Chronic low back pain is a common cause of medical consultation, and is often associated with degenerative vertebral disease. Despite this, we must not forget other diseases even in those cases where the imaging tests may suggest chronic degenerative changes in the lumbar spine, including the possible presence of an abdominal aortic aneurysm with a contained rupture must be ruled out due to its prognostic and therapeutic implications.
We present 5 cases of chronic low back pain associated with serious lytic lesions in the vertebral body due to chronic rupture of an abdominal aortic aneurysm.
El dolor lumbar crónico es una causa habitual de consulta médica y se relaciona en muchas ocasiones con la enfermedad vertebral degenerativa. A pesar de ello no debemos olvidar otras enfermedades incluso en aquellos casos en los que las pruebas de imagen preliminares sugieran cambios degenerativos crónicos en la columna lumbar, y la posible presencia de un aneurisma de aorta abdominal con una rotura contenida debe ser descartada por sus implicaciones pronósticas y terapéuticas.
Presentamos 5 casos de dolor lumbar crónico asociado a lesiones líticas graves del cuerpo vertebral debido a rotura crónica contenida de un aneurisma de aorta abdominal.
Except for those with an inflammatory origin, patients with intact abdominal aortic aneurysms are generally asymptomatic and diagnosis is often an incidental finding whilst obtaining radiographs for a different reason. In some circumstances, particularly when the aneurysms have a large diameter, they may compress adjacent organs or structures and cause symptoms. Although rare, chronic contained rupture of an abdominal aortic aneurysm can result in the partial destruction of the vertebral body. This can be associted with chronic low back pain, and, eventually, distal neurological deficit.
The aim of this work is to emphasise the importance of some atypical presentations of abdominal aneurysmal disease, capable of simulating chronic diseases with a traumatic or rheumatic origin, as well as the need for an accurate diagnosis and prompt treatment.
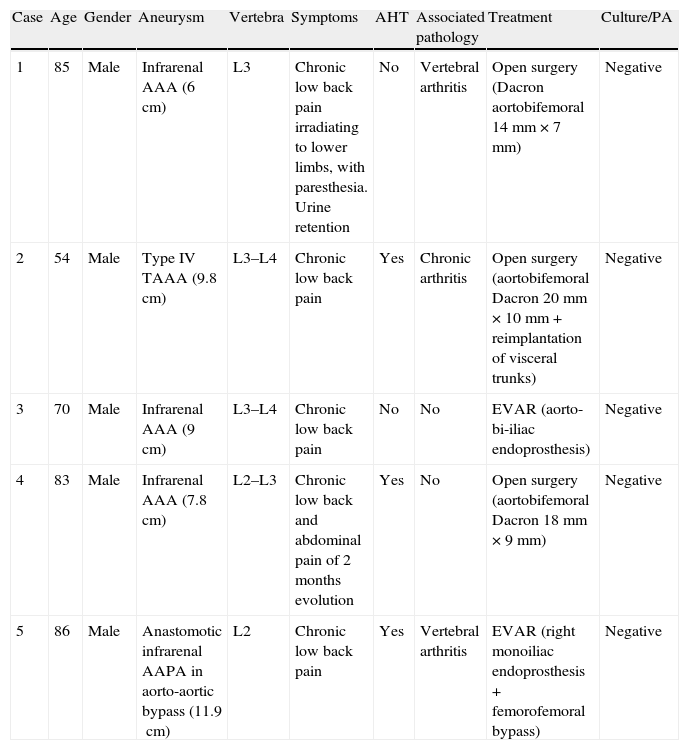
Case reportsBetween 1988 and 2011 there were 5 cases of chronic low back pain associated with severe, lytic lesions of the vertebral body due to a chronic, contained aortic aneurysm rupture at the abdominal level (Table 1). All 5 patients were males and their ages were between 54 and 85 years (mean age of 70 years). All suffered chronic back pain as their main symptom, although 1 patient also reported abdominal pain of 2 months evolution and 1 reported paresthesia and irradiation from the lower back to both lower limbs, as well as urine retention. Three of the patients presented hypertension and 2 suffered associated symptomatic vertebral arthritis.
| Case | Age | Gender | Aneurysm | Vertebra | Symptoms | AHT | Associated pathology | Treatment | Culture/PA |
| 1 | 85 | Male | Infrarenal AAA (6cm) | L3 | Chronic low back pain irradiating to lower limbs, with paresthesia. Urine retention | No | Vertebral arthritis | Open surgery (Dacron aortobifemoral 14mm×7mm) | Negative |
| 2 | 54 | Male | Type IV TAAA (9.8cm) | L3–L4 | Chronic low back pain | Yes | Chronic arthritis | Open surgery (aortobifemoral Dacron 20mm×10mm+reimplantation of visceral trunks) | Negative |
| 3 | 70 | Male | Infrarenal AAA (9cm) | L3–L4 | Chronic low back pain | No | No | EVAR (aorto-bi-iliac endoprosthesis) | Negative |
| 4 | 83 | Male | Infrarenal AAA (7.8cm) | L2–L3 | Chronic low back and abdominal pain of 2 months evolution | Yes | No | Open surgery (aortobifemoral Dacron 18mm×9mm) | Negative |
| 5 | 86 | Male | Anastomotic infrarenal AAPA in aorto-aortic bypass (11.9cm) | L2 | Chronic low back pain | Yes | Vertebral arthritis | EVAR (right monoiliac endoprosthesis+femorofemoral bypass) | Negative |
AAA: abdominal aortic aneurysm; AAPA: abdominal aortic pseudoaneurysm; AHT: arterial hypertension; EVAR: endovascular aortic aneurysm repair; PA: pathological anatomy; TAAA: thoracoabdominal aortic aneurysm.
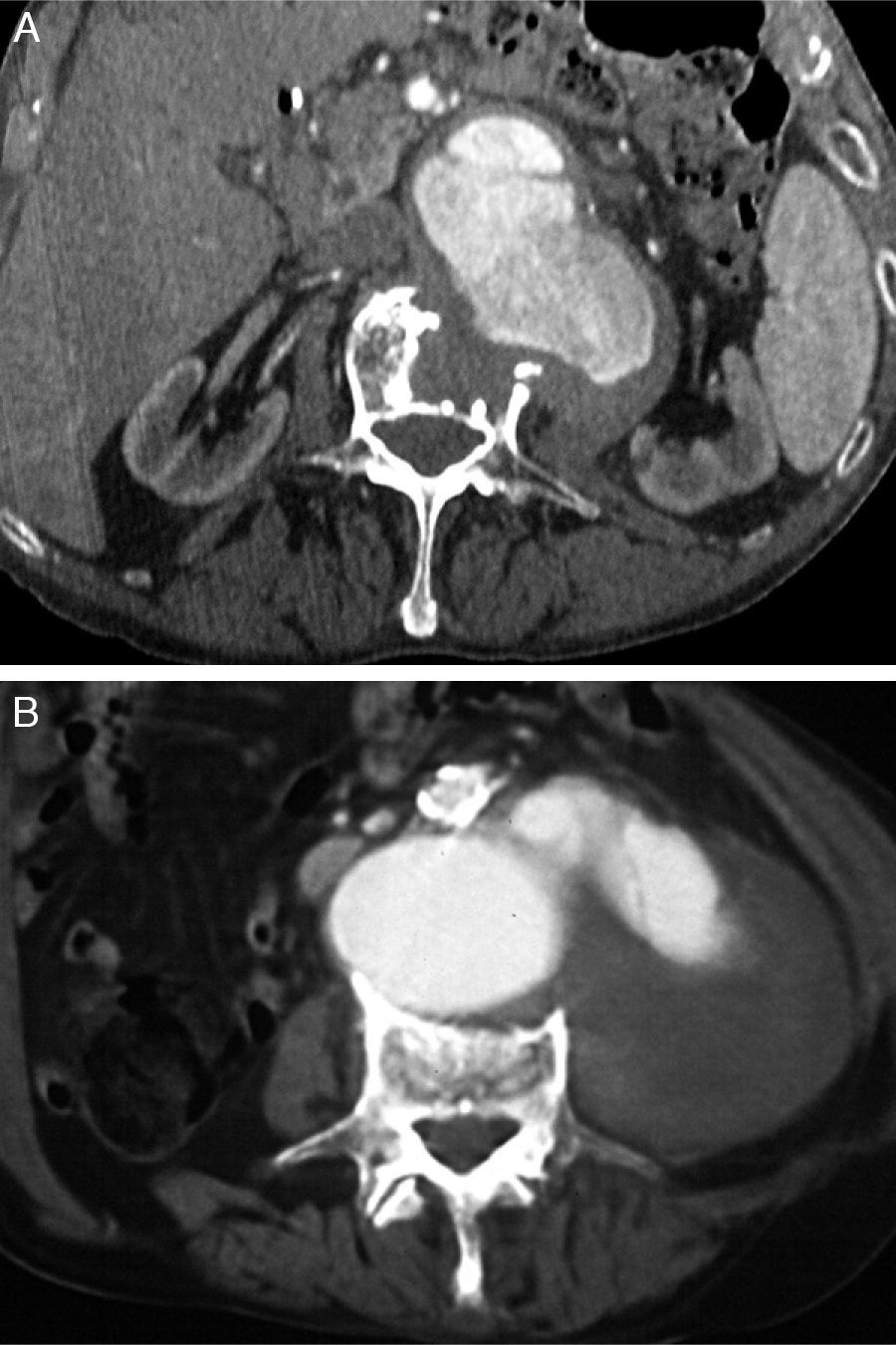
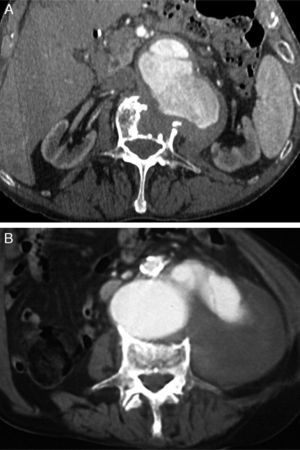
Three cases presented simple, infrarenal, abdominal aortic aneurysms and 1 case was a complex, thoracoabdominal aneurysm of type IV in the Crawford-Safi classification. One last patient presented an anastomotic pseudoaneurysm in relation to a previous aorto-aortic bypass performed 7 years earlier due to an infrarenal, abdominal aortic aneurysm with no complications. The maximum diameters of the aneurysms were within the range of 6–11.9cm, with a mean size of 9cm. The contained haematoma caused lysis of the anterior or anterolateral side of the lumbar vertebral bodies between L2 and L4, with the third lumbar vertebra being the most frequently affected in our series (Fig. 1).
Treatment consisted of an aortobifemoral bypass with Dacron prostheses of different diameters according to the individual anatomy of each aorta, except in 2 patients in whom endovascular treatment was carried out, with implantation of an aorto-bi-iliac, Excluder® type endoprosthesis and an aorto-monoiliac endoprosthesis associating a femorofemoral bypass. In the case of the complex thoracoabdominal aneurysm it was also necessary to reimplant the renovisceral trunks on the body of the prosthesis. The results of the anatomopathological studies and aortic wall cultures were negative in all cases, thus ruling out inflammatory or infectious causes.
Technical success was obtained in 100% of cases, with no perioperative mortality and only requiring reoperation in 1 case due to migration of the iliac branch of the stent 6 years after endovascular repair. The mean follow-up period was 25 months, with a range of 7–72 months. Although 2 patients died during follow-up, neither death was associated with aneurysmal disease.
DiscussionLow back pain is a common reason for medical consultation and its origin is rarely associated with diseases posing a direct risk to the life of patients. Nevertheless, occasionally it may represent the first warning sign of a more serious condition, such as a ruptured abdominal aortic aneurysm. At present, the acute presentation of the disease carries a high mortality rate, reaching 50% among patients who receive urgent surgical treatment1 despite new lines of research on endovascular therapy. The determining factor in the survival of this disease is the type of aneurysmal rupture, as suggested by the fact that a significant number of these patients will die before reaching the hospital due to free intraabdominal bleeding.
In 1965, Szilagy et al.2 introduced the concept of contained, abdominal aortic rupture for those cases in which the rupture occurred towards the posterior side of the vessel and adjacent structures sealed the exit point, causing symptoms of nonspecific lumbar or abdominal pain during a variable period in which patients may present lower limb neuropathy and even paraplegia when the vertebral bodies are eroded by pulsating blood flow.3 At other times, peripheral neuropathy is caused by the retroperitoneal haematoma, mainly affecting the femoral nerve. This atypical presentation can simulate a variety of diseases, including bone metastases, primary bone tumours, rheumatoid arthritis, osteomalacia or infectious processes, such as spinal tuberculosis (Pott's disease), pyogenic spinal spondylitis and psoas abscesses. Direct pressure on the iliohypogastric or ilioinguinal nerve would be the cause of pain radiating towards the inguinal and lower abdominal region, testis and anterior thigh. The lateral femoral cutaneous nerve or femoral nerves are affected less often.4
The prevalence of chronic, contained ruptures of abdominal aortic aneurysms is not known precisely, but is estimated at around 4% of all ruptured aortic aneurysms. Within this group, retroperitoneal haematoma can result in vertebral erosion in up to 30% of cases.5
The pathogenesis of spinal lysis could be explained by the intermittent pressure of the arterial pulse wave exerted by the aneurysm on the body of the vertebra. Likewise, other, more complex mechanisms have been contemplated which may be somewhat interrelated, such as ischaemic necrosis due to occlusion of lumbar arteries or inflammatory and/or infectious processes affecting the vertebral body.6,7 However, most reported cases of vertebral erosion associated with abdominal aortic aneurysms are caused by the chronic, contained rupture of non-infectious aneurysms. Although 1 case of Behçet's disease has been identified as subjacent disease,8 these are usually nonspecific aneurysms.
Chronic contained rupture should be considered in the differential diagnosis of patients with low back pain, even in those cases with a previous history of arthritis-type pain, as reflected in our series. It is important to emphasise the need for a detailed physical examination when lower back pain is significant, including abdominal palpation in search of a pulsating mass. In addition to an anteroposterior column radiograph, we must also obtain images in the lateral projection or else erosion on the anterior side of the vertebral body could be overlooked. The differential diagnosis should take into account the fact that vertebral lysis caused by a contained aneurysm is generally more homogeneous than that caused by pyogenic spondylitis, in which the lytic process margins are irregular and poorly defined.9 Confirmation of the diagnosis is obtained by computerised tomography (CT) or magnetic resonance imaging (MRI) scans capable of revealing the contained aortic aneurysm eroding the vertebral bodies. The information provided by arteriography, although sometimes useful, is not essential and is subject to the individual characteristics of each case (aneurysm affecting renal or visceral arteries, hypertension, peripheral arterial disease, etc.).
Although an infectious origin should be taken into account, its confirmation can be difficult if there are no signs of collection or gas, even intraoperatively. In such cases, in addition to cultures of samples from the wall and adjacent areas, an anatomopathological examination of tissues can be useful when an inflammatory infiltrate of polymorphonuclear leukocytes is confirmed.
Typically, these patients are haemodynamically stable for extended periods of time. Moreover, although the natural history of patients with chronic contained rupture of an aortic aneurysm is not well-known, it seems that most cases progress to complicated ruptures, requiring emergency surgery if this is not repaired previously. For this reason, although they enable a better surgical planning than acute rupture of an aneurysm, once the diagnosis is confirmed the recommendation is to operate without delay. In the case of elderly patients or patients with poor general health but with propitious anatomy, endovascular repair may represent a solution, as long as there are no signs of infection present, such as sepsis, abscesses or gas. In all other cases, classical open surgery should be the first choice.
Evolution after repair of these aneurysms is usually positive, with complete cessation of symptoms and early morbidity and mortality similar to that of repair of standard abdominal aortic aneurysms. Nevertheless, the recorded long-term survival is somewhat lower (64.4% vs 84.4% at 5 years, respectively).10
In summary, chronic contained rupture of an abdominal aortic aneurysm should be ruled out in patients with low back pain of unknown aetiology, even in those cases in which patients report chronic pain and the initial tests suggest degenerative changes in the spine. A lateral radiograph of the lumbar spine is key to the diagnosis, which must be confirmed by a CT or MRI scan. Before operation, diagnosis tests for infection should be performed, although surgical treatment must be carried out without delay. Endovascular repair can be considered as a safe treatment option whenever the anatomy is favourable and there is no presence of gas, abscesses or septic status. In the remaining cases, open surgery is recommended.
Level of evidenceLevel of evidence IV.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: González Gay M, et al. Erosión vertebral en aneurismas de aorta abdominal como causa de dolor lumbar crónico. Serie de 5 casos. Rev Esp Cir Ortop Traumatol. 2012;56:478–81.