Dorsal wrist pain is a very common cause of complaint in the clinical practice of the hand surgeon. Such pain can frequently be related to traumatic, inflammatory or degenerative diseases, but sometimes its origin is far away from these common causes.
A rare case is reported of chronic dorsal wrist pain of neuropathic origin, due to a pre-capsular neuroma of the posterior interosseous nerve. Possible causes, diagnostic hints, and treatment options are thoroughly discussed.
El dolor en el dorso de la muñeca es una causa frecuente de consulta médica en nuestra práctica clínica habitual.
Normalmente este dolor puede ser debido a procesos traumáticos, inflamatorios o degenerativos. Pero en ocasiones el origen del dolor se aleja de estas causas frecuentes.
Presentamos un caso de dolor crónico al nivel dorsal de muñeca sin claro antecedente traumático ni componente degenerativo o inflamatorio atribuible. Siendo de etiología neuropática, debido a un neuroma del nervio interóseo posterior precapsular. Se discuten posibles causas, métodos de diagnóstico y opciones de tratamiento.
Dorsal wrist pain is a common reason for medical consultation in our daily clinical practice.
Such pain is normally due to traumatic (fracture, sprain, muscle–ligament strain), inflammatory (rheumatoid arthritis, psoriatic arthritis, gout, pseudogout, infectious arthritis) or degenerative processes (tendinosis, osteoarthritis). However, the origin of the pain is sometimes different from these frequent causes.
We present a case of dorsal wrist pain lacking a clear traumatic cause and attributable inflammatory or degenerative component. The pain was of neuropathic origin, from a pre-capsular neuroma of the posterior interosseous nerve.
Anatomical detailsFrom the terminal division of the radial nerve, proximal to the elbow joint space, the sensory superficial branch and the deep branch (posterior interosseous nerve) arise with motor fibres and proprioceptive fibres for the wrist joint capsule. It descends outwards in the shape of a spiral. At approximately 2cm from the space, it enters the thickness of the supinator muscle, running between its heads (Fig. 1). It goes over the origin of the abductor pollicis longus to a location in the posterior side of the interosseous membrane (Fig. 2). It continues covered by the finger extensor tendons and, once the extensor pollicis longus is innervated, it sends small branches for the distal radioulnar joint. It enters the fourth extensor compartment, occupying a deep radial position, and it divides into three or four branches (Fig. 3), expanding over the dorsal capsule for the radiocarpal, mediocarpal and carpometacarpal joints and perforating the capsule at the scapholunate level.1–4
Posterior interosseous nerve (a), entering the supinator muscle (b). Superficial branch of the radial nerve (c). Author's dissection obtained in collaboration with the Laboratory of Macro- and Microdissection and Surgical Anatomy at the University of Barcelona, Hospital Clínico (Director: Dr Manuel Llusa).
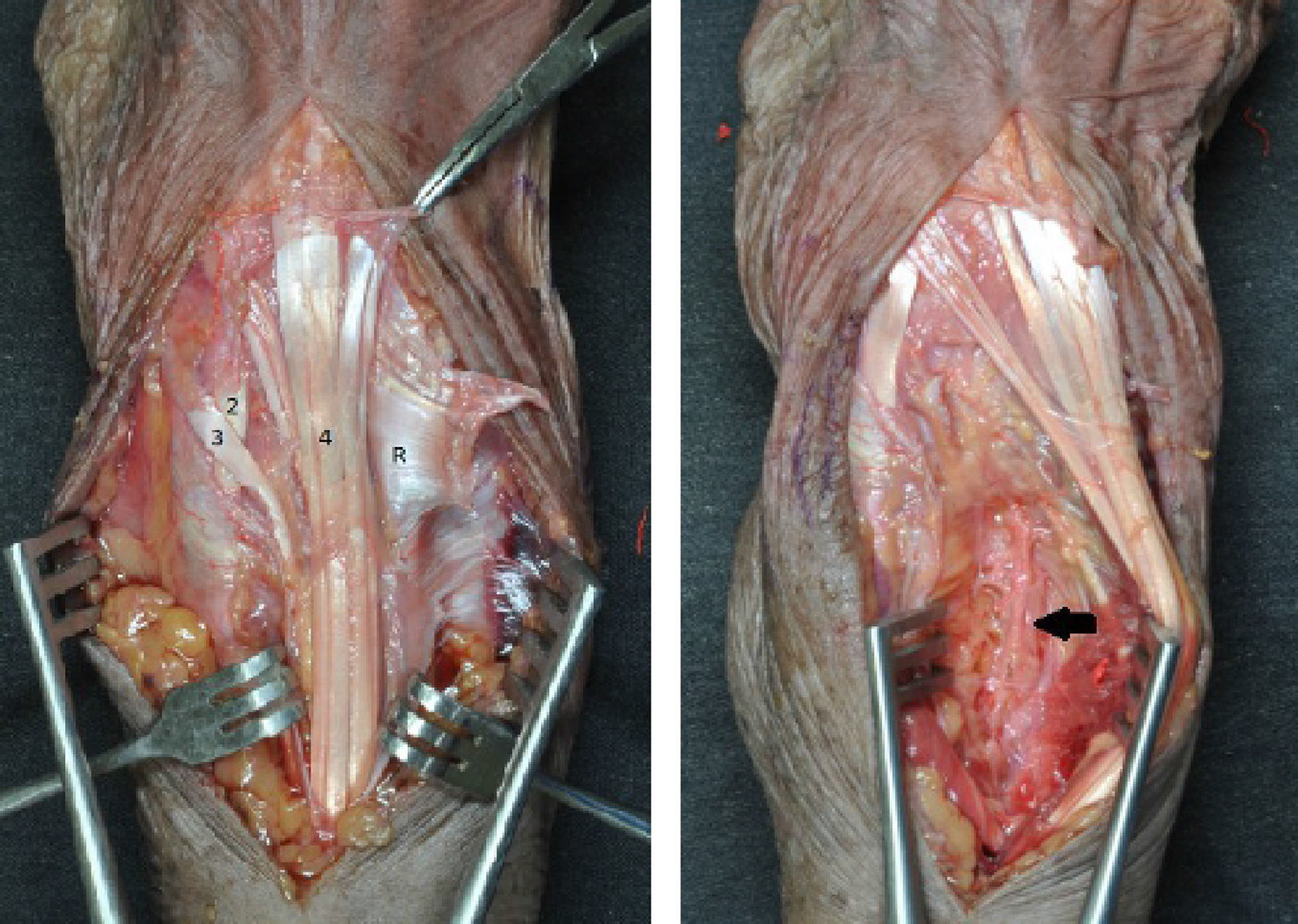
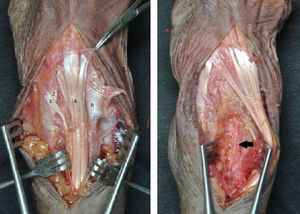
Opening of the extensor retinaculum (R) at the level of the third slip (3) exposing the fourth slip (4), followed by the retraction in cubital direction of the extensors of the fourth compartment exposing the pathway over the interosseous membrane and the floor of the fourth compartment of the posterior interosseous nerve (arrow). (2) Second extensor compartment. Author's dissection obtained in collaboration with the Laboratory of Macro- and Microdissection and Surgical Anatomy at the University of Barcelona, Hospital Clínico (Director: Dr Manuel Llusa).
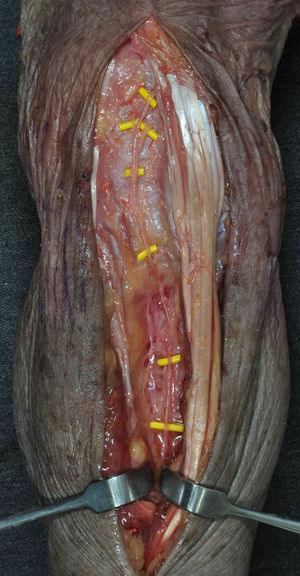
Dissection showing the posterior interosseous nerve and its trifurcation at the level of the joint capsule into three proprioceptive branches. Author's dissection obtained in collaboration with the Laboratory of Macro- and Microdissection and Surgical Anatomy at the University of Barcelona, Hospital Clínico (Director: Dr Manuel Llusa).
Along its route, it innervates the muscles of the extensor carpi radialis brevis, supinator, common extensor digitorum, extensor carpi ulnaris, extensor digiti minimi, apductor pollicis longus, extensor pollicis brevis and longus, and the extensor indicis.
Neuropathies of this nerve in its proximal area are a widely described cause of motor deficiency of the carpal extensors and the fingers, as well as of muscle hyperplasia. Algia around the epicondyle area sometimes appears (at times preceded by pain symptoms in the extensor area of the forearm), with its most common area of compression being the arcade of Frohse.5–10
Pathology at the level of its terminal branch has been reported in the literature as persistent, non-radiating poorly defined pain in the back of the wrist. High clinical suspicion is necessary, given that means available to the surgeon to back the suspected diagnosis are very limited beyond clinical expertise.11,12
Clinical caseWe present the case of a 40-year-old man without medical or surgical history of relevance. The patient did not perform high-demand work duties and enjoyed free-time cycling. He came to us, after being seen by various professionals, due to persistent wrist pain. No prior trauma injury was remembered. He had received treatment for wrist sprain, extensor tendonitis and initial inflammatory arthropathy.
The pain had begun approximately a year earlier. Conservative means, splints and standard pain killers had not improved the clinical symptoms significantly.
No trophic or vascular alterations were found in the physical examination. He had complete, non-painful joint mobility in flexion, but felt discomfort in the dorsal wrist area at maximum extension. There were no signs of joint instability or loss of strength. The pain produced with palpation of the area proximal to the dorsal joint edge of the radius.
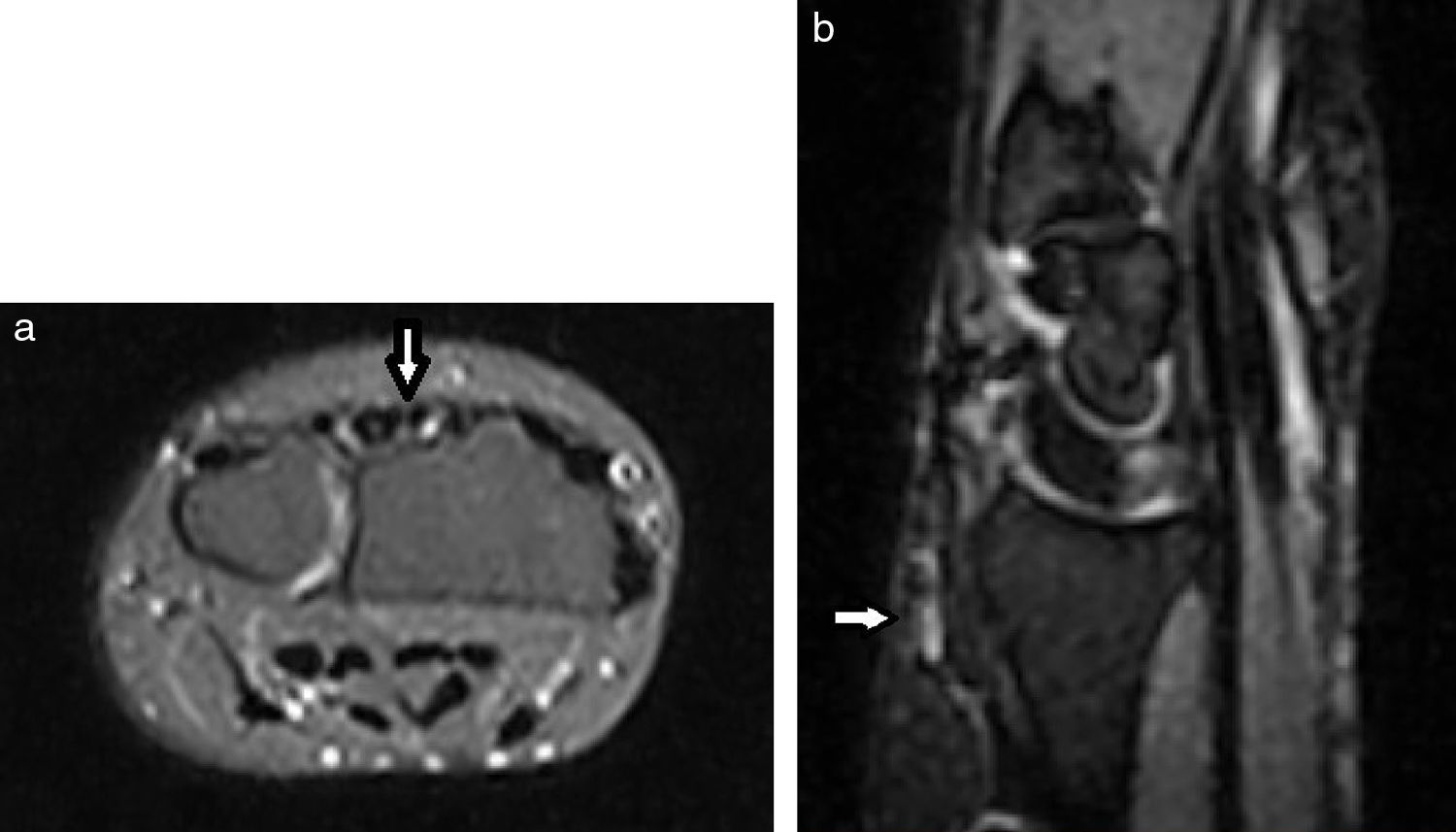
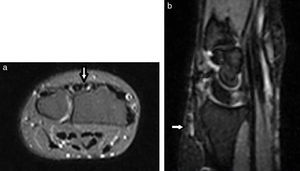
The X-rays performed did not show any degenerative pathology or joint inconsistencies in the carpal bones. Magnetic resonance imaging revealed thickening of the posterior interosseous nerve at the level of the floor of the fourth compartment (Fig. 4). No significant joint alterations were seen.
Faced with suspected distal posterior interosseous nerve syndrome, distal, a diagnostic infiltration was performed in the consultation. Lister's tubercle was located and 2ml of lidocaine was injected at a finger breath both proximally and cubitally, with immediate disappearance of the symptoms.11
Given the lengthy evolution of the condition, without improvement from conservative methods, surgery was indicated. Through a fourth compartment approach, neurotomy was performed with removal of a 2-cm increased fibrous tract of the posterior interosseous nerve.13 This was sent for pathological study, which confirmed the aetiology of neuroma (14×7mm large).
The symptoms improved a few days after the wound healed.
DiscussionPain in the dorsal area of the wrist is a common reason for consultation. Its significance is often underrated, causing patients discomfort for two reasons: Firstly, because their daily functions or activities are frequently limited (those that require wrist extension); and, secondly, because they perceive that the physician is downplaying their pathology due to lack of knowledge of the possible causes and because they receive only limited improvement with conservative remedies such as pain-killers or splints for immobilization.
Repeated patient consultations can lead the surgeon to the hasty decision to perform inappropriate interventions such as a joint revision for suspected scapholunate ligament injury or occult ganglion trauma as being pathology in the areas near the pain.
The discomfort produced in maximum wrist extension is probably provoked by a pinching mechanism after fibrosis has been produced around the nerve, as has been indicated in the literature. Although less frequent, discomfort can also appear upon maximum flexion.12 The presence of a neuroma indicates that there was some sudden or repetitive trauma, forgotten by the patient, that caused the nerve injury and fibrosis.
Possible causes of posterior interosseous nerve injury have been reported to be repetitive or forced activities that necessitate hyperextension, which in our case could be correlated with cycling, fractures or dislocations.11,13,14
Posterior interosseous nerve injury after surgical procedures focused on the radiocarpal joint have sometimes been described in the literature.15 With the current spread of arthroscopy, cases of iatrogenic injury of the nerve have also been reported.16
In our opinion, everything stems from the clinical suspicion. This pathology must be considered when other sources of pain in the dorsal wrist have been ruled out.
Differential diagnosis should include tenosynovitis of the carpus and finger extensors, radiocarpal arthritis, carpal chondromalacia, dynamic instability of the carpus, degeneration of the triangular fibrocartilage complex, positive or negative ulnar variance, avascular semi-lunate necrosis and occult ganglions.17–19
As far as we know, magnetic resonance imaging has not been described in the literature associated with this condition. We feel that it could be helpful in backing the diagnosis of suspicion, at times being able to show an increase in thickness and signal at the level of the nerve. Likewise, sonography should be considered as another imaging test that helps to guide diagnosis, as this technique is currently capable of capturing thickening of the normal contour of a nerve of this size.
Once the source of the pain is known and there is a solid basis, it becomes possible to explain the treatment options to the patient. It is possible to opt for a conservative attitude (a splint and drugs to block the transmission of pain), infiltration of anaesthetic11 or resection of the neuroma if the symptoms last longer than 6 months and there is an anatomopathological study that offers diagnostic certainty.
Level of evidenceLevel of evidence V.
Ethical disclosuresProtection of people and animalsThe authors declare that no experiments have been carried out on human beings or animals for the purpose of this research.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre about the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflicts of interest to declare.
We wish to thank the Institut Kaplan, Barcelona, Spain.
Please cite this article as: Pérez Abad M, Llusa Pérez M, Giacalone F. El neuroma de la porción distal del nervio interóseo posterior como causa de dolor dorsal persistente de muñeca. Rev Esp Cir Ortop Traumatol. 2017;61:281–285.