To evaluate the results of vascular reconstruction in soft tissue sarcoma surgery and establish an algorithm based on current evidence.
Materials and methodsWe studied patients undergoing soft-tissue sarcoma in a tertiary hospital. A retrospective review of 8 cases was carried out, analysing the demographics, surgical planning, complications, disease-free survival and bypass patency.
ResultsSuccessful limb preservation was observed in all patients, and the bypass remained patent in all cases. The mean follow-up was 38.4 months average, with 87.5% survival and no recurrences.
ConclusionsThe involvement of major vascular structures in soft tissue sarcomas of the limbs does not necessarily exclude resectability. In selected cases, resection is possible with vascular reconstruction and limb preservation. However, multidisciplinary planning is needed.
Valorar los resultados de las reconstrucciones vasculares en la cirugía de sarcomas de partes blandas y establecer un algoritmo de actuación con base a la evidencia actual.
Material y métodosSe han estudiado los pacientes intervenidos de sarcoma de partes blandas en un hospital terciario. Revisión retrospectiva de 8 casos; ha sido analizado: la demografía, la planificación quirúrgica, las complicaciones, la supervivencia libre de enfermedad y global, y la permeabilidad del bypass.
ResultadosSe ha objetivado que todos los pacientes han preservado la extremidad y el bypass ha permanecido permeable en todos los casos. El seguimiento fue de 38,4 meses de media, con el 87,5% de supervivencia y ausencia de recidivas.
ConclusionesEl envolvimiento de estructuras vasculares principales en los sarcomas de partes blandas en extremidades no necesariamente impide la resecabilidad. En los casos seleccionados es posible la resección con reconstrucción vascular y preservación de extremidad. No obstante, es necesaria una correcta planificación multidisciplinar.
At present, surgical resection is the only potentially curative option for the management of soft tissue sarcomas. Historically, large vessel involvement has represented a contraindication to resection of retroperitoneal sarcomas, in turn leading to amputations in cases of limb sarcomas.1–4 Currently, the standard management paradigm of soft tissue sarcomas involves surgical resection with adjuvant radiotherapy and achieves a high rate of success, as well as limb preservation.5–13 The main goal of resection is to obtain tumour-free margins. Limb preservation techniques represent a therapeutic approach which should be taken into account and analysed in relation to ablative surgery upon suspicion of large vessel involvement.14–25 It seems clear that the management of these tumours requires a multidisciplinary and experienced team, so that the low regional casuistry may provide a single team with adequate resources.
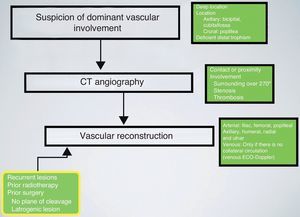
Although the cited studies do not provide abundant scientific evidence, we analyse our series and define an algorithm for the management of patients with soft tissue sarcomas and suspected involvement of large vessels in the limbs.
Materials and methodsThe study was a retrospective review of a tertiary hospital with a multidisciplinary team for the management of sarcomas. The core of this team consisted of: medical oncology, radiation oncology, plastic surgery, orthopaedic surgery, radiology, anatomical pathology and specialised nursing staff.
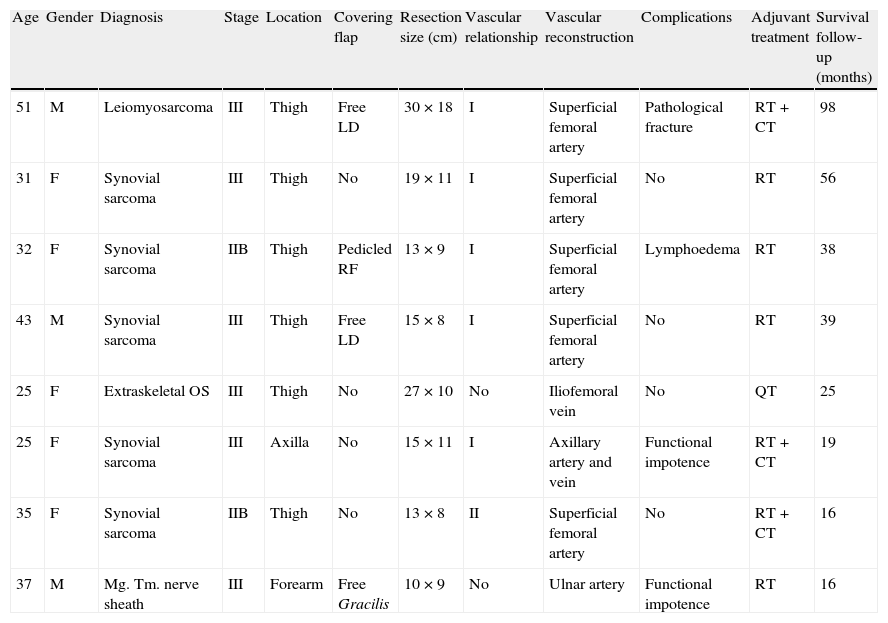
We reviewed a total of 8 patients (Table 1), who were treated between the years 2003 and 2010. All patients suffered soft tissue sarcomas in the limbs and underwent vascular reconstruction techniques. All patients were presented at the Committee of sarcomas. All patients underwent a needle biopsy procedure directed by ultrasound or computed tomography (CT) scan for diagnosis. CT angiographies and extension studies with abdominothoracic CT or positron emission tomography (PET) were also conducted. Therapeutic strategies were established by the Committee. Monitoring was carried out at 15 days, 30 days, 2 months, 6 months and then every 6 months up to 5 years. Physical examination was systematic and thorough. The correct presence of distal pulses and the absence of venous insufficiency stigmata were incorporated as clinical signs of bypass patency. In addition, all patients underwent serial magnetic resonance imaging (MRI) scans. Early and late complications, reoperations, survival, recurrence and mortality were all evaluated during monitoring. The mean follow-up period for the series was 38.4 months (range: 16–98 months).
Results.
| Age | Gender | Diagnosis | Stage | Location | Covering flap | Resection size (cm) | Vascular relationship | Vascular reconstruction | Complications | Adjuvant treatment | Survival follow-up (months) |
| 51 | M | Leiomyosarcoma | III | Thigh | Free LD | 30×18 | I | Superficial femoral artery | Pathological fracture | RT+CT | 98 |
| 31 | F | Synovial sarcoma | III | Thigh | No | 19×11 | I | Superficial femoral artery | No | RT | 56 |
| 32 | F | Synovial sarcoma | IIB | Thigh | Pedicled RF | 13×9 | I | Superficial femoral artery | Lymphoedema | RT | 38 |
| 43 | M | Synovial sarcoma | III | Thigh | Free LD | 15×8 | I | Superficial femoral artery | No | RT | 39 |
| 25 | F | Extraskeletal OS | III | Thigh | No | 27×10 | No | Iliofemoral vein | No | QT | 25 |
| 25 | F | Synovial sarcoma | III | Axilla | No | 15×11 | I | Axillary artery and vein | Functional impotence | RT+CT | 19 |
| 35 | F | Synovial sarcoma | IIB | Thigh | No | 13×8 | II | Superficial femoral artery | No | RT+CT | 16 |
| 37 | M | Mg. Tm. nerve sheath | III | Forearm | Free Gracilis | 10×9 | No | Ulnar artery | Functional impotence | RT | 16 |
CT: chemotherapy; F: female; LD: Latissimus dorsi; M: male; Mg. Tm.: malignant tumour; OS: osteosarcoma; RF: Rectus femoris; RT: radiotherapy.
Vascular relationship: I: arterial and venous involvement; II: arterial involvement; III: venous involvement; No: accidental cause.
Study limitations: retrospective and reduced sample.
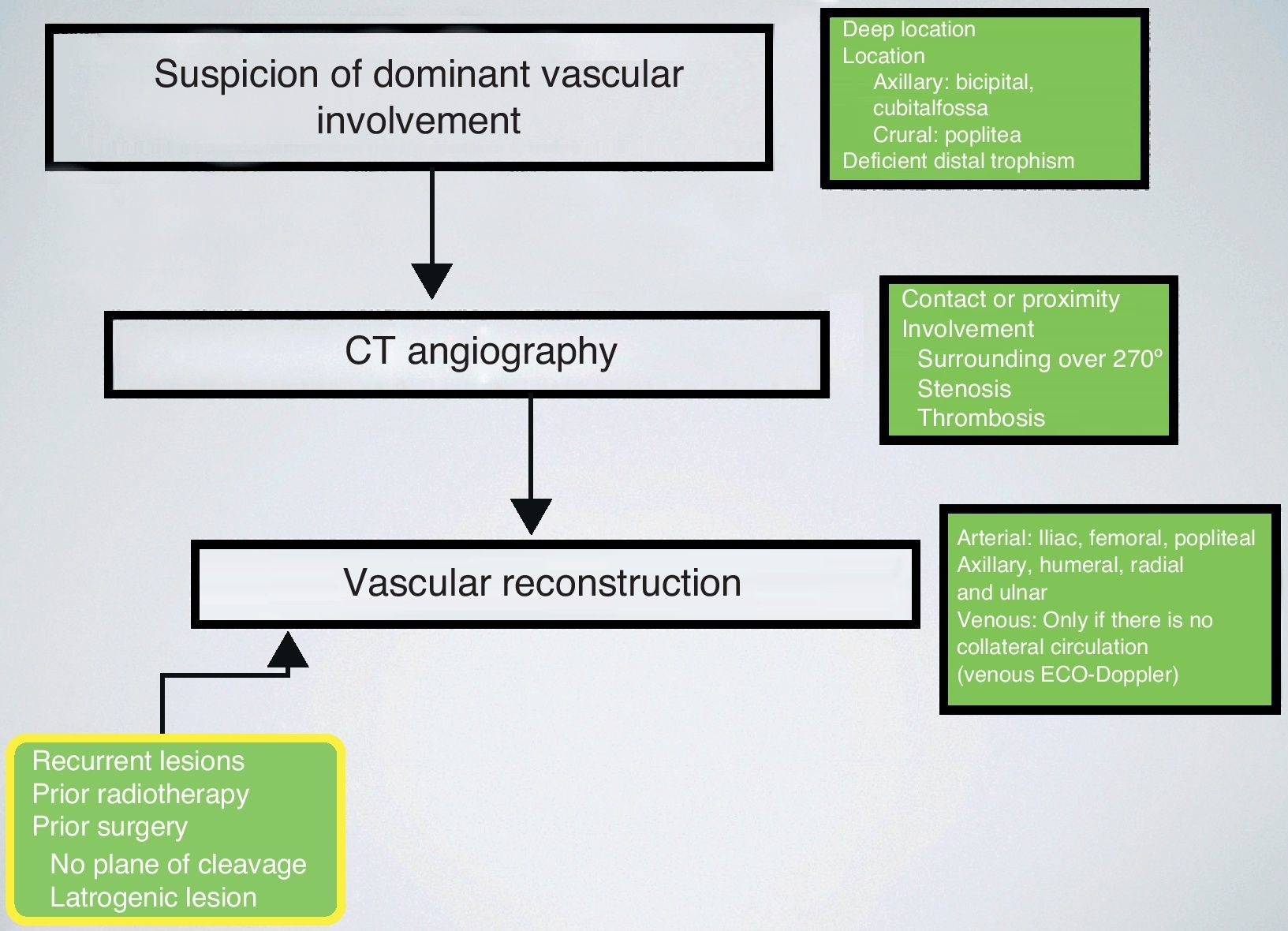
Vascular reconstructionsPatients with tumours in anatomical locations which could compromise dominant vascular axes, such as the crural region, popliteal space, axillary fossa and cubital fossa, underwent vascular studies using CT angiography. All cases were reviewed by a radiologist with ample experience in musculoskeletal sarcomas. Preoperative planning considered infiltrations of the vascular axis when the existence of venous thrombosis or vascular stenosis was noted and when the tumoural mass surrounded over 270° of the vascular perimeter.
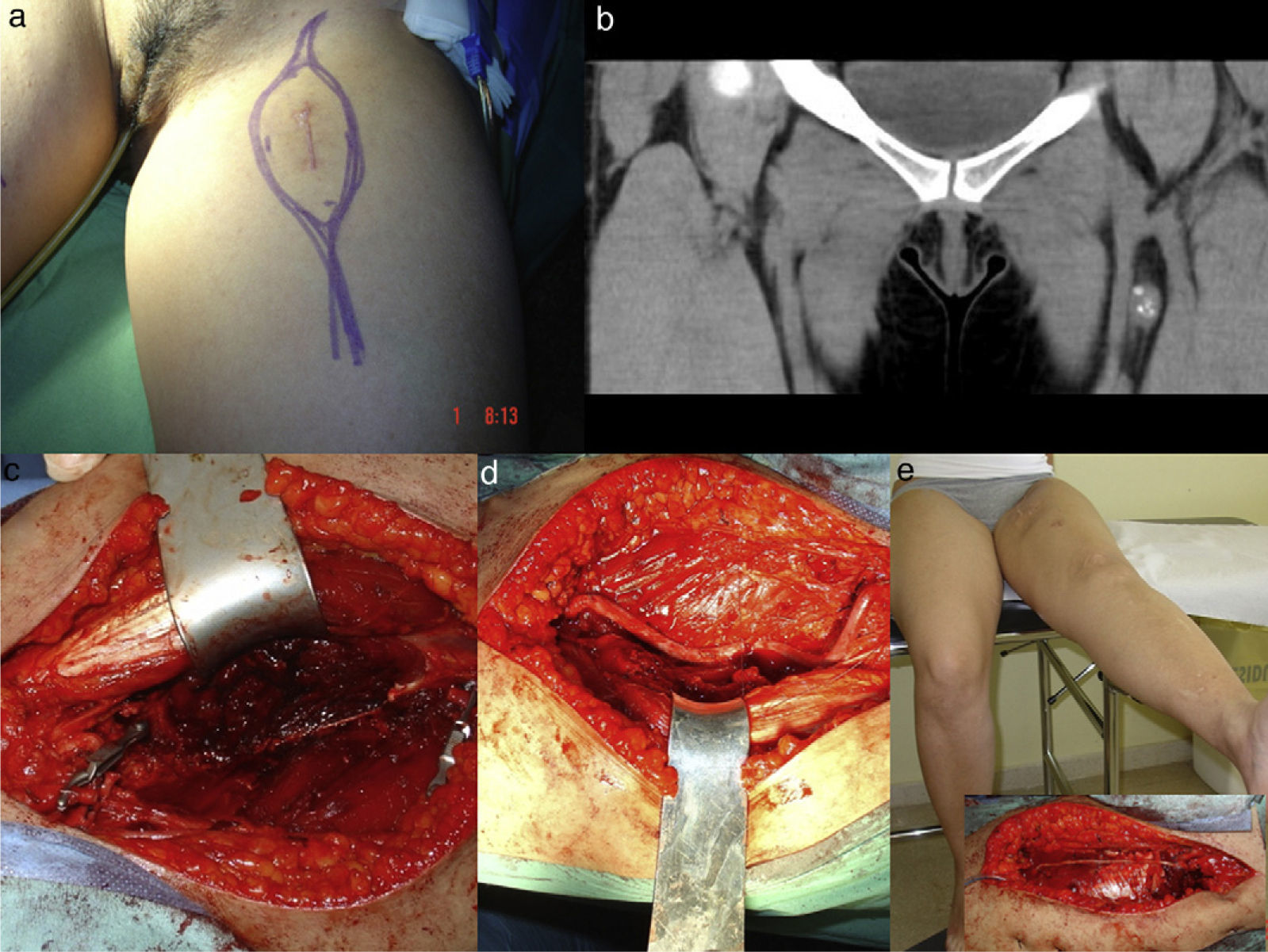
All patients were operated by the same oncological and reconstructive team, formed by plastic surgeons and led by the senior specialist (JMVV performed the vascular reconstructions). Reconstructions were carried out with contralateral saphenous vein grafts. All anastomoses were termino-terminal and performed under 3.5× magnification with 8/0 nylon suture. In total, 8 arterial reconstructions and 1 venous reconstruction were conducted. Figs. 1 and 2 illustrate vascular reconstructions.
Synovial sarcoma of the thigh. (a) Preoperative approach design. (b) Coronal CT image with a heterogeneous mass on the femoral vascular bundle. (c) Detail of a radical resection. (d) Vascular reconstruction with contralateral great saphenous vein. (e) Detail of crural nerve reconstruction with sural graft and adequate extension at 12 months postoperatively.
Table 1 shows the results of the series. In oncological terms, we highlight the free margins achieved in 7 of 8 patients, with the case of affected margins corresponding to a contact with the femoral diaphysis. All patients presented high-grade tumours (G2 or G3), recurrent in 6 cases and all tributaries of complementary treatments. With a mean follow-up period of 34.8 months we obtained limb preservation in all cases, without any recurrences and a survival rate of 87.5%. Clinically, we observed 100% patency of the reconstructions. Functionally, patients underwent the Toronto Extremity Salvage Score (TESS) scale and obtained an acceptable mean result of 82±16. Regarding complications, we noted 1 case of pathological fracture which was treated by intramedullary fixation, 1 case of grade II lymphoedema which was treated with compressive measures and rehabilitation and 2 cases of upper extremity functional impotence. We did not observe flap necrosis, dehiscence or wound infections.
DiscussionThe involvement of vascular structures represents a relatively common obstacle in the process of healing and restitution ad integrum of patients with sarcoma. The need to obtain tumour-free margins is generally considered23–29 as the main reason for vascular reconstruction in limb sarcomas. In strict compliance with this criterion, all sarcomatous tumours in proximity to large vessels should lead to resection with margins and vascular reconstruction. Other clear indicators are vascular involvement by the tumour and iatrogenic lesion of large vessels during surgery. In our experience, the most common cause is precisely vascular involvement as demonstrated by imaging studies. This is probably due to the fact that the majority concerned recurrent cases. Cases of proximity to vascular structures and primary tumours are usually managed with conservative surgery and complemented locally with radio- or brachytherapy. The prevalence of vascular reconstruction procedures among the total series of soft tissue sarcomas treated at our unit was 6%, which was within the range described in literature.22–26
Vascular reconstructions in the current series were performed by the same surgical team, responsible for oncological and reconstructive surgery, and counting with microsurgery and vascular skills. The reviewed literature noted the presence of a vascular surgeon for performing vascular reconstructions.
Regarding the choice of material for vascular reconstruction, no scientific evidence was found which ruled out any options. Thus, it would appear possible to conduct reconstructions with autologous vein or vascular prostheses. Some studies recommend the use of autologous grafts whenever possible, mainly in venous reconstructions.19,24,26 We opted for the use of autologous material in all cases, advocating the need for complementary treatments, normally radiotherapy, and the complications of prosthetic material in such a hostile tissue environment. Complications related to the reconstructions did not include any cases of thrombosis, obliteration of the bypass or wound superinfection. The possibility of an extra-anatomical prosthetic bypass was contemplated by the surgical salvage team for cases of local major complications (flap necrosis, wound dehiscence or infection with risk of vascular complications).
The decision to perform an autologous bypass also required adequate local coverage. In this context, we considered it vital that the tissue overlying the bypass, either by means of flaps (local or free) or by remnant tissue, corresponded to a well-vascularised tissue structure. We used muscle flap coverage in 50% of cases: 3 microsurgical (2 Latissimus dorsi and 1 Gracilis) and 1 local (Rectus femoris).
The decision to carry out venous reconstruction was considered only when the superficial system was incompetent. On the other hand, its repair seemed preferable in order to avoid distal venous hypertension and its sequelae.26 However, venous reconstruction often leads to vascular complications such as oedema and graft occlusions, so we opted for not reconstructing the venous axis in 7 of the 8 patients. No venous complications were observed and there was only 1 case of lymphoedema.
The use of CT angiography enabled the relationship between the tumour and the vascular trunks to be studied. We considered this study essential for adequate surgical planning. Moreover, arterial and venous angiographies were only conducted in 2 cases, which also enabled preoperative embolisation in certain hypervascular tumours located in complex anatomical regions.30 We considered that this CT angiography study provided sufficient information, thus rendering angiography dispensable.
Although this series did not contain enough patients to enable meaningful statistical tests, we believe that vascular reconstruction offers the possibility of conducting limb-sparing surgery in cases of tumour resection with associated vascular lesions. The surgical team must include specialists with sufficient oncological, vascular and reconstructive skills to manage this type of condition, as well as those cases in which vascular reconstructions are not planned, but become necessary nonetheless because trunks are damaged in an oncological or iatrogenic manner (Fig. 3).
Level of evidenceLevel of evidence IV.
Ethical responsibilitiesProtection of human and animal subjectsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestThe authors have no conflict of interest to declare.
Please cite this article as: Viñals Viñals JM, et al. Reconstrucción vascular durante la cirugía de sarcomas para la preservación de extremidades: serie de casos y algoritmo de manejo. Rev Esp Cir Ortop Traumatol. 2013;57:21–6.