Reverse total shoulder arthroplasty in rotator cuff arthropathy patients, improves anteversion and abduction, but not rotational, outcomes. The main aim of this study is to determine its repercussions on daily life activities in our patients.
Material and methodsBetween 2009 and 2011 we implanted 210 shoulder arthroplasties, 126 of them were reverse total shoulder arthroplasty in a rotator cuff arthropathy context. About 88% were women, with a mean age at time of surgery of 81 years, 95% were retired. The mean follow up was 53 months. The Constant scale, Visual Analogue Scale, Charlson Comorbidity Index, and range of motion were measured for each patient and whether they could manage 40 daily life activities by means of a new questionnaire, classifying them according to shoulder functional demand.
Results and discussionMean normalised by sex and age Constant value was 81.2%. Mean Visual Analogue Scale and Charlson Index were 3.56 and 1.69 respectively. Improvement in anteversion and abduction, not in rotational range of motion. Limitation was found in low and high functional demand activities in 20% and 51% respectively, especially those which involved internal rotation.
ConclusionReverse total shoulder arthroplasty treatment for RCA in the elderly, achieves adequate pain management and good functional outcomes. Nevertheless, an important risk of DLA limitation must be accepted in those which involve internal rotation or shoulder high functional demand.
La artroplastia total de hombro inversa en el contexto de la artropatía de manguito rotador mejora la anteversión y abducción existentes, no así las rotaciones. Nuestro objetivo es determinar la repercusión de este hecho en la realización de actividades más cotidianas.
Material y métodosEntre 2009 y 2011 se implantaron 210 artroplastias de hombro en nuestro centro. De ellas, 126 artroplastias totales de hombro inversas por artropatía de manguito rotador. El 88% eran mujeres, con una edad media en el momento de la cirugía de 81 años, encontrándose el 95% laboralmente retirados. El seguimiento medio fue de 53 meses. En cada paciente fue valorada la escala Constant, la escala visual analógica e índice de comorbilidad de Charlson, el balance articular así como la capacidad de realización de 40 actividades cotidianas, divididas según grado de demanda funcional para el hombro en un cuestionario nuevo adaptado a nuestro grupo poblacional.
Resultados y discusiónEl Constant medio normalizado por edad y sexo fue del 81,2%. EL valor medio de la escala visual analógica e índice de comorbilidad de Charlson medios de 3,56 y 1,69 respectivamente. Mejoría del balance articular en anteversión y abducción, no en rotaciones. Limitación para realizar actividades de baja y alta demanda funcional del 20 y 51% respectivamente, apreciándose mayor limitación en aquellas que implican rotación interna.
ConclusiónLa artropatía de manguito rotador en el paciente anciano tratada mediante artroplastia total de hombro inversa consigue un adecuado control analgésico y buenos resultados funcionales. Sin embargo, hay que asumir un importante riesgo de limitación en actividades cotidianas de alta demanda y que impliquen rotaciones, sobre todo interna.
Reverse total shoulder arthroplasty (RTSA) is now a highly topical subject within the field of shoulder pathologies. There are currently more than 300 indexed articles on this subject, and although the first of these appeared in the final decade of the last century and the first decade of the current one, more than 65% of publications to date appeared after 2010. The majority of these centres on indications, surgical approaches, specific aspects of surgical technique, rehabilitation protocols, follow-up or complications. These articles use different scales to measure functional results. Nevertheless, few works at world level and even fewer within our own context analyse the results of our intervention using questionnaires about everyday activities to examine where patients find the greatest difficulties.1–4 These questionnaires enable us to discover the specific improvements in patients’ lives which arise due to our intervention.
We are increasingly less restrictive in our use of prostheses of this type, in terms of pathology and patient age. An implant that was initially designed for use in rotator cuff arthropathy with a pseudo-paralytic arm is now used to treat primary glenohumeral arthrosis, glenohumeral arthrosis that is secondary to trauma or rheumatism, massive fractures of the rotator cuff, revision shoulder surgery and tumour lesions, as well as in the management of proximal humerus fractures with 3 and 4 fragments. Likewise, although this prosthesis was first used only in elderly patients (over the age of 76–89 years old), an increasing number of publications describe its use in considerably younger patients.5–7 This is largely due to the good results it gives and the reproducibility of the same.
RTSA improves pain and mobility in anteversion and abduction (due to the resulting increase in leverage arm length and the fact that it helps the functioning of the deltoid muscle). However, external rotation is severely compromised, and this has even given rise to the introduction of technical modifications to improve the results obtained in this parameter.5,8,9
Our study aims to discover the specific everyday activities in which rotator cuff arthropathy RTSA patients have the greatest restrictions. These patients form a population sample within the health care area in which we work.
Material and methodsFrom an initial sample of 210 patients treated surgically by RTSA in our centre from 2009 to 2011, we selected 126 in which the surgical indication was rotator cuff arthropathy to undertake a retrospective descriptive study of their clinical and functional status. 10 patients were excluded from the total of 126 as it was impossible to contact them (because of change of address in 3 cases and death due to causes unconnected with the prosthesis in 7 cases).
All of the patients were operated by 3 shoulder surgery specialist surgeons following the same surgical technique. The approach was superolateral in 76% of cases and deltopectoral in the remaining 24%, with subscapular re-insertion and placement of the humeral rod at 30° retroversion. During the immediate postoperative stage the patients commenced pendular and assisted exercises taught by the physiotherapist before discharge. They then followed a rehabilitation protocol for at least 6 weeks.
The epidemiological data gathered include age, sex, dominant or non-dominant affected arm, working status and associated comorbidities.
We conducted a personal interview with all of the patients during the study, recording the following data:
- -
Pain, using the analogue visual scale.10 This makes it possible to quantify pain intensity and therefore how it evolves after different therapies.
- -
Medication: whether or not analgesic medication was required and the level of this on the WHO scale.11
- -
Function: on the Constant–Murley12 scale adjusted for age and sex. This expresses the situation of the patient numerically, combining pain, functional limitation, strength and mobility.
- -
Comorbidity: this uses the Charlson Comorbidity Index.13 This determines the degree of comorbidity and predicts the risk of patient mortality at 3 years depending on their overall medical condition. A score of 1–6 associated with each patient pathological process is generated. The sum of all these scores gives the final comorbidity score: absent (0 points), low (1–2 points) or high (3 or more points); this is equivalent to a probability of death at 3 years expressed as a percentage.
- -
Joint balance measurement: anteversion, abduction and rotational.
- -
The performance of everyday activities: a personal questionnaire was used to evaluate the ability to perform certain everyday activities, This was based on the one published by Cofield's1,2 work group and was adapted to our population group with 40 items (Table 1). The activities in question involve washing, personal care, housework, leisure activities and social relationships as well as physical and mental exercise. The subjects were divided into 3 groups according to the functional demands made on the shoulder joint:
- ∘
Low functional demand: activities that do not involve repetitive joint stress or the lifting of any weight, in which the arm remains below shoulder height for the majority of the time.
- ∘
Moderate functional demand: activities involving potential repetitive joint stress, lifting weights of less than 4kg, and activities in which the arm is sometimes above shoulder height.
- ∘
High functional demand: activities involving repetitive joint stress, lifting weights of more than 4kg and activities in which the arm functions at more than 90° anteversion or abduction.
Table 1.Percentage of patients who perform different low, moderate and high functional demand activities.
Low demand, % Moderate demand, % High demand, % Talking by telephone, 88 Sweeping/mopping the floor, 69 Pulling shopping trolley, 57 Cooking, 72 Washing-up, 39 Caring for other individuals, 57 Sewing, 75 Ironing, 11 Driving, 69 Combing hair, 85 Making the bed, 69 Carrying own luggage, 48 Scratching back, 8 Home DIY, 48 Cleaning windows, 11 Unfastening brassiere, 3 Transfers, 75 Taking out rubbish, 63 Shower/bath, 55 Fitness gym, 11 Changing light bulbs, 11 Dressing, 80 Carrying a bag, 70 Racquet sport, 0 Playing cards, 88 Lifting objects <4kg, 48 Lifting >4kg, 24 Exercise bike, 62 Home gardening, 48 Hunting, 0 Writing, 88 Swimming breaststroke, 3 Swimming crawl, 3 Holding a book to read, 74 Taking objects from tall shelves, 3 Using a personal computer, 80 Eating, 92 Putting on make-up, 75 Shaving, 90 Brushing teeth, 88 It should be pointed out that we only took patient disability or limitation in performing specific activities into account when they were unable to do so or failed to meet their expectations. This was based on their activity prior to the functional limitation that led to their surgical operation. Thus the fact that they did not voluntarily undertake a certain activity beforehand (such as “using a personal computer”) or did not do so for gender-based reasons (such as “putting on make-up”) was not understood to be a limitation.
- ∘
- -
Degree of muscular atrophy based on Goutalier's classification13 by means of preoperative magnetic resonance imaging study.
From discharge to the time the personal interview took place in outpatient surgeries, average patient follow-up was 53 months (48–72 months).
ResultsEpidemiological resultsThe average age of the subjects studied was 81 years old (76–89 years old), and 95% had retired from work. 88% of the patients studied were women, and in 73% of cases the dominant arm had been operated.
Clinical resultsAverage preoperative pain was 8.3 and average postoperative pain was 3.5. 76.7% of the patients required no pharmacological treatment whatsoever after the rehabilitation period, while only 10% needed analgesic medication (paracetamol, NSAID and/or metamizol) habitually due to their shoulder.
The average sex- and age-normalised preoperative for the whole series (116 patients) was 36%. The average postoperative figure was 80%.
The average Charlson index for the series was 1.69, which indicates a low comorbidity score.
Regarding joint balance, the pre- and post-operative values for anteversion, abduction and external rotation are shown in Table 2.
All of the patients were grade 3 or higher according to Goutalier's classification, when they were present in the evaluation of the subscapulus, teres minor and musculus infraspinatus using preoperative magnetic resonance imaging.
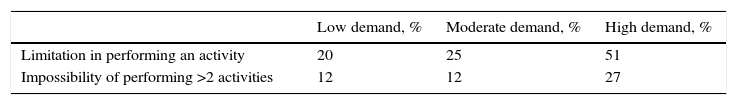
Table 1 shows the percentage of patients who performed the different degrees of low, medium and high functional demand activities. If all of these data are grouped according to degree, 20% of patients had some degree of limitation in performing low demand activities, 25% had some degree of limitation for moderate demand activities and 51% had some degree of limitation for high functional demand activities. On the other hand, 12% of the subjects were unable to perform more than 2 of the activities in the questionnaire within the low to moderate functional demand group; the corresponding figure for the high functional demand activities was 27% (Table 3).
Percentage of patients with limitations in performing an activity covered by the questionnaire or with impossibility of performing more than 2 activities according to the different degrees of functional demand.
| Low demand, % | Moderate demand, % | High demand, % | |
|---|---|---|---|
| Limitation in performing an activity | 20 | 25 | 51 |
| Impossibility of performing >2 activities | 12 | 12 | 27 |
Of all the low functional demand activities in our questionnaire, the patients stated that they found the greatest difficulty in unfastening their brassiere and scratching their back.
DiscussionIt is very well-known that medialising the centre of rotation of the implant in a reverse shoulder makes it possible to create a longer lever arm, which helps the deltoid muscle to perform shoulder anteversion and abduction, substituting part of the work of the rotator cuff when this is damaged.12,13 Nevertheless, shoulder rotations are poorly counterbalanced by the rest of the musculature when the infraspinatus and subscapulatus are damaged and are unable to anchor to the tuberosities around the implant.
Functional evaluation using questionnaires about the performance of everyday life activities following the implementation of RTSA is not a common subject in the literature. Publications which evaluate this technique in terms of joint balance and pain using different scales (chiefly the Constant–Murley and ASES scales) are somewhat more common.14,15
Of all the series that were revised, we only found one4 in which the indication for RTSA in all of the patients was arthropathy of the rotator cuff, as was the case in our series. In few of the other publications examined cuff arthropathy was the reason for implant in more than 50% of the patients in their series.2,3
Our activity questionnaire is inspired by the questionnaire which Cofield and his co-workers1,2 used to evaluate the everyday life activities that patients were able to perform after the implantation of a RTSA. However, this questionnaire was used for patients under the age of 65 years old for sport and everyday life activities in the U.S.A. This meant that it was hardly reproducible in our target population, so that we designed a new one. This was adapted to the more everyday activities in our area for patients with a substantially higher average age. We also classified activities according to their level of functional demand, given that for patients of this type it is important to also know the degree of independence that the prosthesis will give them.
Cofield carried out a comparative review of the functional results in patients with an average age of 62 years old (which is notably below that of our series) operated using hemiarthroplasty or RTSA, and concluded that both options clearly improve preoperative pain. On the other hand, his study shows that cases treated using RTSA achieve better results in terms of strength and mobility, while the patients are equally active in sports. When they are compared with our series, and in spite of the age differences, they show very similar results in terms of activity limitation according to functional demand: low (11%), moderate (33%) and high (56%), with an adjusted average constant of 81.2% and a fall of at least 5 points in the analogue visual scale.
The series presented by Fink Barnes et al.3 shows better analgesic control and that 60% of patients had a functional limitation. The latter was associated more with comorbidity (one of the main predictors for not restarting sports activity) than it was with the implant itself. Another factor which is known to compromise results is age. At above 70 years old it becomes harder to return to sports activities and those involving a high functional demand, as Gulotta et al. state, and which is corroborated by other recent publications.
Postoperative joint balance in our series shows satisfactory results in abduction as well as in anteversion. This agrees with the findings of the series by Cofield and Bigliani, with average results of 115° and 120°, respectively.
Nevertheless, we find that our surgical intervention does not give rise to major changes in external rotation. We know that retroversion of the humeral component influences the range of rotational movements of the RTSA, so that greater retroversion of the same leads to greater external rotation to the detriment of internal rotation.15 This circumstance did not arise in our series, given that in spite of using greater retroversion in implantation of the humeral component (30° in our case as opposed to the 20° used by the authors in their respective work groups), we obtained an average external rotation value of 10°, in comparison with almost 50° in the other series reviewed.
On the other hand, the activities which were limited the most often were those in which the glenohumeral joint has to move in internal rotation (unfastening your brassiere/scratching your back). This may be due to 2 factors (Fig. 1):
- -
The fact that the retroversion angle of the humeral component is increased restricts internal rotation, as we pointed out above.
- -
Residual subscapular dysfunction. The majority of our patients had grade III–IV rotator cuff arthropathy according to Hamada's classification,16 in which the subscapularis is affected in the context of massive breakage of the rotator cuff (Fig. 2). In the series of the American authors that were compared, the surgical procedure used a deltopectoral approach without reinsertion of the subscapularis in 80% of cases, with average internal rotation to S1.3 This may be associated with a poorer outcome, in spite of the published data which state that reinserting the subscapularis does not affect functionality after the implementation of a RTSA.17,18
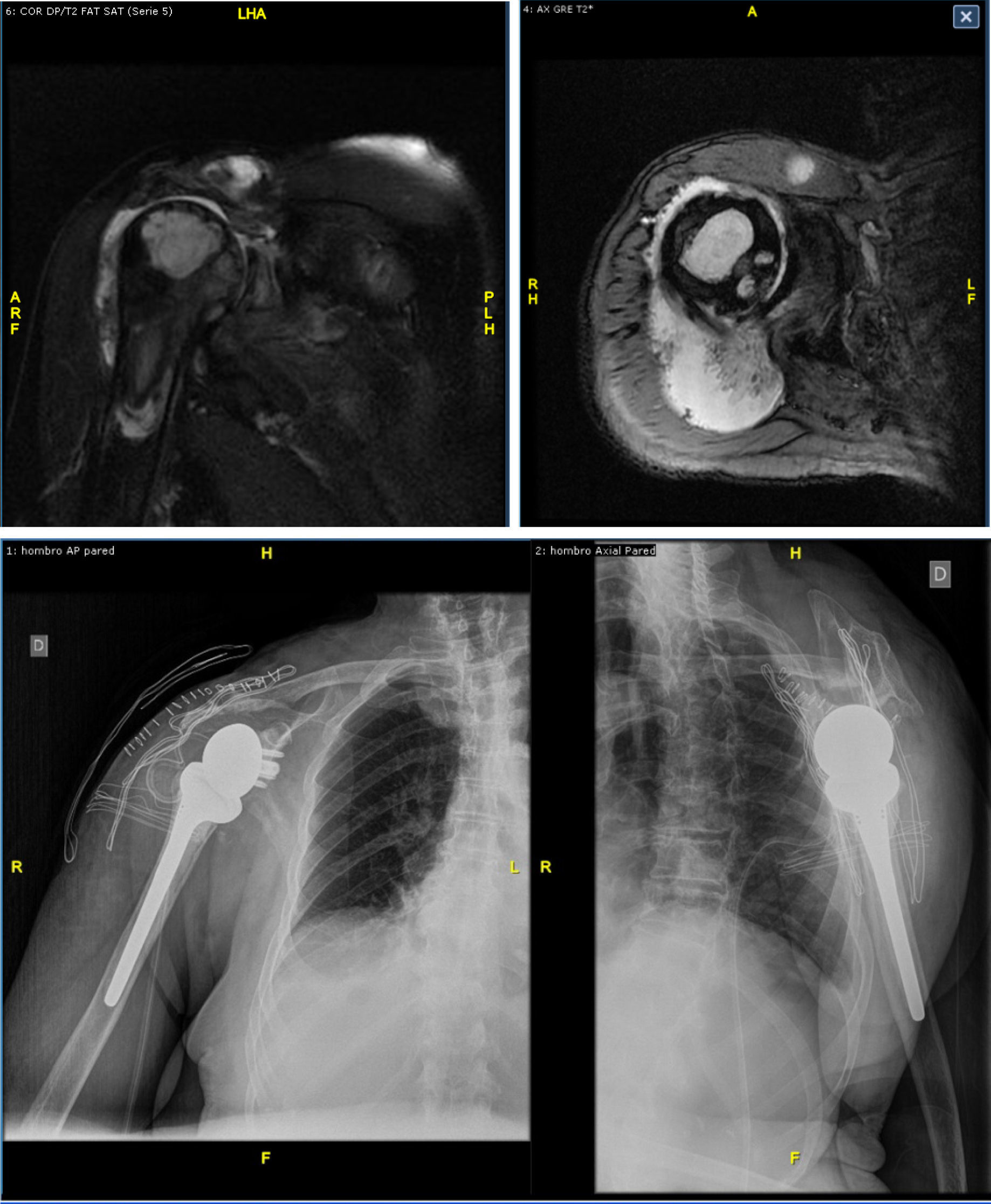
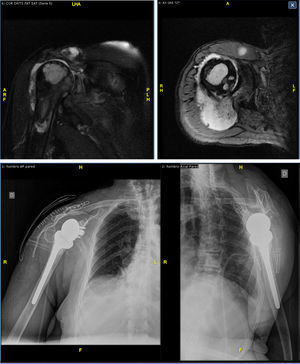
Figure 2.Top: 2 slices of magnetic resonance imaging prior to surgery, showing Hamada grade IV rotator cuff arthropathy with breakage and medial retraction to the acromioclavicular joint of the SE, major anterosuperior migration of the humerus head with large bone cysts and a large amount of intrajoint fluid, narrowing of the acromion, arthrosis of the acromioclavicular and glenohumeral joints. Bottom: X-ray result after RTSA implantation (Delta III-X-Tend Depuy-Synthes®).
(0.36MB).
The Charlson index, which is widely used in Gerontology, is important because it aids the surgeon to analyse subject survival when we have to resolve the risk-benefit balance of a surgical intervention.19–22
In our series the average score on the Charlson index was 1.69, which corresponds to low comorbidity in which a 26% mortality could be expected. This is far lower than the results obtained (7 patients, corresponding to associated risk data associated with a zero comorbidity index).
RTSA makes it possible to perform the majority of low and moderate functional demand activities in elderly patients, in spite of its functional limitations in the recovery of external rotation.
Study limitationsThese arise due to the limitations intrinsic to retrospective studies and the lack of uniformity in the parameters studied by the few series published in the current literature for the comparison of the results we obtained.
Conclusions- -
RTSA is a useful therapeutic option in the treatment of elderly patients with rotator cuff arthropathy. It is able to control pain and reduce or prevent the need to take analgesic medication.
- -
Although it improves the range of joint mobility in anteversion and abduction, this is not the case for external rotation when there is deterioration of the infraspinatus and teres minor tendons. This is because of the biomechanical nature of the implant itself.
- -
Good to excellent functional results are obtained in patients with a low comorbidity index.
- -
It is important that patients are aware of which activities will be more limited following the implantation of a RTSA so that they do not make high functional demands, given that otherwise we will be unable to satisfy their expectations.
Level of evidence III.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were undertaken in human beings or animals for this research.
Confidentiality of dataThe authors declare that no patient data appear in this paper.
Right to privacy and informed consentThe authors declare that no patient data appear in this paper.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Alcobía-Díaz B, Lópiz Y, García-Fernández C, Rizo de Álvaro B, Marco F. Actividades de vida afectadas en pacientes tras artroplastia total inversa de hombro en el contexto de artropatía de manguito rotador. Rev Esp Cir Ortop Traumatol. 2017;61:273–280.