Complications related to anticoagulant therapy have been widely described, although tension haematomas in the extremities are frequently undervalued, and commonly considered banal pathologies.
Material and methodRetrospective descriptive study between 2014 and 2017, including patients with limb haematomas after minimal trauma related with anticoagulant therapy, and surgically treated by Traumatology.
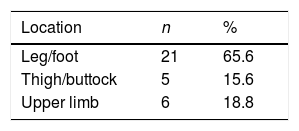
Results32 cases were eventually included, 81% were women, average age of 83.56 years, and a mean aCCI of 5.97. Anatomical location of haematomas was 65.6% in leg/foot, 15.6% in thigh/buttock, and 18.8% in the upper limb. Seventy-eight point thirteen percent received acenocoumarol, 15.63% LMWH, and 3.13% NOACs. Of the cases, 59.38% were due to AF, 15.63% to valvular heart disease/valve prosthesis, and 12.5% to PE/DVT. The mean time from diagnosis to surgical drainage was 2.66 days, mainly as a result of alterations in coagulation parameters. Forty-six point eighty-eight percent were reoperated for new drainage, cure or skin defect coverage, and 3 patients required embolisation. Of the patients, 78% needed consultation with other specialties. The average length of stay was 22.34 days, and the in-hospital mortality rate was 9.38%.
ConclusionTension haematomas in the extremities associated with anticoagulants occur in patients with multiple comorbidities that make them vulnerable. Surgical drainage is usually delayed by numerous factors which lead to skin defects that require further surgical operations, and prolonged hospital stays that are associated with medical complications. In our study, the average length of stay and in-hospital mortality rate were higher than those for hip fractures, so we should not underestimate this pathology.
Las complicaciones del tratamiento con fármacos anticoagulantes han sido ampliamente descritas, si bien los hematomas a tensión en extremidades se consideran en muchos casos patologías banales.
Material y métodoEstudio descriptivo retrospectivo entre 2014 y 2017, incluyendo a pacientes con hematomas tras un mínimo traumatismo en extremidades por anticoagulantes intervenidos por Traumatología.
ResultadosSe incluyó a 32 pacientes; el 81% eran mujeres, con una edad media de 83,56 años e ICCa de 5,97. La localización anatómica de los hematomas fue: el 65,6% en pierna/pie, el 15,6% en muslo/glúteo y el 18,8% en miembro superior. El 78,13% consumía acenocumarol, el 15,63% HBPM y el 3,13% NACO, siendo el 59,38% de los casos por FA, el 15,63% por valvulopatías/prótesis valvulares y el 12,5% por TEP/TVP. El tiempo medio desde el diagnóstico al drenaje quirúrgico fue de 2,66 días, principalmente por alteraciones de la coagulación. Un 46,88% fueron reintervenidos para nuevo drenaje, cura o cobertura del defecto cutáneo y 3 pacientes precisaron embolización. Fue necesaria la valoración por otras especialidades en el 78,1%. La estancia media fue de 22,34 días y la tasa de mortalidad intrahospitalaria del 9,38%.
ConclusiónLos hematomas a tensión por anticoagulantes en extremidades acontecen en pacientes pluripatológicos y ancianos frágiles. Habitualmente el drenaje quirúrgico se retrasa por multitud de factores, lo que conlleva defectos cutáneos amplios que requieren reintervenciones y estancias hospitalarias prolongadas que se asocian a complicaciones médicas. En nuestro estudio, los datos de estancia media y tasa de mortalidad son superiores a los de las fracturas de cadera, por lo que no debemos subestimar esta patología.
Pharmacological anticoagulant treatment is associated with many complications. Oral anticoagulants have a narrow therapeutic range, with frequent oscillations. A low INR is associated with a higher risk of thromboembolic complications, while overdosing is linked to haemorrhagic complications.
Intracranial and gastrointestinal bleeding are considered to be the most severe haemorrhagic complications. This is due to their repercussions in terms of morbidity and mortality, while cutaneous complications such as haematomas in the subcutaneous cellular tissue are often underestimated. This is so in spite of the case that they are the most frequent complication in several series,1,2 and they often fulfil the criteria defining serious bleeding.3 They are often considered to be trivial pathologies that do not require treatment.
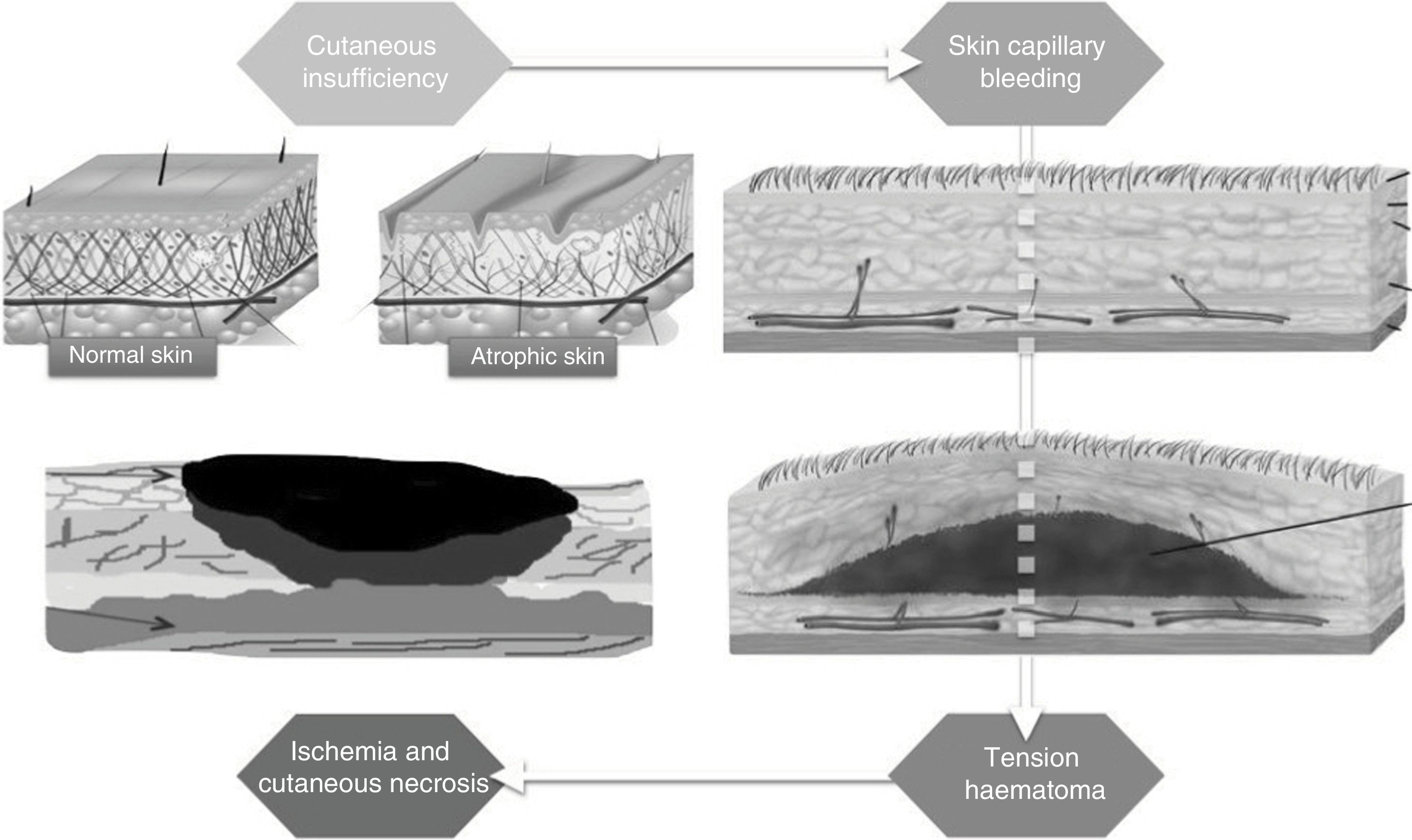
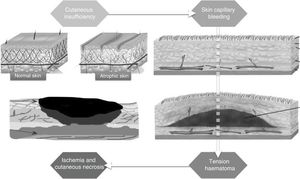
The term “dermatoporosis”4,5 is used to define the clinical manifestations and complications deriving from chronic cutaneous insufficiency. These start at the age of around 60 years old and progress with age, with signs such as senile purpura, cutaneous atrophy and delayed scar formation. This cutaneous insufficiency in elderly patients also gives rise to the appearance of tears and bruising after minimum trauma, due to the bleeding of vessels located in the subcutaneous cellular tissue under skin that is atrophic and fragile.
The blood that has accumulated in the virtual space between the subcutaneous fat and muscle fascia may exceed the arterial pressure in the skin capillaries, leading to ischaemia (Fig. 1). If this condition lasts over time it causes the formation of large areas of cutaneous necrosis (Fig. 2) that require broad surgical debridement, and in such cases it is difficult to cover soft tissues.
In other cases the haematomas open to the outside in the form of ulcerative lesions where scar formation is problematic. Due to the advanced age of the patients, underlying comorbidities and poor vascularisation in some anatomical locations, these lesions may last for months until they are completely resolved.
There is also evidence that suggests that the free radicals produced by iron after the decomposition of haemoglobin (Hb) in the haematoma contributes to damage of the surrounding tissue and wound morbidity.6
However, complications are not solely local, given that bleeding may lead to analytical and haemodynamic deterioration in vulnerable patients.7,8
This is why tension haematomas should always be evaluated for potential cutaneous involvement, and if signs of cutaneous suffering exist then early drainage of the haematoma is recommended.
Due to the formation of coagulae, these haematomas tend to be very difficult to empty using techniques that are not very invasive, such as needle aspiration. This is therefore usually performed by means of traditional surgical drainage, which normally requires the hospitalisation of the patient and general anaesthesia.
Although early drainage is recommended, it is not always possible to do this. The initial diagnosis is often difficult, given that the initial phases are characterised by erythema, tumefaction, a rise in temperature and pain, without being associated with a clear traumatic event. Many cases are confused at first with cellulitis and treated using antibiotic therapy,9,10 so that only when the symptoms persist or evolve poorly are cases referred to hospital. In many other cases it is necessary to wait to correct coagulation times, and this delays treatment.
ObjectivesTo determine the characteristics of patients with tension haematomas caused by anticoagulants in their extremities and drained surgically, analysing their morbidity and mortality together with hospitalisation data due to this cause.
Material and methodsThis is a retrospective descriptive study based on data gathered from patient clinical histories.
Patients over the age of 65 years old were included, with haematomas that were either spontaneous or followed minimum trauma in the extremities, associated with the use of anticoagulant drugs and who received surgery in the Orthopaedic Department from 2014 to 2017, in the Hospital Clínico San Carlos (HCSC), Madrid.
Exclusion criteria were also established (Table 1).
Of the patients diagnosed at discharge and coded according to eCIE10ES as “M79.81: non-traumatic soft tissue haematoma” and “T45.515: adverse effect of anticoagulants”, we selected those with involvement of the extremities and surgical drainage.
The surgical treatment performed was similar in all of the patients. Under aseptic conditions a deep incision was made over the most fluctuating zone that did not have cutaneous involvement. This incision was made following the skin tension lines. The virtual cavity which contained the haematoma was then opened, and it was emptied by digital manoeuvres and manual compression from the exterior. The haematoma was usually coagulated and retained, requiring in-depth washing with physiological saline solution to eliminate all of the haematic residues (Figs. 3 and 4).
Suction drainage was then put into place to prevent blood accumulating once again. If possible the skin edges were joined using silk and a compressive bandage was applied to control bleeding.
When the surgical drainage was created after a delay there was increased probability of skin necrosis, so that after emptying the haematoma it was not possible to close the skin directly. In these cases the skin edges had to be brought closer together, with planned dressings until a second attempt at closure or a skin defect coverage procedure could be performed. Sometimes a vacuum-assisted closure (VAC) system had to be applied, to aid the formation of granulation tissue.
A range of variables were recorded: age, sex, Charlson Comorbidity Index (CCI), Hb and INR at admission, delay before surgical drainage, average hospitalisation time, repeat surgery percentage and mortality rate.
Version 23 of the SPSS program was used for statistical data analysis (SPSS Inc, Chicago, Illinois, USA). Quantitative variables were described by their average and standard deviation, to facilitate comparison of our results with those of other published studies. Categorical variables were shown as a frequency and percentages.
Results32 of the 42 cases selected at first were included (7 were excluded as they did not require surgical drainage, and 3 were drained in the surgery).
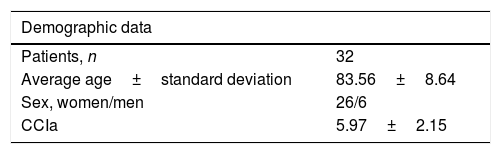
Regarding the demographic characteristics of the patients, 26 were women (81%) and only 6 were men (19%). The average age of the patients was 83.56±8.64 years old, and their age-adjusted Charlson Comorbidity Index (CCIa) was 5.97±2.15 (estimated survival at 10 years 2.25%) (Table 2).
65.6% of haematomas were located in the leg or foot, 15.6% in the thigh or buttock and 18.8% in an upper limb (Table 3).
78.13% of the patients were taking acenocumarol (Sintrom®), 15.63% low molecular weight heparin (LMWH) and 3.13% were taking the new oral anticoagulants (NOAC). 59.38% of the cases were being treated for atrial fibrillation, 15.63% for valve prosthesis pathologies, and 12.5% for pulmonary thromboembolism or previous deep vein thrombosis.
The initial Hb was<12mg/dl in 68.8% (22 patients) and INR was>1.2UI in 71.9% (23 patients). 28.1% (9 patients) had thrombocytopenia at admission, while 25% had a high average platelet volume (8 patients with APV>10fl).
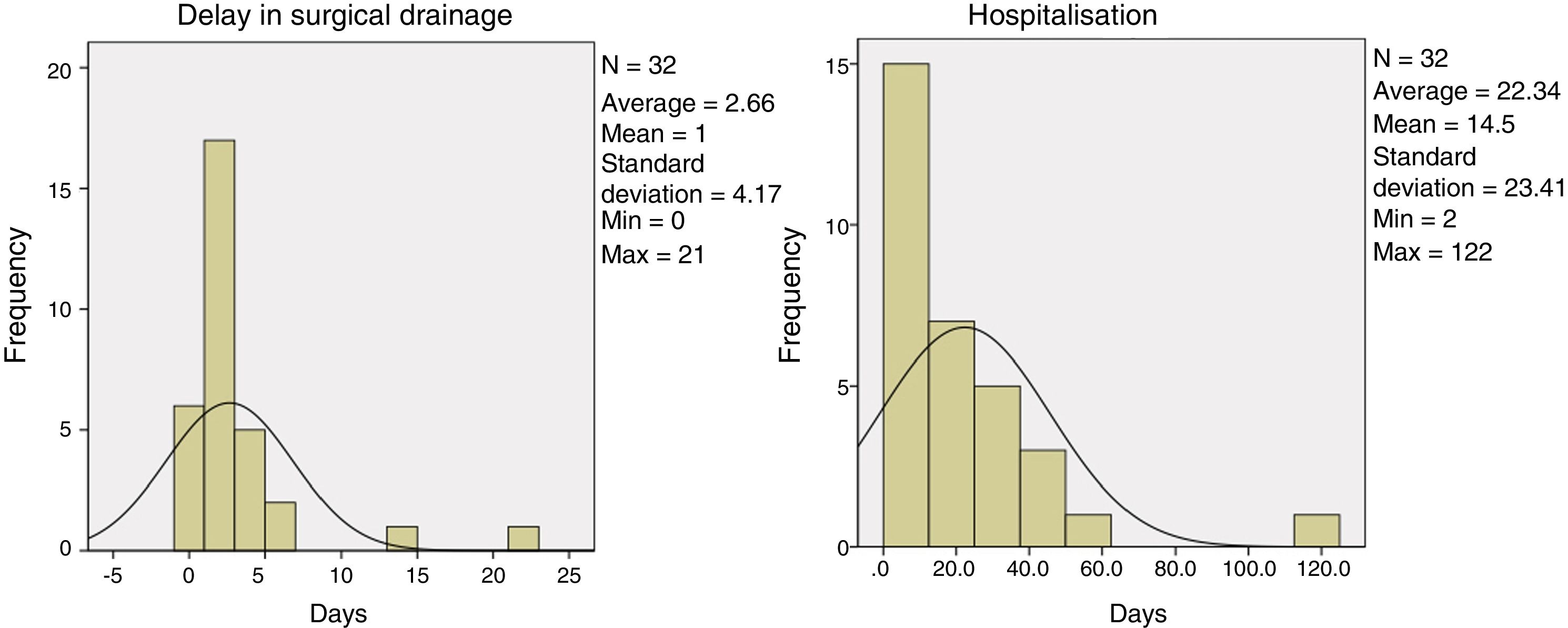
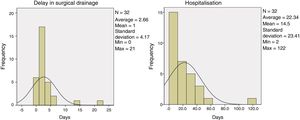
The average time from diagnosis to surgical drainage was 2.66±4.17 days, mainly due to coagulation alterations. It was not possible to calculate the average delay in requesting hospital care as this datum was not included in all of the clinical histories.
Direct closure of the skin after emptying the haematoma was achieved in a total of 17 patients, while a skin defect remained in 15 patients, of which: frequent dressings were performed in 6 patients, achieving closure at the second attempt. A VAC system was used in 2 patients, in 5 patients an autologous free skin graft was performed, while rotational flaps were used in 2 patients. As well as the aforementioned additional surgical procedures, several of the patients in which direct closure was not possible required a new drainage or dressing in the operating theatre (Fig. 5), so the total percentage of patients who received repeat surgery amounted to 46.88%.
Tension haematoma in the leg with delayed surgical drainage and poor evolution: (a and b) Tension haematoma in the lateral and medial leg leading to skin involvement. (c) Drainage and direct closure of the skin. (d) Drainage of the haematoma and approximation of edges due to the impossibility of direct closure. (e and f) Poor evolution of the skin with clear signs of necrosis.
Additional complications meant that 3 patients needed embolisation due to persisting signs of bleeding that could not be controlled using conventional surgical techniques. A total of 6 patients were treated using antibiotic therapy and local dressings, as the haematoma was infected.
An evaluation by other specialities was necessary in 78.1% of the patients: 10 by general medicine, 12 by plastic surgery, 7 by geriatrics, one by cardiology and 2 by other specialities. Several patients had to consult different specialists at the same time.
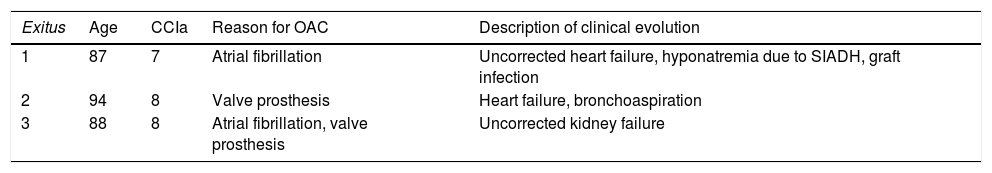
The average duration of hospitalisation was 22.34±23.41 days (Fig. 6) and the intrahospital mortality rate was 9.38% (3 cases), due to their underlying pathology becoming acute again (Table 4).
Description of the characteristics of patients who died.
| Exitus | Age | CCIa | Reason for OAC | Description of clinical evolution |
|---|---|---|---|---|
| 1 | 87 | 7 | Atrial fibrillation | Uncorrected heart failure, hyponatremia due to SIADH, graft infection |
| 2 | 94 | 8 | Valve prosthesis | Heart failure, bronchoaspiration |
| 3 | 88 | 8 | Atrial fibrillation, valve prosthesis | Uncorrected kidney failure |
In many hospitals this pathology is managed by emergency doctors, dermatologists or plastic surgeons. In our hospital it is treated by the Orthopaedic Surgery and Traumatology Department.
Striking findings in our results are the percentages of patients who required evaluation by other specialists, the percentage of patients who received repeat surgery, overall average hospitalisation lasting for longer than 20 days and a significant rate of intrahospital mortality, close to 10%.
There is a notable lack of literature on this subject, and it is mainly composed of publications of case studies7,11,12 and descriptions of different haematoma drainage techniques13–16 together with methods of dressing the wounds deriving from haematomas.
We only found 2 descriptive studies which include a series of cases similar to our study of subcutaneous haematomas in the extremities.
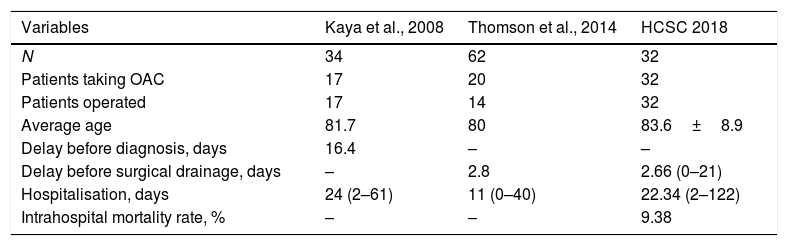
A paper published by Kaya et al.17 includes 34 patients with subcutaneous haematoma, which in 17 patients were caused by anticoagulants and treated by surgery. They used NMR to precisely evaluate the anatomical extension of lesions, together with the histological analysis of the tissue obtained. They also recorded an average delay prior to hospital treatment of 16.4 days, as well as the cost of hospital treatment.
Another more recent study by Thomson et al.18 included 62 patients with pretibial haematomas following minor trauma, of which 20 were due to treatment with acenocumarol. 14 of them were treated surgically and 6 received conservative treatment. They also recorded the mechanism of injury – a casual fall, or trauma caused by collision with furniture or a tool –, the need for transfusion in 4 patients and the cost of hospital treatment.
The results in both studies were similar to each other and to those of our study in terms of the type of elderly patient, with a high level of comorbidity, delay before surgery after diagnosis and duration of hospitalisation (Table 5).
Comparison of published studies on subcutaneous haematomas in the extremities.
| Variables | Kaya et al., 2008 | Thomson et al., 2014 | HCSC 2018 |
|---|---|---|---|
| N | 34 | 62 | 32 |
| Patients taking OAC | 17 | 20 | 32 |
| Patients operated | 17 | 14 | 32 |
| Average age | 81.7 | 80 | 83.6±8.9 |
| Delay before diagnosis, days | 16.4 | – | – |
| Delay before surgical drainage, days | – | 2.8 | 2.66 (0–21) |
| Hospitalisation, days | 24 (2–61) | 11 (0–40) | 22.34 (2–122) |
| Intrahospital mortality rate, % | – | – | 9.38 |
Although we did not find much literature on haematomas caused by anticoagulants in the extremities, there are more publications covering a broader range of issues in connection with pretibial lacerations.19–21 These lesions have similar characteristics and it is possible to restore skin continuity in them. They too usually occur in elderly patients with skin-weakening pathologies in association with anticoagulant drugs and other types. The incidence of pretibial lacerations is estimated to stand at 1.1% for men and 6.1% for women aged from 70 to 74 years old, with a tendency that rises with increasing age up to 4% in men and 30% in women aged 85 years old or more.22
Although we have no data on the incidence of subcutaneous haematomas caused by anticoagulants, we believe that there are a significant number of cases. On the one hand we have an ageing population in which 19.2% are over the age of 65 years old, with a tendency to increase (up to 25.2% in 2033, according to 2018 estimations by the INE).23 And on the other hand, the percentage of patients taking oral anticoagulants stands at from 1.3% to 2%,24 a percentage that increases with age. If both figures are combined we have a large increase in the number of individuals who unify both basic risk factors for the development of this pathology: advanced age and anticoagulant therapy.
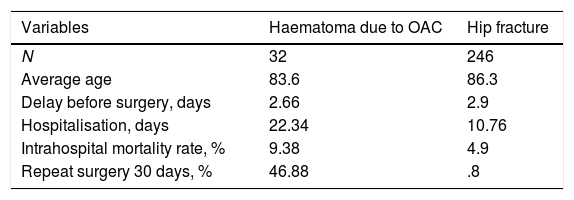
This issue is not only important because of its incidence, as its consequences are relevant, too. Thus if we compare these data with those extracted from the 2017 annual report of the National Registry of Hip Fractures25 on patients operated for hip fracture in our hospital, we find that they are patients with similar characteristics. They are elderly with multiple comorbidities and require surgery; nevertheless, tension haematomas in the extremities are associated in our study with a higher percentage of repeat surgery, longer average hospitalisation and a higher rate of intrahospital mortality (Table 6).
Comparison of data of patients operated for hip fracture vs. haematoma in Hospital Clínico San Carlos.
| Variables | Haematoma due to OAC | Hip fracture |
|---|---|---|
| N | 32 | 246 |
| Average age | 83.6 | 86.3 |
| Delay before surgery, days | 2.66 | 2.9 |
| Hospitalisation, days | 22.34 | 10.76 |
| Intrahospital mortality rate, % | 9.38 | 4.9 |
| Repeat surgery 30 days, % | 46.88 | .8 |
Orthopaedic surgeons are currently aware of the importance of treating hip fractures as soon as possible in clinically stable patients, achieving early sitting and walking, as this has been proven to contribute to reducing their complications and mortality as they spend less time lying in bed.26,27 In the same way, this is also important for patients with haematomas as delaying treatment and the consequences of this may have a negative impact on their final evolution. One way of achieving early drainage may be to withdraw anticoagulation therapy from these patients.
We believe that the data we obtained showing higher mortality and longer average hospitalisation in patients with tension haematomas in the extremities may be due to a longer time spent immobilised with the aim of achieving good closure of the skin. It is widely accepted that long periods of hospitalisation and immobilisation are risk factors for a poor outcome.28 Although the time patients remained immobilised due to operations for haematoma was not recorded directly in our study, we believe that it was longer than the corresponding immobilisation of patients operated for hip fracture. In this case we believe that the result of higher intrahospital mortality would be accompanied by greater functional deterioration due to loss of muscle mass and bone mineral density caused by the prolonged immobilisation in bed of elderly frail patients.
Several authors describe the benefits of early mobilisation instead of bed rest in elderly patients with skin grafts in pretibial lesions.29,30 This does not adversely affect the evolution of the graft, and it also helps to reduce the duration of hospitalisation and associated morbidity.
As well as the general consequences described above, it is important o underline the local complications of haematomas. These include problems with wound closure, skin defects that require procedures to ensure skin coverage and infections, etc. These may be prevented by early drainage in those tension haematomas that show signs of skin suffering or in very large haematomas.
No previous study of subcutaneous haematomas shows the percentage of repeat surgery or the need for multidisciplinary treatment by general medicine specialists, geriatricians, plastic surgeons and cardiologists, etc., after patient admission to reduce complications and the intrahospital mortality rate, as this study does.
The limitations of our study include its retrospective nature, as data were gathered from patient clinical records. It is descriptive and lacks a control group, making it impossible to establish a statistical relationship. We also performed a short follow-up of each patient, given that we restricted this to the time they spent in hospital, without gathering data on their long-term evolution. Although this study covers more patients with haematomas in their extremities caused by anticoagulants than any other published study, the number of cases here is limited. All of the above factors mean that we have to be cautious in the conclusions deriving from our results.
Given these findings, we consider it to be fundamental to raise awareness among primary care doctors, specialists and patients regarding the possible consequences of subcutaneous tension haematomas, so that early diagnosis and treatment are able to improve the outcome of these lesions. We recommend an alert attitude above all when faced with elderly patients with signs of cutaneous fragility when they are being treated with anticoagulant drugs. As well as treating these lesions at an early stage we believe that, as is the case with hip fracture patients, early mobilisation of these patients may reduce their hospital stay and associated morbidities.
ConclusionsTension haematomas in the extremities due to anticoagulants occur in patients with multiple pathologies and frail elderly patients.
Surgical drainage is often delayed due to many factors, and this often leads to large skin defects that require repeat surgery and long periods of hospitalisation and immobilisation that in vulnerable patients are associated with medical complications and functional deterioration.
In our study the data on the average duration of hospitalisation, the percentage of repeat surgery and the rate of intrahospital mortality are higher than those for hip fractures, so this pathology should not be underestimated.
Level of evidenceLevel of evidence III.
FinancingThis research received no specific financing from public, commercial or not-for-profit entities.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Galán-Olleros M, Valle-Cruz JA, García-Coiradas J, González-Pérez A, Rodríguez-González FA, Alcobía-Díaz B, et al. Hematomas subcutáneos a tensión por anticoagulantes en ancianos: ¿más morbimortalidad precoz que las fracturas de cadera? Rev Esp Cir Ortop Traumatol. 2019;63:361–369.