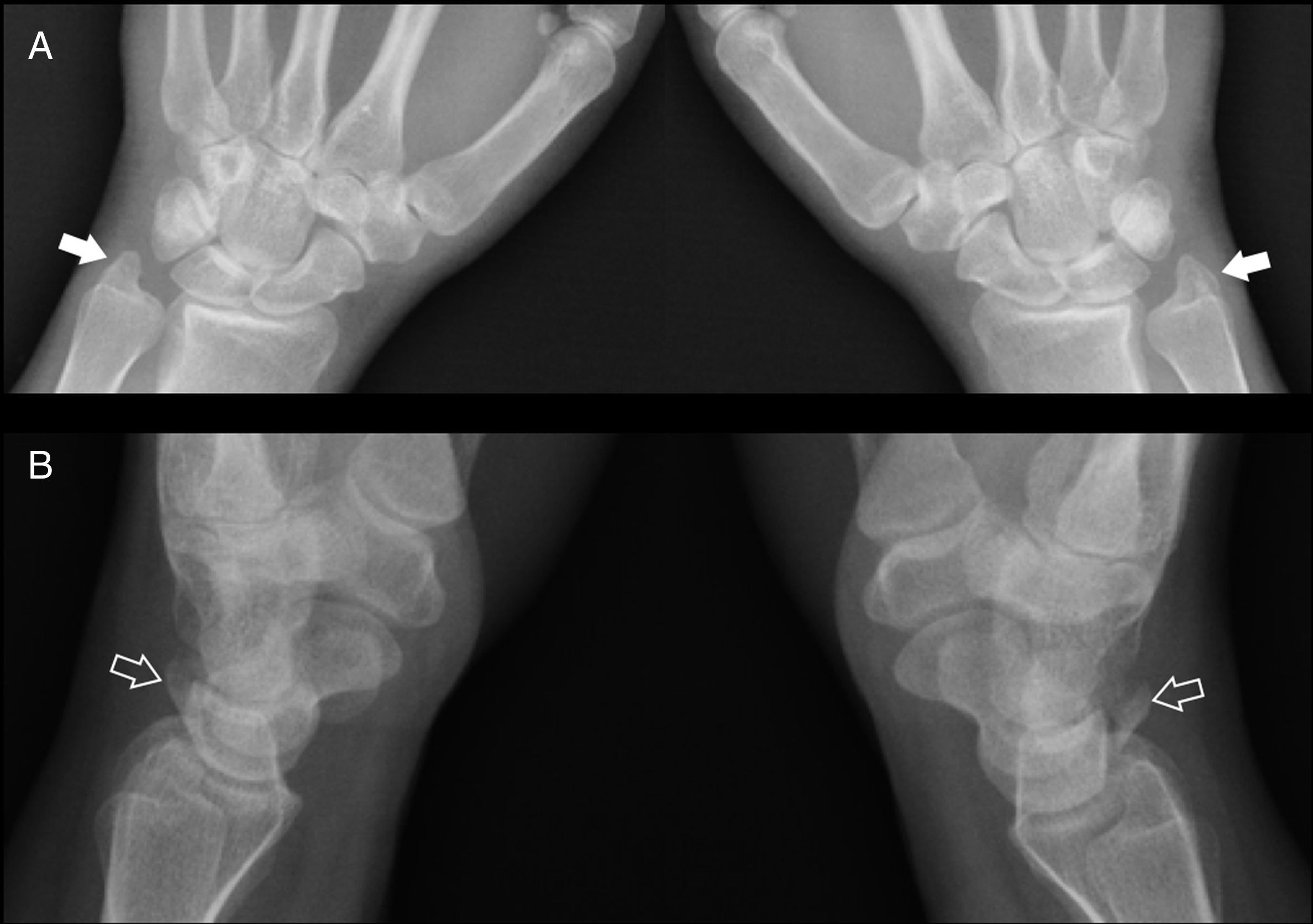
Clinical caseWe present the case of a 30-year-old woman that came to emergency services following a fall to the ground with support of both hands in forced hyperextension. During the physical examination, the patient reported diffuse pain in the back of the radiocarpal joints. A lateral anteroposterior X-ray was taken of both wrists, in which a fracture of the scaphoid bones was ruled out (Fig. 1). The patient was released with a plaster splint and the clinical diagnosis of bilateral scaphoid bone fractures. Follow-up of radiological control in 10 days and orthopaedists consultation at 15 days was indicated.
Anteroposterior (A) and lateral (B) X-ray images of both wrists at the time of the fall. In image A, no evident signs of scaphoid fracture can be seen. Prominent ulnar styloid bones (white arrows). In Image B, there is an osseous tear of both triquetral bones (dark arrows) that was unseen in emergency services.
In the radiological control (not shown), a scaphoid bone fracture was ruled out and standard painkillers were recommended. When the plaster was removed in the orthopaedists consultation, there was no pain perceived in the anatomical snuff-box, although there was in the cubital area and the dorsal carpus. The previous lateral X-rays were evaluated and a possible bilateral dorsal cortical fracture of the triquetral was noted (Fig. 1). For that reason, a computed tomography (CT) scan of both wrists was requested for better assessment.
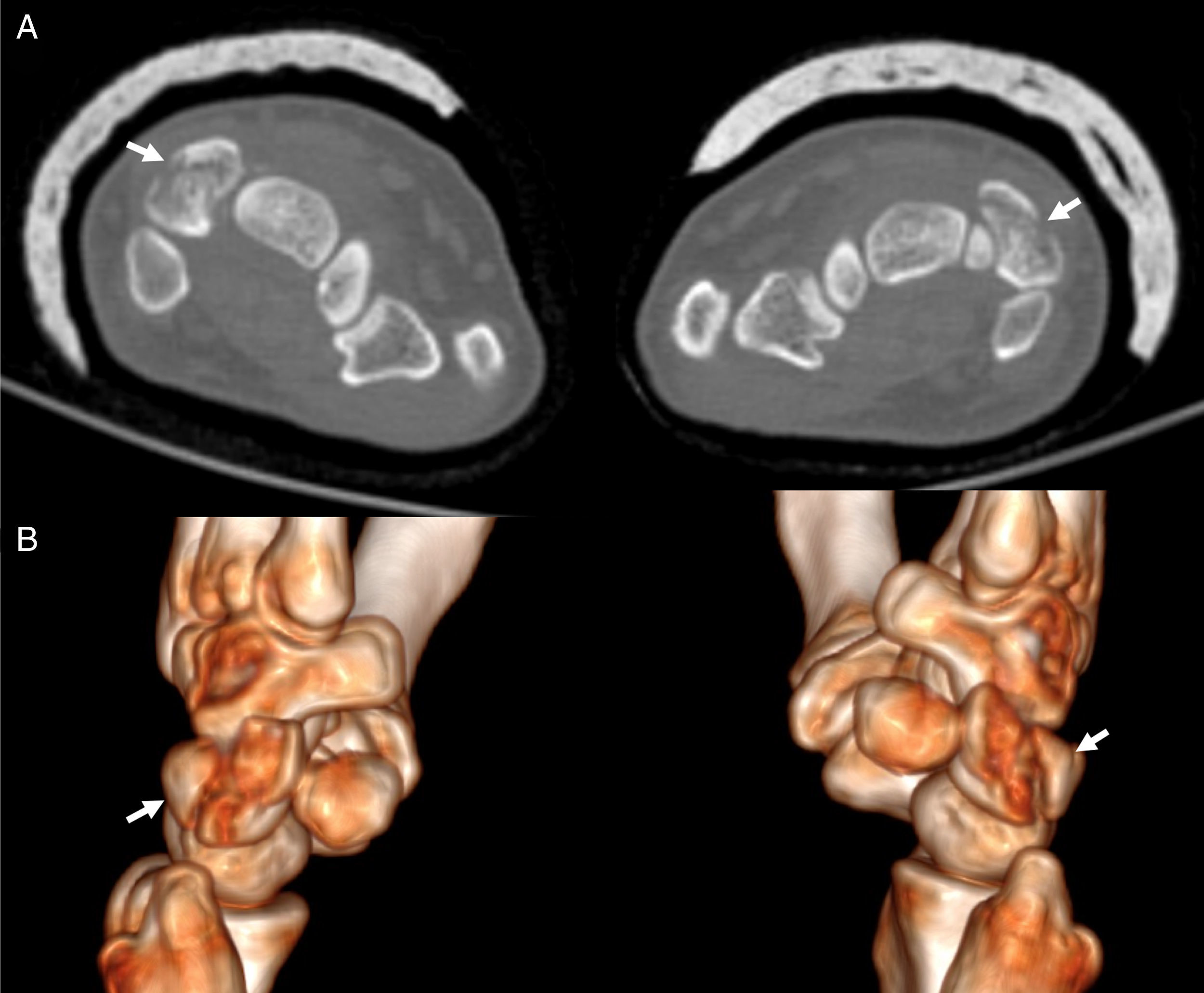
In the CT, the existence of a dorsal cortical avulsion fracture in both triquetral bones was confirmed (Fig. 2). After a total of 6 weeks of immobilisation with plaster splint, the patient had no symptoms.
DiscussionTriquetral bone fractures can be classified as dorsal cortical avulsion (>90%), palmar cortical and of the body. There are several main theories that explain the fracture mechanism. Some authors have proposed that the cause is that the triquetral bone impacts the styloid apophysis of the ulna3 or the hamate. At other times, avulsion fractures of the area of dorsal ligamentous insertion (intrinsic ligaments such as the dorsal intercarpal dorsal and extrinsic such as the dorsal ulnar triquetral and dorsal radiocarpal ligaments) are involved; such fractures tend to happen in falls where the hand is in palmar flexion position.2,4,5 A high level of clinical suspicion should exist, given that they are generally overlooked in simple X-rays. Clinically, triquetral fractures usually evolve with pain and inflammation in the dorsal triquetral bone, as dorsal cortical tears are involved in the great majority of cases.
Anteroposterior (AP) views in X-rays are of limited use; lateral and oblique lateral views at 45° pronation are necessary. If there is clinical suspicion and conventional X-rays are negative, a CT scan would be the technique of choice.5 Magnetic resonance imaging has shown itself useful in evaluating ligament integrity in dorsal cortical fractures.6
Treatment of dorsal cortical fractures consists of immobilisation for 3–6 weeks; the pain usually disappears in approximately 4–8 weeks.2 The risk of avascular necrosis is very low and if symptoms persist after this period, injury to the triangular fibrocartilage complex should be suspected.4
In our case, the initial pain in the anatomical snuff-box focused the study on assessment of the scaphoid bones. This, together with the existence of symmetrical finding in the lateral X-ray, caused the fractures to go unnoticed at first.
Bilateral triquetral bone fractures are rare, with there being only 1 published case of simultaneous bilateral fracture caused by the same trauma. There should be a high level of clinical suspicion for diagnosing them, given that simple X-ray in AP view will not provide the diagnosis and the assessment can be difficult in a lateral view due to there being symmetrical findings. In our case, strong clinical suspicion, re-evaluation of the X-rays and the CT scan made it possible to reach the diagnosis.
Level of evidenceLevel of evidence V.
Please cite this article as: Martínez-Martínez A, García-Espinosa J. Fractura bilateral simultánea del piramidal. Rev Esp Cir Ortop Traumatol. 2017;61:286–288.