To check the agreement of a preoperative digital templating, compared with the final result in the postoperative radiograph.
Material and methodThe study was carried out in 55 total hip prosthesis cases. A templating-software Neteous® (Socinser®, Gijón, Spain) was used. Agreement was measured using the Kappa Index for the stem offset or Lin Index for others variables: stem size, cup size, femoral neck length, and the distance from the centre of rotation of the femoral head to the lesser trochanter. The percentage of accurate hits was also described.
ResultsStem size: the exact success or error of only one size was of 61.6%. Quantitatively the Lin Index was 0.64 (substantial). Horizontal offset: satisfactory agreement was obtained (Kappa Index of 0.75). In 6 cases (10.90%) was changed to lateralised during surgery, for more joint stability. Size of the cup: the agreement obtained was 0.67 (substantial) with a hit grade of 43.6%. Prosthetic neck length: the exact hit or error of only one size were found in 50.9%, moderate level of agreement. Distance from the centre of rotation to the lesser trochanter: was observed for almost perfect agreement with Lin Index of 0.95. The exact percentage of hits or gap error less than 5mm was 74.5%.
Discussion and conclusionIn ours hands, the preoperative templating software analysed, has provided acceptable agreement rates, when compared with the postoperative result. But it takes more works verified by independent observers.
Comprobar el grado de concordancia de un sistema informático de planificación preoperatoria, en comparación con el resultado final en la radiografía postoperatoria.
Material y métodoSe analizaron 55 implantes de prótesis total de cadera. Se utilizó un programa informático de planificación comercializado Neteous® (Socincer®, Gijón, España). La valoración de la concordancia se realizó calculando el índice Kappa para el tipo de vástago o el índice de concordancia de Lin para el resto de medidas: talla de vástago y cotilo; cuello protésico; y distancia desde el centro de rotación a trocánter menor. También se describieron los porcentajes de aciertos.
ResultadosTamaño de vástago: el acierto exacto o con error de solo una talla fue del 61,6%; cuantitativamente fue un Lin de 0,64 (sustancial). Offset horizontal: se obtuvo una concordancia satisfactoria (índice de Kappa de 0,75). En 6 casos (10,90%) se cambió a lateralizado durante la cirugía, para obtener mayor estabilidad articular. Tamaño del cotilo: la concordancia obtenida fue de 0,67 (sustancial) con un grado de aciertos del 43,6%. Longitud del cuello protésico: los aciertos exactos o con error de solo una talla se hallaron en un 50,9%, nivel de concordancia moderada. Distancia del centro de rotación a trocánter menor: se apreció una concordancia casi perfecta con un Lin de 0,95. El porcentaje de aciertos exactos o con discrepancia inferior a 5mm fue del 74,5%.
Discusión y conclusiónEn nuestras manos el sistema informático de planificación preoperatoria analizado ha proporcionado índices de concordancia aceptables al compararlo con el resultado postoperatorio. No obstante, hacen falta trabajos que sean verificados por observadores independientes.
Preoperative planning is an action that should be routinely carried out in the total hip arthroplasty process. It identifies biomechanical, anatomical and surgery technique factors that are of great use during surgery so as to increase the functionality and longevity of the arthroplasty. The success of hip arthroplasty primarily depends on proper positioning of the components to optimise surgery results.1
Furthermore, preoperative planning allows for proper selection of component size, reduces the risk of intraoperative periprosthetic fractures, helps to restore overall offset (femoral and acetabular) of the hip and makes it possible to reduce the probability of lower limb length discrepancy and of prosthetic dislocation. In addition, planning makes components more readily available for the surgeon, thus minimising inventory costs.2
Presently, the preoperative planning system about conventional radiography, using acetate templates provided by commercial establishments, has become obsolete. The great majority of these templates have 15–20% magnification (seen as “normal” in conventional X-rays), which brings with it a significant margin of error.3 The inability to precisely determine the magnification of an X-ray is perhaps the biggest problem in preoperative planning, because conventional templates with pre-established magnifications make modifications or compensations imposible.4 Conn et al.5 found that classic preoperative planning coincided with component selection by only 69%.
In digital preoperative planning, the magnification measurements from both the templates and the digital X-rays can be unified. This led us to the hypothesis that upon using digital planning whose protocol includes digital X-rays, we would obtain a higher final agreement. This combination has the potential to eliminate errors associated with the manual manipulation of templates and X-rays.6
The objective of this study was to retrospectively test the degree of concordance of a digital preoperative planning system that assessed component size, as well as the horizontal and vertical offset of a total hip arthroplasty.
Methods and materialsA retrospective study was performed with patients who underwent cementless total hip arthroplasty between 2005 and 2011. With these patients, Neteous® software (Socinser®, Gijón) Spain was used for the preoperative planning. Osteoarthritis of the hip was the main diagnosis that motivated total prosthetic implantation. Patients were not included if they showed necrosis effects in the femur head, rheumatoid arthritis, fractures or effects from infectious or neoplastic processes. The objective was to obtain a homogenous group regarding the hip morphology.
All patients were operated on by a single senior surgeon at the hip unit in our hospital. Intervention was performed via lateral access modified by Hardinge.7 All prosthetics were the cementless PROSIC® model (Socinser®, Gijón, Spain).
Planning was performed sequentially, following protocols according to a technique developed by a surgeon in our unit, after his inclusion in the Neteous® programme (Socinser®, Gijón, Spain). This planning is further detailed below.
Step 1Radiography was performed using an anterior posterior (AP) view of the pelvis, centred on the symphysis pubis and on internal rotation of both hips. The general computer system of the hospital saved all the images in the standard Digital Imaging and Communication in Medicine (DICOM) format, in a storage system called PACS (Picture Archiving and Communication System).
The preoperative X-ray of the patient was captured in the PACS file and incorporated into the planning software. The same programme determined the degree of magnification or calibration. This was carried out by incorporating an external marker, of a known dimension, situated near the symphysis pubis between the patient's muscles at the moment of taking the X-ray. We used a marker called “hip scaler” (www.hipscaler.com).8 This allowed us to scale the X-ray size, in turn adapting it to the digital templates of the prosthetic components.
Step 2The centre of rotation of the healthy hip was located using a modifiable circle according to the size of the femoral head. If it had a prosthetic head, the same process could be used. For extremely deformed heads, the acetabulum could be used as a reference.
Step 3A line was drawn over the centre of the femoral medullary canal of the healthy femur (anatomical femoral axis), adjusting the upper end to the tip of the greater trochanter. This gave us information about the height to which the centre of rotation of the healthy hip could be found (centre of the circle drawn in the previous step) in relation to the tip of the greater trochanter.
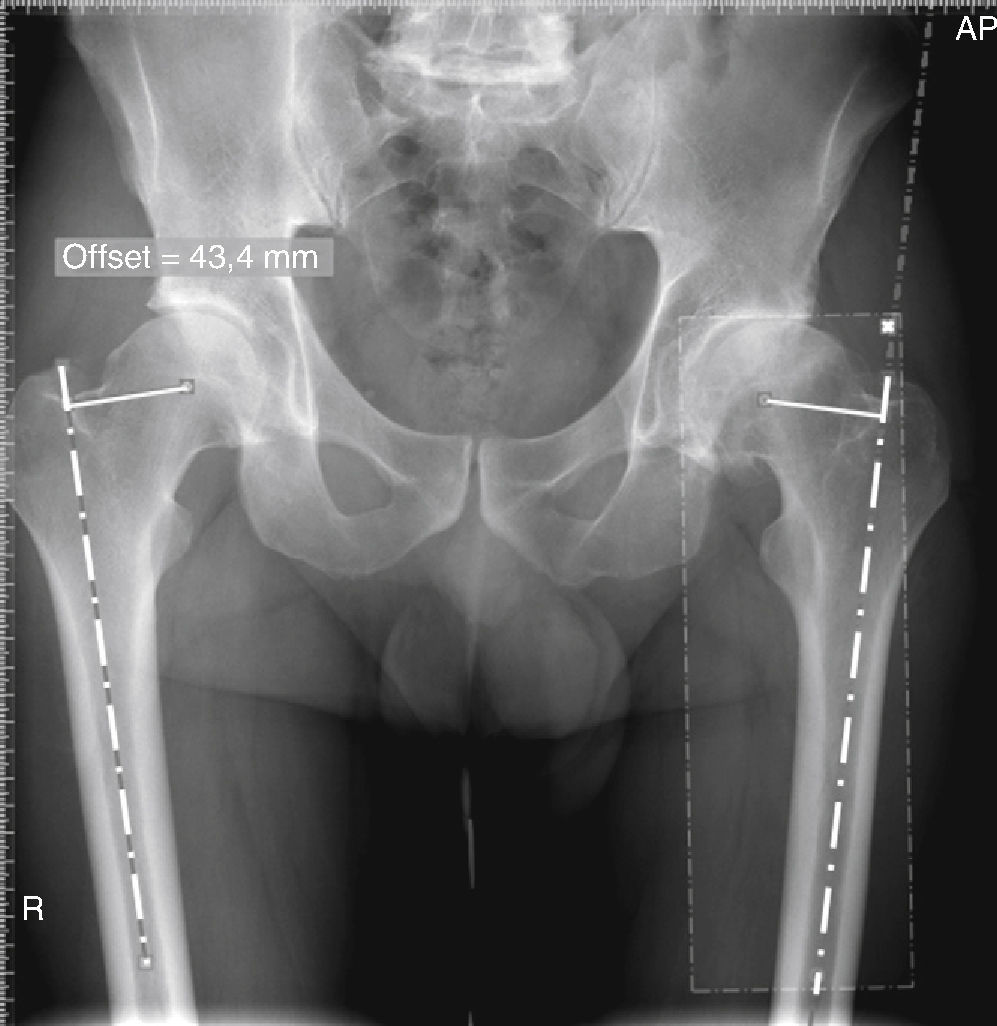
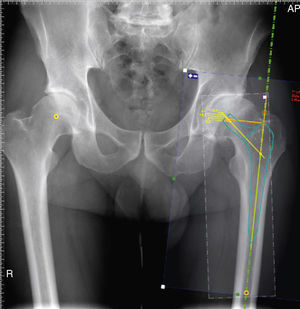
Step 4The horizontal femoral offset was measured (distance from the centre of hip rotation to the anatomical femoral axis) on the healthy hip. Next, the programme asked us to place a symmetry axis at the centre of the pelvis, with the objective of taking the measurements from the healthy hip and automatically extrapolating them for the fractured hip. This step required a final manual adjustment by the surgeon so that the references were placed exactly on the tip of the greater trochanter and the centre of the femoral medullary canal of the fractured hip (Fig. 1).
Once the X-ray magnification is calibrated, the data for the healthy hip are extrapolated for the hip to be operated on. Measurement of the horizontal femoral offset (distance from centre of rotation to the anatomical femoral axis) of the healthy hip (right hip in the figure). Extrapolation for the fractured hip (left hip in the figure). This step requires a final manual adjustment by the technician so that the references are placed exactly on the tip of the greater trochanter and on the centre of the femoral medullary canal of the fractured hip.
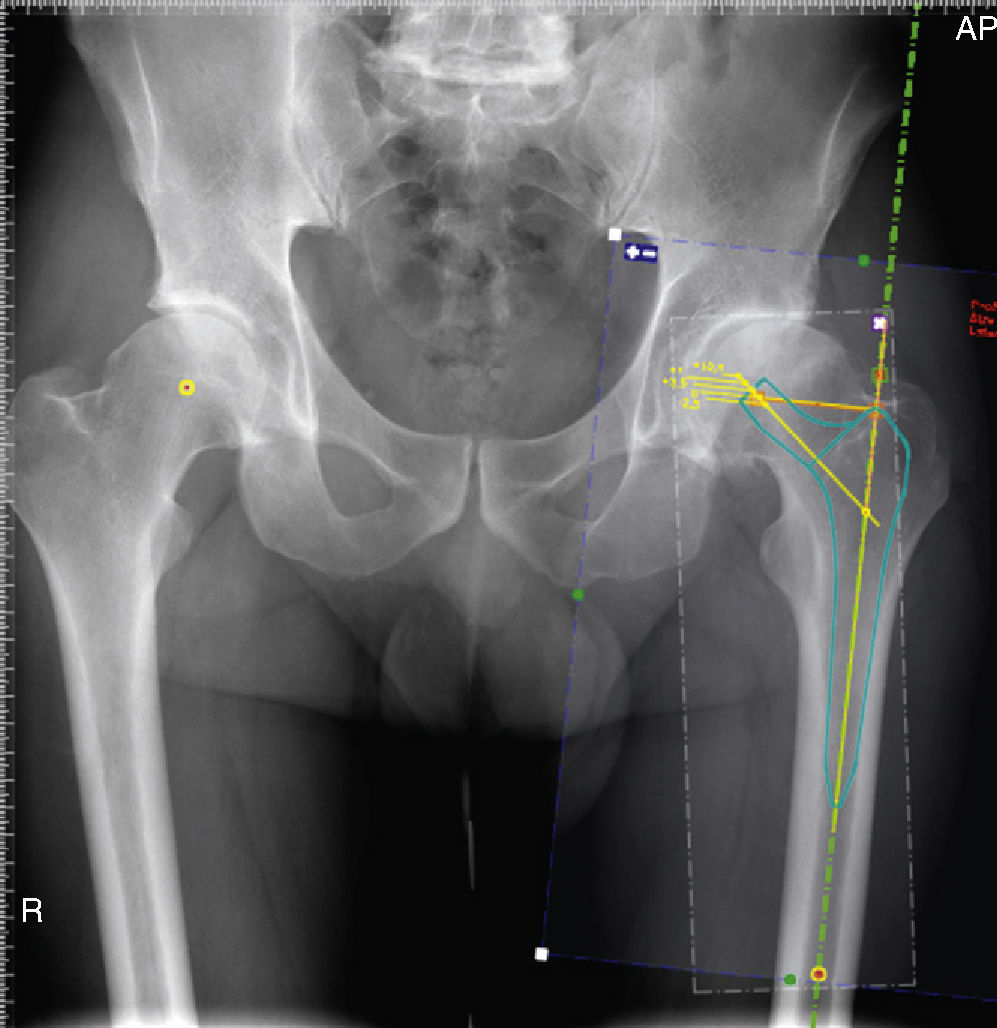
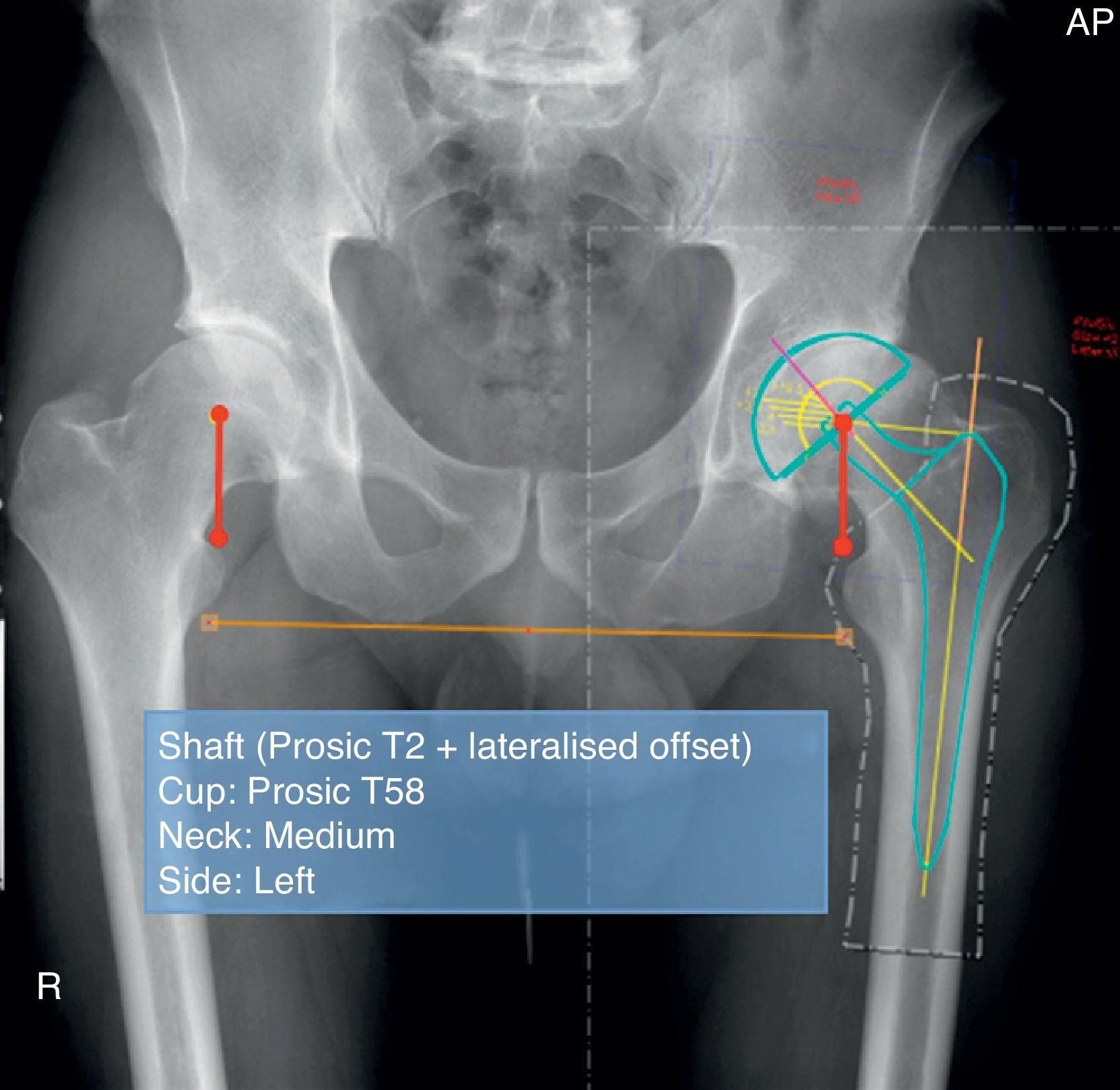
From the database of templates that the software provides, the desired stem was selected and placed on the anatomical bone shaft. The medium neck (neck 0) must coincide with the centre of rotation, adjusting size, horizontal offset and height with relation to the tip of the greater trochanter (Fig. 2).
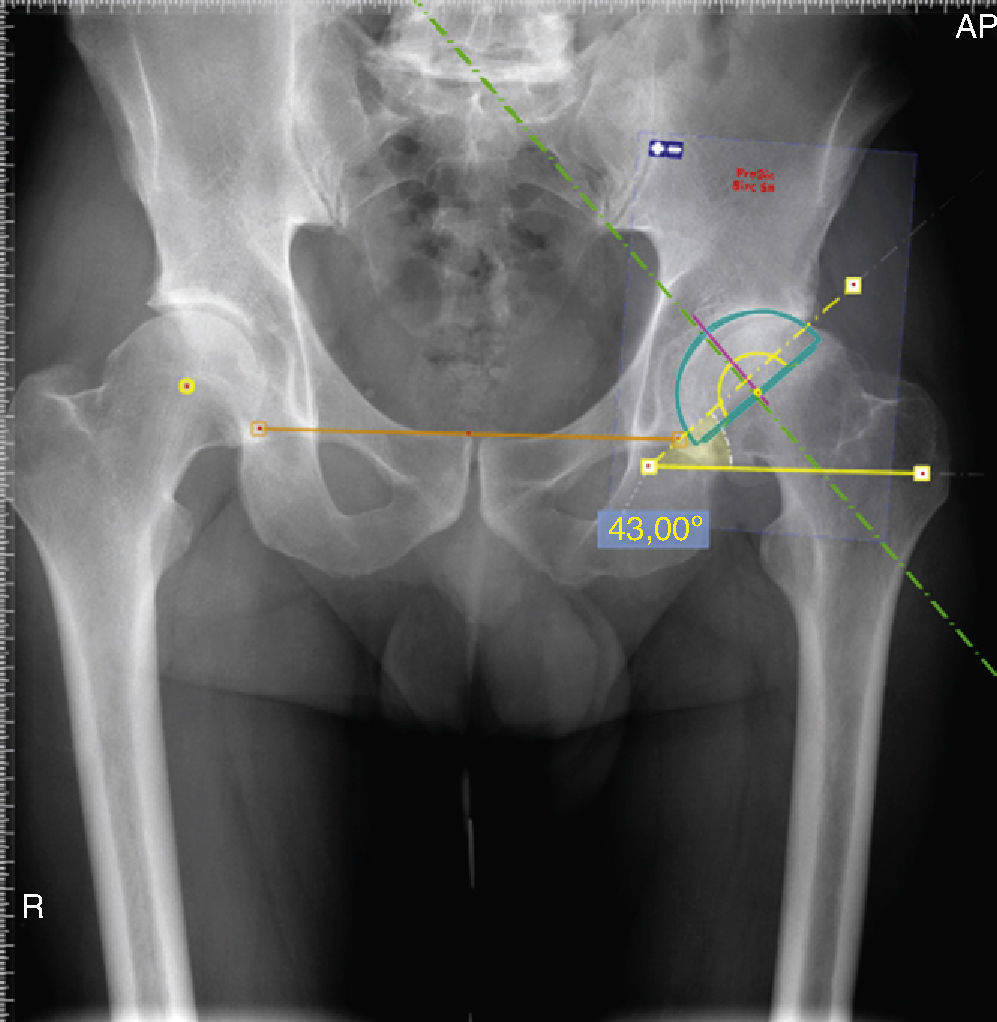
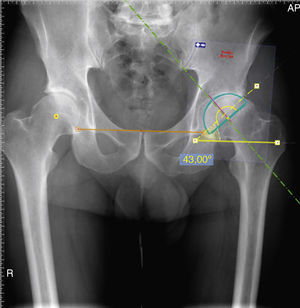
Step 6The bilacrimal line was traced (on the basis of the 2 Köhler's teardrop images) to orient the transversal pelvic axis and have a reference pattern for comparing lower limb length. If these teardrop images were not identified, the ischial tuberosities or the obturator foramen could be used. However, the measurement could be less exact in these cases, depending on the quality of the x-ray projection. This transversal axis was used to calculate the desired incline (or abduction) angle of the acetabular cup component, placing the implant template in an appropriate position with respect to the pelvis and the acetabular background (Fig. 3). At the same time, the cup size could also be determined.
Planning for the acetabular cup component (size and incline angle adjustment). The transversal axis is used to calculate the desired incline (or abduction) angle of the component, placing the implant template in the proper position with respect to the pelvis and acetabular background.
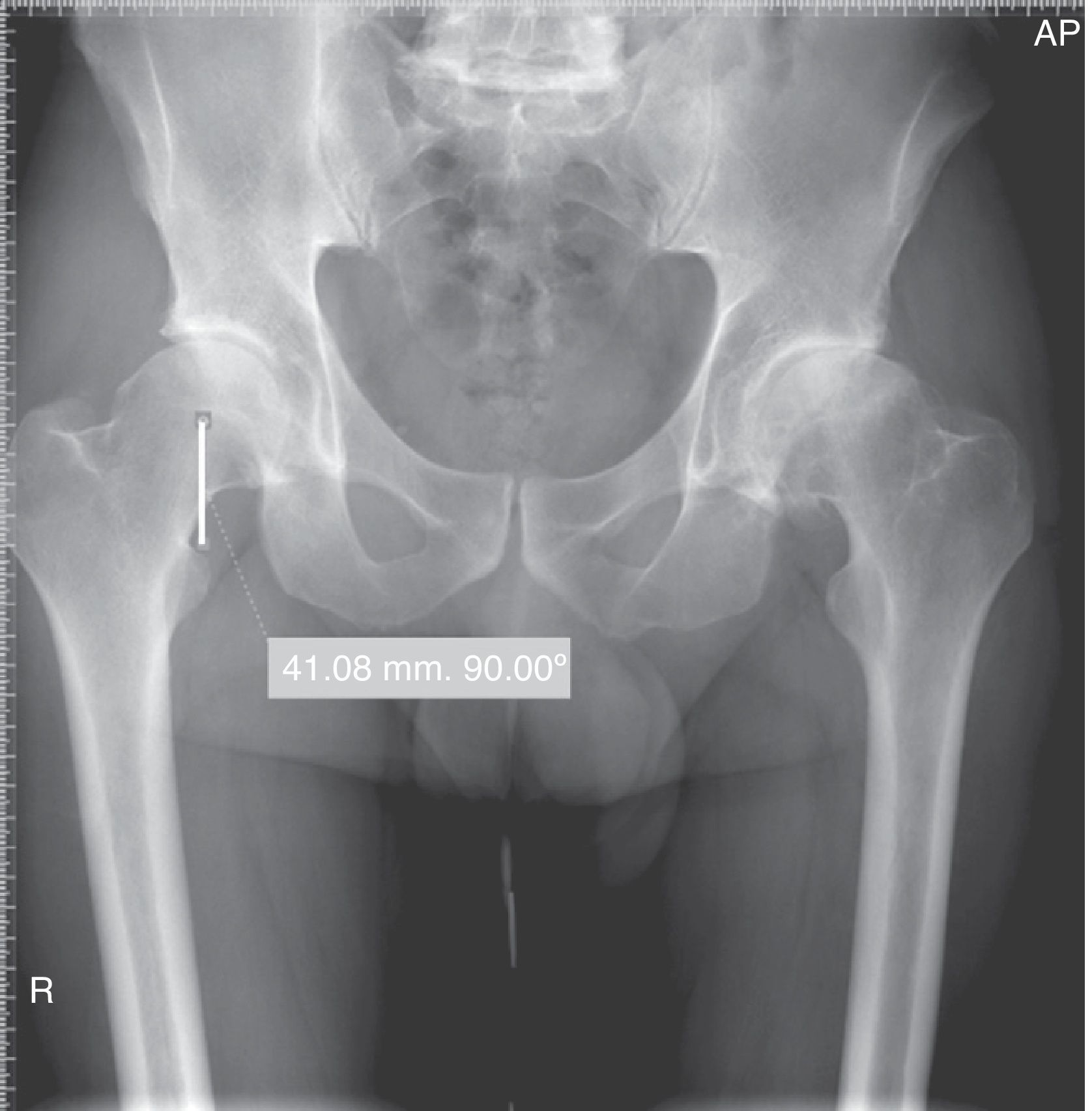
The distance was measured from the centre of rotation to the upper part of the lesser trochanter on the healthy hip (Fig. 4). For the hip that is to be operated on, this length measurement should be exact, to avoid leg length differences.9
Step 8The software allowed the planned femur-shaft set to be cropped and positioned by simply sliding it in a way that the centre of rotation-lesser trochanter distance coincided with the healthy hip measurement. According to each case, the size of the prosthetic neck should be modified if increasing or decreasing limb length is needed.
Step 9Planning text was added, noting the stem type, its size, the offset to be used (standard or lateralised), cup type and size, neck size and laterality of the surgery, as well as the patient's name, if desired (Fig. 5). With this step, planning was finalised.
After the surgery, to study the degree of concordance, an AP X-ray of the pelvis was taken in the same way as the preoperative X-ray. With this, using the same planning software, the following variables were assessed: (1) size of the components, for both the cup and the stem; (2) horizontal offset (standard or lateralised neck); (3) length of the neck per se; and (4) distance between the centre of rotation and the part closest to the lesser trochanter. For this last measurement, an error margin of ≤5mm was accepted. This was because, in our opinion, small changes in the beam incidence on the pelvis when taking the X-rays (pre- and postoperative) can cause false variations in the distance measured.
For the statistical treatment of the results, analyses were performed with SPSS® v18 for Windows (SPSS® Inc., Chicago, IL, USA) and the level of confidence was determined at 95% for the confidence intervals (CI).
The results were presented as mean±standard deviation (SD) or absolute frequencies and percentages for quantitative or qualitative data, respectively. Evaluation of agreement between both offset assessments was performed using Cohen's Kappa,9 as it evaluated a dichotomous variable. The main agreement assessment among the rest of the quantitative determinations was performed using Lin's10,11 concordance correlation coefficient (CCC) and its corresponding CI at 95%, to quantify the degree of agreement and magnitude of precision between both values. Lin's CCC measured the degree of agreement and the precision with which both values differed from a regression line that expressed perfect concordance. This line passed through the coordinates (0,0) and was at a 45° angle, which implied an incline equal to 1. Values closer to 1 on this index implied nearly perfect agreement and precision, while values closer to 0 implied imprecision and/or lack of agreement.
The level of agreement was interpreted using the following grading scale: 0: poor; 0–0.2: slight; 0.21–0.40: reasonable; 0.41–0.60: moderate; 0.61–0.80: substantial; and 0.81–1.00: nearly perfect.
ResultsData were obtained from a total of 55 patients who underwent a total hip replacement operation during the study period. The gender distribution consisted of 22 women (40%) and 33 men (60%). The mean age at the moment of intervention was 63 years (range 26–84). The patients showed a mean body mass index of 28kg/m2 (range: 18.99–41.40).
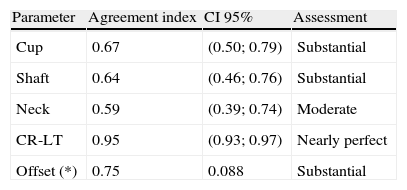
The levels of agreement reached between preoperative planning and X-ray assessment after surgical implantation of the prosthetic are shown together in Table 1. Each of the variables studied is analysed below in greater detail.
The value obtained for Lin's CCC was 0.64 (CI 95%: 0.46–0.76), which gave us a substantial agreement level. In 27 cases (49.09%), the exact number was correct. Despite this, another 9 cases (16.36%) presented a size above or below the planned measurement. We observed a tendency to place stems that were larger than the size provided, with a mean of 0.9. The standard deviation was 3.27. This last value also represented the margin measurement within which most stems were placed.
Stem type in relation to horizontal offsetRegarding horizontal offset, because it is a dichotomous variable (standard or lateralised offset), a Cohen's Kappa value of 0.75 was obtained (standard error: 0.088). In 31 cases (56.36%), lateralised stems (high offset) were planned and placed as such. In another 17 cases (30.90%), the use of standard stems was planned and successful. In 6 cases (10.90%), the switch was made to lateralised stems during surgery upon considering that they provided more joint stability. In 1 case, the change was from lateralised offset to standard offset, after observing excess tension in soft parts during the surgery. Therefore, the agreement index was satisfactory in relation to the offset type.
Cup sizeRegarding cup size, the value for Lin's CCC was 0.67 (CI 95%: 0.50–0.79), which showed substantial agreement, according to the grading table. Of all the cases, 24 (43.63%) measurements were correct and 14 (25.45%) planned for a size above or below that implanted.
Length of prosthetic neckFor the prosthetic neck length used, the value for Lin's10 CCC was 0.59 (CI 95%: 0.39–0.59), which indicated moderate agreement. Correct measurements were found in 29 cases (52.72%). There were 28 cases (50.90%) in which the size of the implanted neck had a variation of at least 1 size above or below the planned measurement. In the other 3 cases, variation was equal to or higher than 2 sizes.
Distance from centre of rotation to lesser trochanterFinally, Lin's CCC was used to evaluate the distance between the centre of rotation of the prosthetic hip and the upper edge of the lesser trochanter, which was the measurement that determined the difference in length between the 2 femurs. We obtained an index value of 0.95 (CI 95%: 0.93–0.97), which indicated nearly perfect agreement. Correct measurements between what was planned and the postoperative result were obtained in 42 cases (76.36%). In this measurement, variations equal to or less than 5mm were accepted as valid.
DiscussionDifferent commercialised computer programmes can be found for the digital planning of a total hip replacement. The programme used in this study, Neteous® (Socinser®, Gijón, Spain), and the technique we developed provide the surgeon with an organised prevision of the prosthetic inventory needed during surgery, as well as the special biomechanical and anatomical parameters for each case. These measurements, carried out before the surgery itself, constitute a crucial step for the success of the arthroplasty.
Some authors6,13,14 demonstrated that classic preoperative planning, on conventional X-rays and using acetate templates, resulted in more correct measurements regarding component size and was quicker in its execution, compared to digital planning systems. However, these authors were unable to explain the cause of this finding. Nonetheless, in the last few years and in most hospitals around the world, the tendency is to perform planning with digital tools and X-rays, for economic reasons.12
We know that the magnification of a simple X-ray image of the pelvis is a constant and depends on the distance (always variable) between the skeleton of the patient and the X-ray film. For this reason, regardless of the planning system, we need to introduce a radio-opaque object of a known measurement (calibrator) onto the film when taking the X-ray. In our study, the “hip scaler” calibrator was used, its validity demonstrated by Wimsey et al.8 These authors, however, placed the apparatus alongside the greater trochanter. We placed it proximally between the patient's thighs, to support the calibrator. This imitated the system Crooijmans et al. advocated,4 in which they placed it at the pubic level. The prevalence levels of success in the Crooijmans study and in ours were very similar, confirming the reliability of the method proposed.
To use any planning tool within a surgical procedure, its main characteristic should be reliability. To analyse the precision between what was planned and what happened, we used Lin's10 CCC for quantitative variables. However, in the case of offset assessment, as it was a dichotomous variable, analysis was performed using Cohen's9 Kappa agreement index. In general terms, index values closer to 1 imply nearly perfect agreement and precision, while values closer to 0 imply a lack of agreement and/or imprecision.
The values obtained were: 0.64 for correctness in shaft size; 0.67 for that of cup size; 0.59 for the neck length used; 0.95 for the distance from the centre of rotation to the lesser trochanter (vertical offset); and 0.75 for the horizontal offset. Considering these results, the agreement indexes seem unfavourable, excluding that of vertical offset. However, upon analysing the measurements closely, 65.45% were correct or presented a margin of error that was less than 2 sizes for the femoral component. The same thing occurred with cup size, where 69.08% were measured correctly or varied by only 1 size above or below what was expected. In our opinion, varying by 1 size during surgery indicates that size of the planned components should not have great repercussions in the final result. Furthermore, in each case, it would depend on the bone quality and the condition of the tool used to prepare that bone. Iorio et al.6 found that analogical planning (classic) for the femur was successful (using 1 size more) in 77%, and in 74% if digital planning was performed, also with 1 size more. Regarding the cup, it was found that 78% of the analogical cases presented correct measurements compared to 60% of the digital cases, both with the caveat of allowing the use of 1 size larger or smaller.
González Della Valle et al.14 found that exact stem size agreed in 69% of cases when planning was done analogically, and in 98% when a 1-size margin of error was assumed, whether it was 1 size larger or smaller. Digital planning showed a 58% success rate compared to a 94% success rate when a 1-size variation was permitted.
Regarding the cup, the same author found that exact component measurement was taken analogically in 51% of the cases, and digitally in 25%. If 1 size larger or smaller was permitted for these values, the rates of correct measurement climbed to 97% and 81%, respectively. Our results also showed this increase in agreement for the method we present if this 1-size variation is allowed. Other authors also accept a digital planning system as very useful, with a margin of error of 1 size larger or smaller.15
What indeed affects the biomechanical performance of the hip is the degree of lateralisation or medialisation given to the centre of rotation of the hip and the final limb length, in comparison to that of the healthy side. In our study, in relation to the degree of lateralisation of the femoral axis (horizontal offset), stem type showed a high percentage of correct measurements: all cases except 7. In 6 of these, the surgeon opted to widen the planned shaft laterality to improve hip stability. In the other case, the surgeon opted to reduce the laterality to improve the tensional balance of the soft periprosthetic parts. This situation was due to excessive medialisation of the acetabular component (increase in acetabular offset). Agreement in femoral shaft offset was satisfactory.
For González Della Valle et al.,14 the distance between the centre of rotation and the upper part of the lesser trochanter showed a difference of 2mm (in manual planning) in 66% of the cases, and a difference of 5mm in 14% of the cases. These results were not statistically significant. Our series showed a lower level of agreement (76.36%). It seemed that the distance was subject to a certain margin of error, due to the possibility that the X-rays compared (preoperative and postoperative) may have had different beams of incidence on the patient's pelvis.
With respect to limitations in our study, we can say that during the surgical intervention, the risks of undersizing or oversizing the prosthetic components were assumed according to the bone quality perceived by the surgeon, and no effort was made to comply with what was planned. The final decision on prosthetic component size was made intraoperatively, according to the surgeon's judgement at that moment. It was also assumed that this was the best option. In addition, we did the planning on just a single X-ray projection of the pelvis (AP) and the axial or lateral projections were not considered. Another limitation is that the surgeons or the institutions where their healthcare activity is performed need to buy planning software and cover its economic cost.
Results in the literature continue to show greater certainty and greater predictability in analogical planning methods. However, the universal tendency is to carry out digital planning for cost-benefit and surely cost-effectiveness reasons, which have yet to be tested. What is known is that digitally planning a hip arthroplasty involves no risk for the patient6; this is because, in the end, what prevails is the surgeon's judgement at the moment of the intervention, with the plan being a helpful guideline.
In general, preoperative planning in a total hip arthroplasty is accepted as absolutely necessary as it provides relevant information for a successful implant. Given that magnification of the X-ray image can vary considerably from 1 patient to the next, the use of a calibrating device is unquestionable.
In conclusion, we can say that the preoperative planning method proposed, using Neteous® software (Socinser®, Gijón, Spain), has shown acceptable (substantial) agreement indexes in relation to the postoperative X-ray result. However, further studies evaluated by independent observers are necessary.
Ethical responsibilitiesHuman and animal protectionThe authors declare that no experiments were performed with humans or animals for this study.
Data confidentialityThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors have no conflict of interest to declare.
Please cite this article as: Gallart X, et al. Estudio de la concordancia de un sistema de planificación preoperatoria digital en artroplastia total de cadera. Rev Esp Cir Ortop Traumatol. 2012;56:471–7.