In this article, a discussion is presented on the following aspects of sudden death, related to legal medicine. The epidemiological aspects and diseases associated with sudden death are discussed first. This is followed by presenting the chain of events leading to the final arrhythmias triggering sudden death, and the legal aspects of this.
This is a comparative study of the final arrhythmias responsible of sudden death in patients with: (1) acute myocardial infarction; (2) with no apparent heart disease; and (3) with heart failure. A comparison is also made between the incidence of ischaemic heart disease, acute coronary thrombosis, and left ventricular hypertrophy.
En este artículo comentamos varios aspectos de la muerte súbita, relacionados con la medicina legal. En primer lugar, se exponen los aspectos epidemiológicos y las enfermedades asociadas a la muerte súbita. Más tarde, se discute la cadena de eventos que llevan a las arritmias finales a desencadenar la muerte súbita y sus aspectos legales.
Se hace un estudio comparativo de las arritmias finales responsables de la muerte súbita en pacientes: 1) con infarto agudo; 2) ambulatorios sin cardiopatía evidente y 3) con insuficiencia cardiaca evidente, y también se comparan las diferencias de incidencia de cardiopatía isquémica, trombosis coronaria aguda e hipertrofia ventricular isquémica.
Sudden death (SD) probably represents the most significant challenge of modern cardiology due to the large number of cases which exist (in the USA alone there are more than 400,000/year) and due to its resulting significant social impact. However, its incidence is lower in some Mediterranean countries such as Spain.1–6
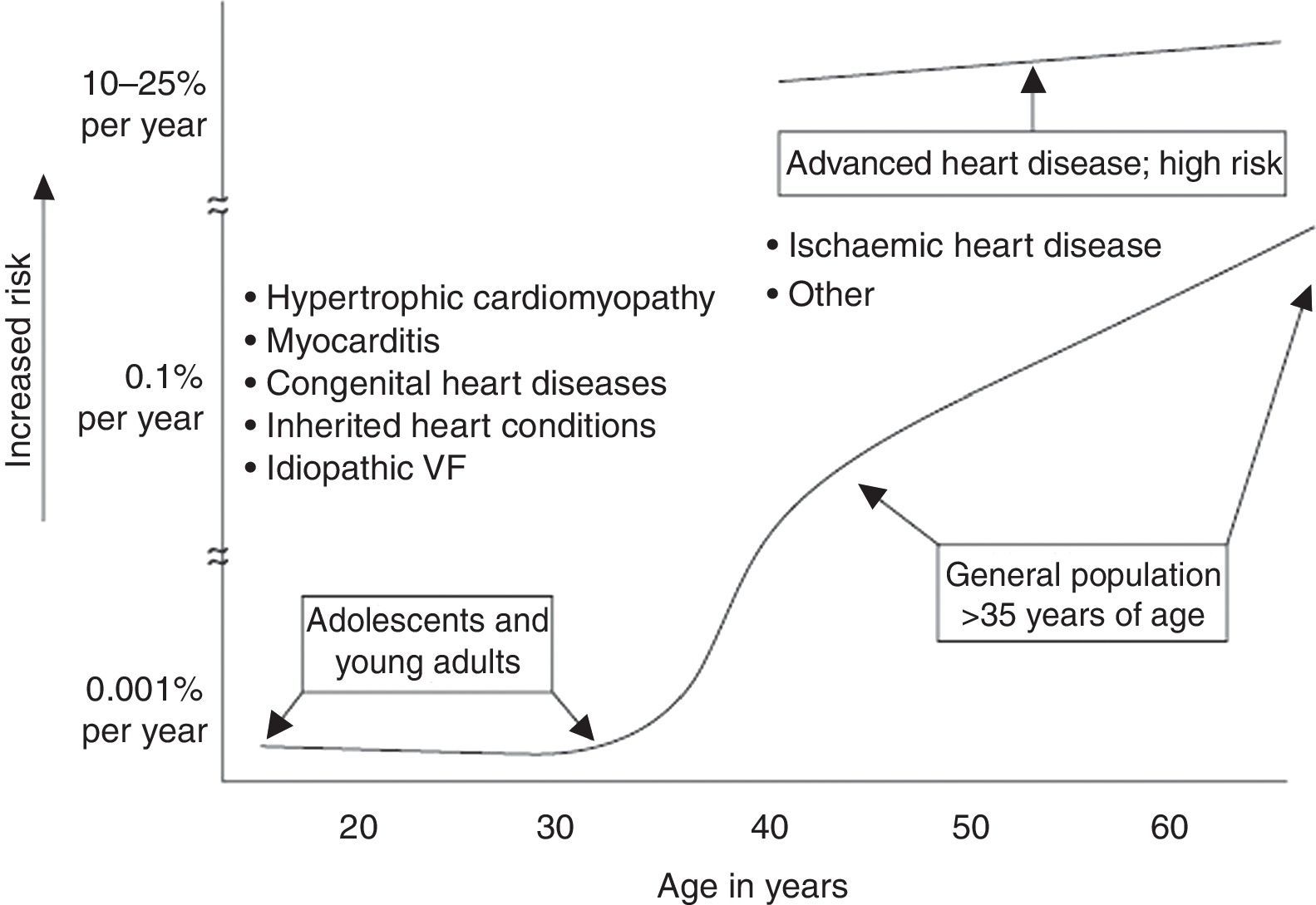
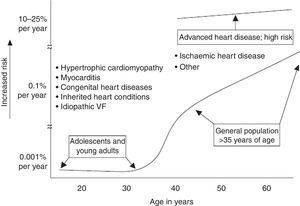
Although SD can even occur in infants, related to repolarisation disorders, autonomic nervous system abnormalities and increased vagal tone, it is in fact rare in the first few decades of life. In young subjects, it often occurs while doing sport.7 In these cases, it tends to develop in the presence of inherited heart conditions (hypertrophic cardiomyopathy, arrhythmogenic right ventricular dysplasia/cardiomyopathy and channelopathies). The incidence of SD increases gradually, but significantly, from the age of 35 to 40 years, and it is particularly high in the acute phase of myocardial infarction (MI). It is also common in the chronic phase of this disease and in any heart disease, especially in the presence of heart failure (HF)8 (Fig. 1).
Associated diseasesAs we have just stated, acute ischaemic heart disease (IHD) is frequently associated with SD in adults. In most cases of SD, aside from acute IHD and channelopathies, HF or, at least, ventricular dysfunction can be identified. HF can be associated with idiopathic cardiomyopathy, or be present in patients with chronic IHD, hypertension, cardiomyopathies of another aetiology, etc. Inherited heart conditions can cause SD at any age, but their overall impact is small (Fig. 1).
It is worth highlighting, however, that they are responsible for many cases of SD which occur before the age of 35 years. Inherited heart conditions are more prevalent in males and can occur during physical exercise (cardiomyopathies), at rest or during sleep (channelopathies).
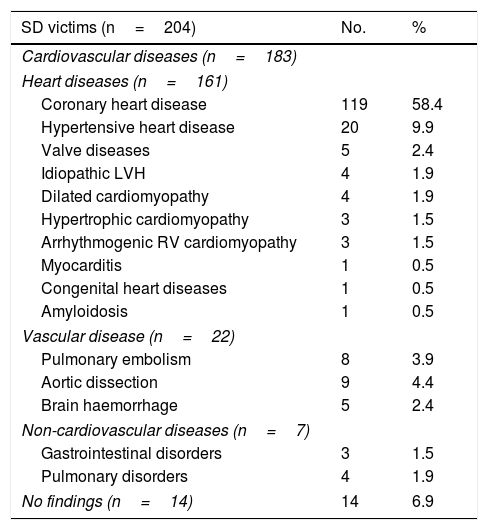
Our group conducted a study (EULALIA study) which included 204 cases of SD occurring in a Mediterranean region.9 This study analysed the epidemiological, anatomical and pathological aspects of diseases associated with SD. Table 1 shows the pathological diagnosis obtained in this group of patients.
Diseases associated with SD: autopsy study.
| SD victims (n=204) | No. | % |
|---|---|---|
| Cardiovascular diseases (n=183) | ||
| Heart diseases (n=161) | ||
| Coronary heart disease | 119 | 58.4 |
| Hypertensive heart disease | 20 | 9.9 |
| Valve diseases | 5 | 2.4 |
| Idiopathic LVH | 4 | 1.9 |
| Dilated cardiomyopathy | 4 | 1.9 |
| Hypertrophic cardiomyopathy | 3 | 1.5 |
| Arrhythmogenic RV cardiomyopathy | 3 | 1.5 |
| Myocarditis | 1 | 0.5 |
| Congenital heart diseases | 1 | 0.5 |
| Amyloidosis | 1 | 0.5 |
| Vascular disease (n=22) | ||
| Pulmonary embolism | 8 | 3.9 |
| Aortic dissection | 9 | 4.4 |
| Brain haemorrhage | 5 | 2.4 |
| Non-cardiovascular diseases (n=7) | ||
| Gastrointestinal disorders | 3 | 1.5 |
| Pulmonary disorders | 4 | 1.9 |
| No findings (n=14) | 14 | 6.9 |
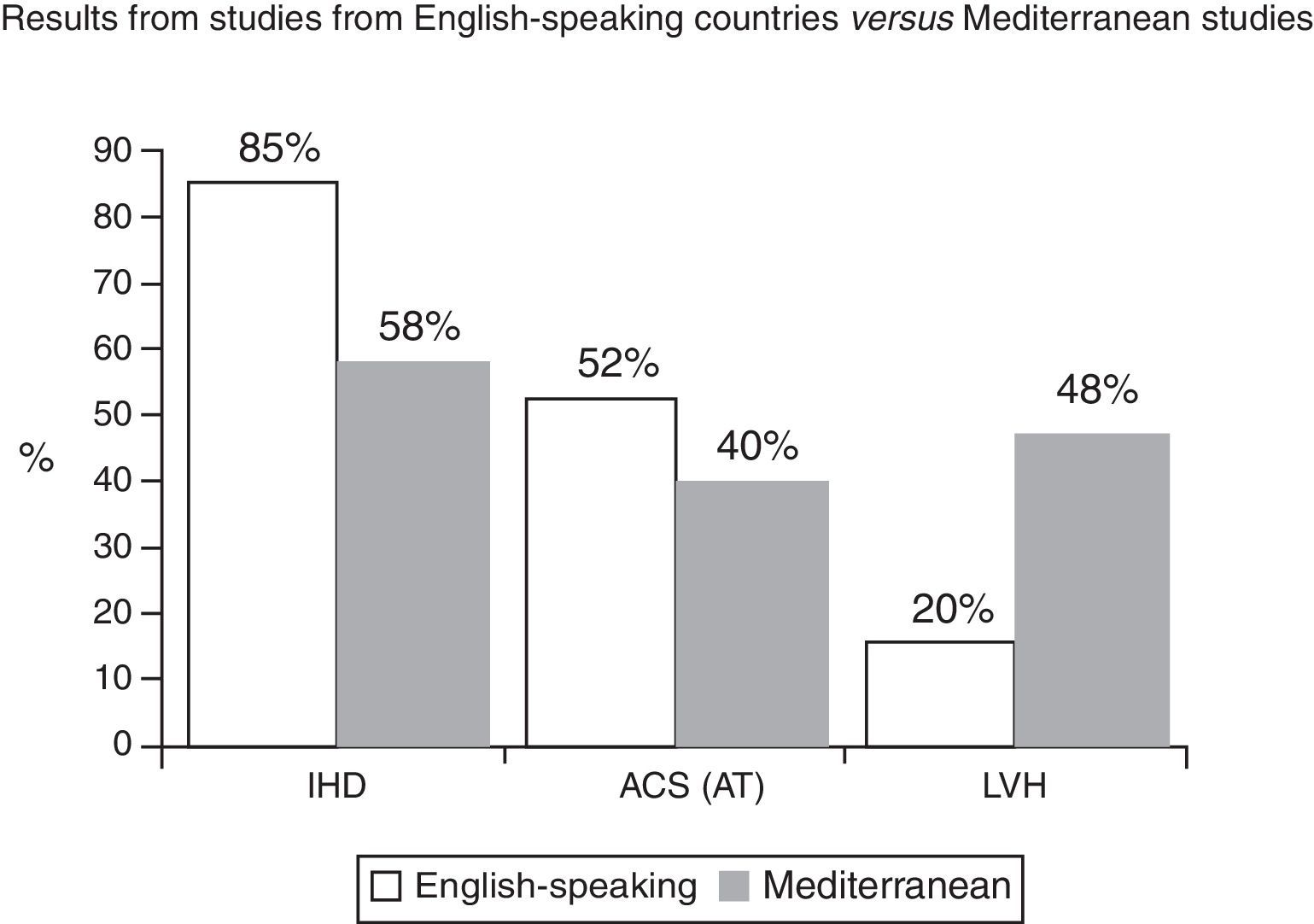
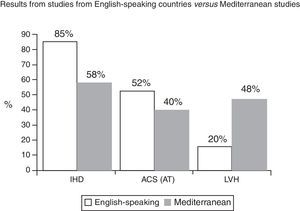
It is striking, when compared to similar studies in English-speaking countries,10 that the incidence of cases of IHD detected in the autopsy is lower (≈80–90% vs 58%) and that, within these cases, the incidence of acute thrombosis and pathological expression of acute MI is also lower (52% vs 40%) (Fig. 2). All of this is consistent with the already known evidence,1,3,4,11 that the incidence of IHD in Mediterranean countries is lower, which is probably related not only to the diet, but also to the overall way of life and to environmental aspects (Mediterranean culture). On the other hand, we have observed a greater number of SD cases which present left ventricular hypertrophy (48% vs 20%)9,12 (Fig. 2). From a clinical point of view and compared with the Maastricht study,13 SD victims from the EULALIA study presented fewer reports of angina pectoris history (20% vs 37%), which is consistent with the lower number of cases of IHD found in the autopsy. In our series, the incidence of possible associated inherited diseases was 3% of cases (hypertrophic and right ventricle arrhythmogenic cardiomyopathies) and no findings were found in the post-mortem in around 7% of cases. This suggests that some of them probably suffered a channelopathy.
Comparative study of the incidence of ischaemic heart disease (IHD), acute coronary syndrome with infarction: acute thrombosis (AT) and left ventricular hypertrophy (LVH).
Source: Taken from Subirana et al.7
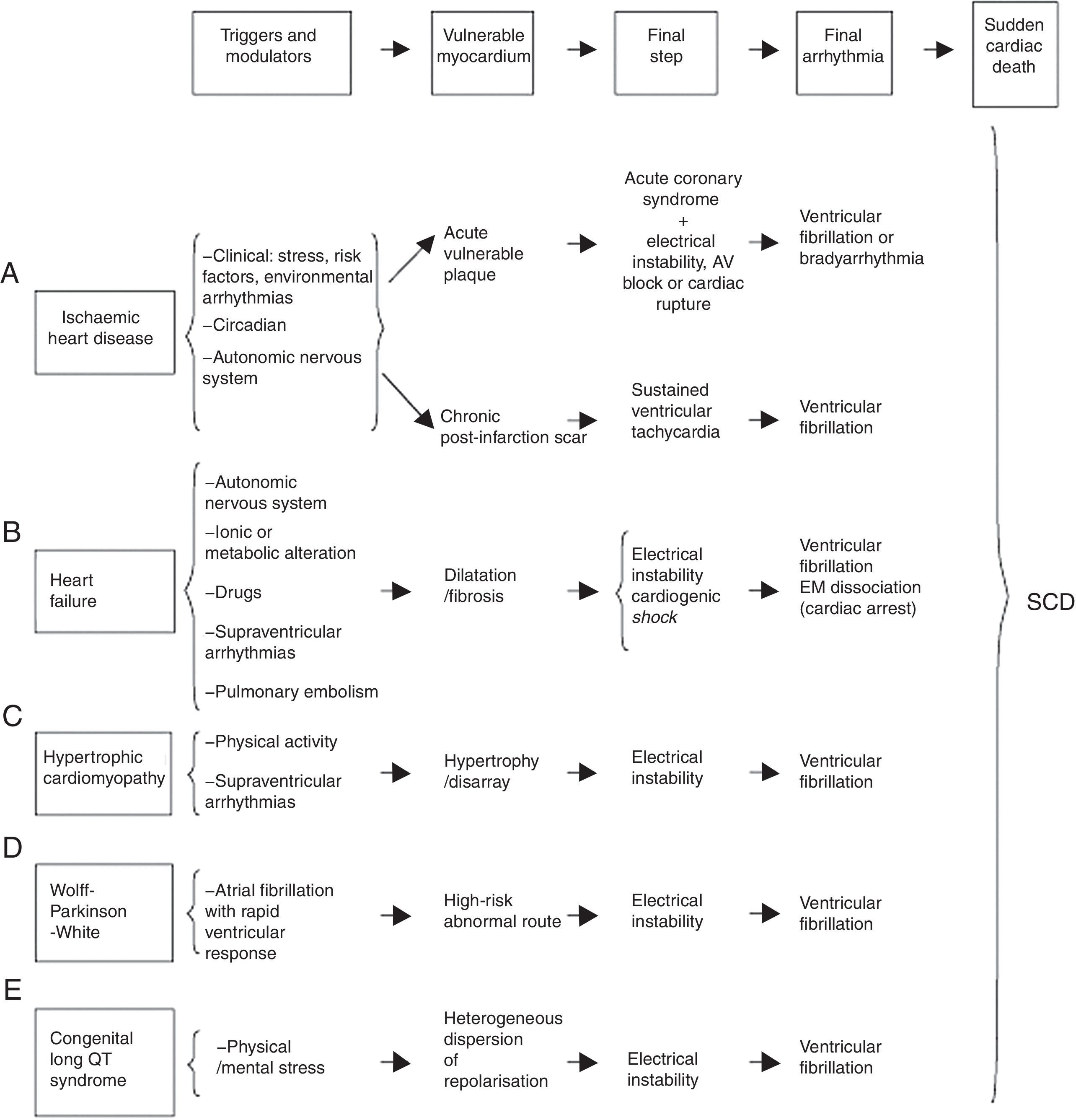
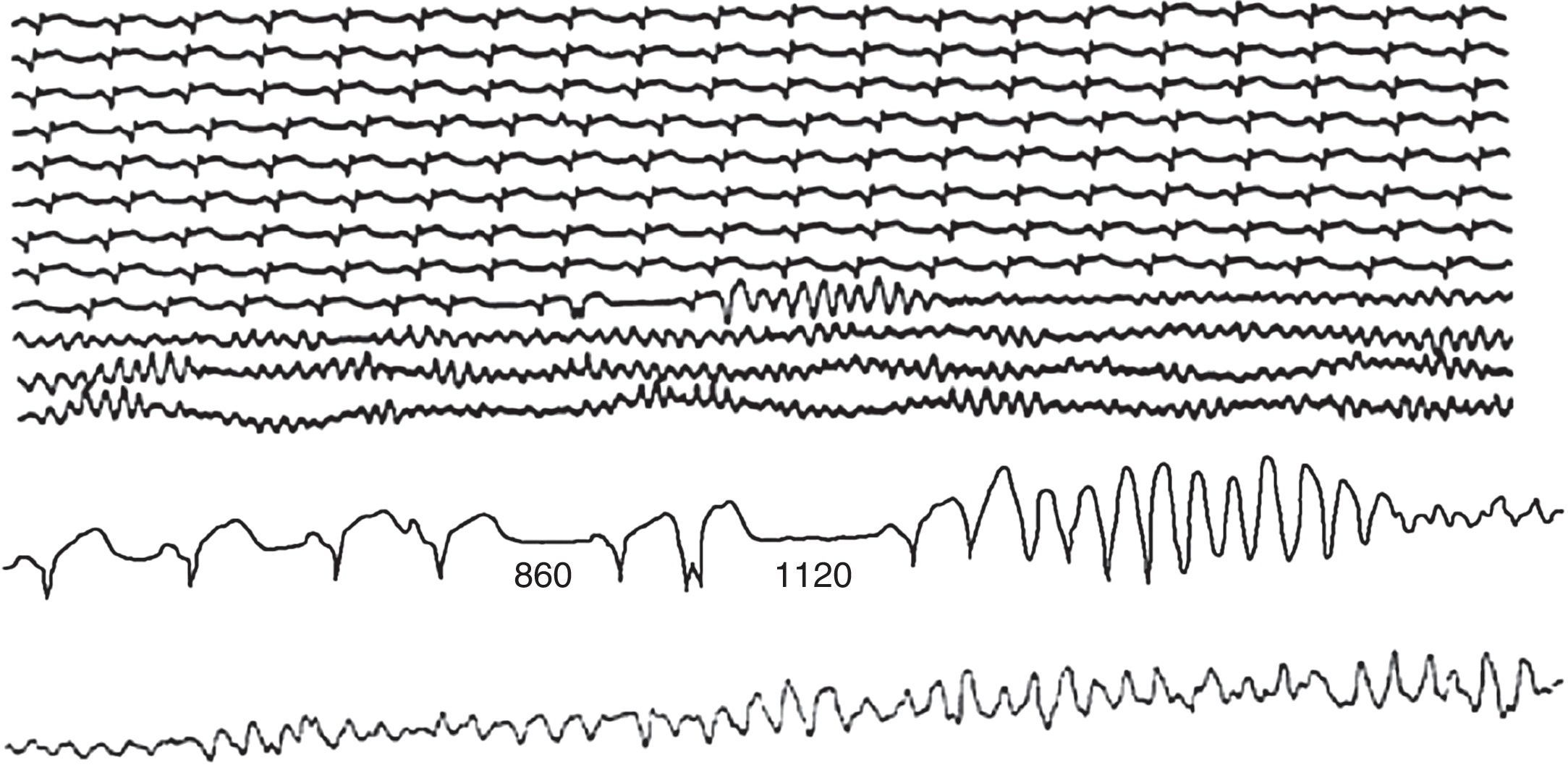
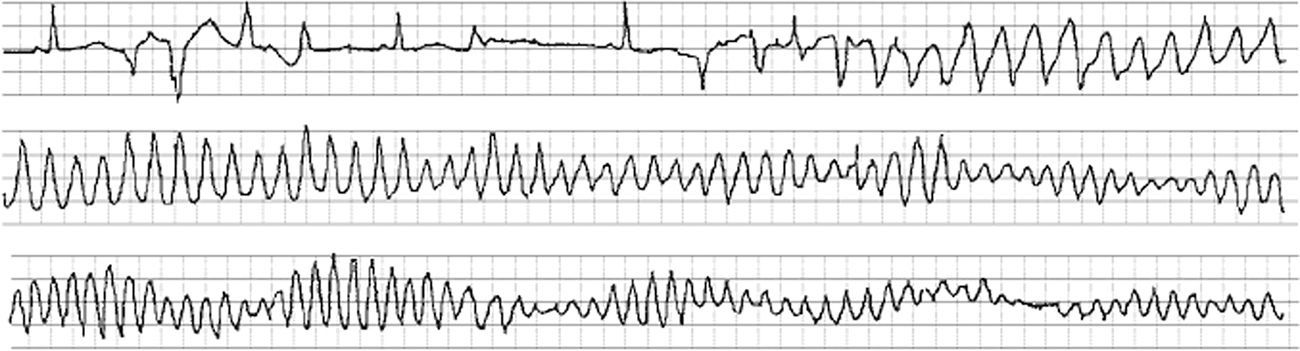
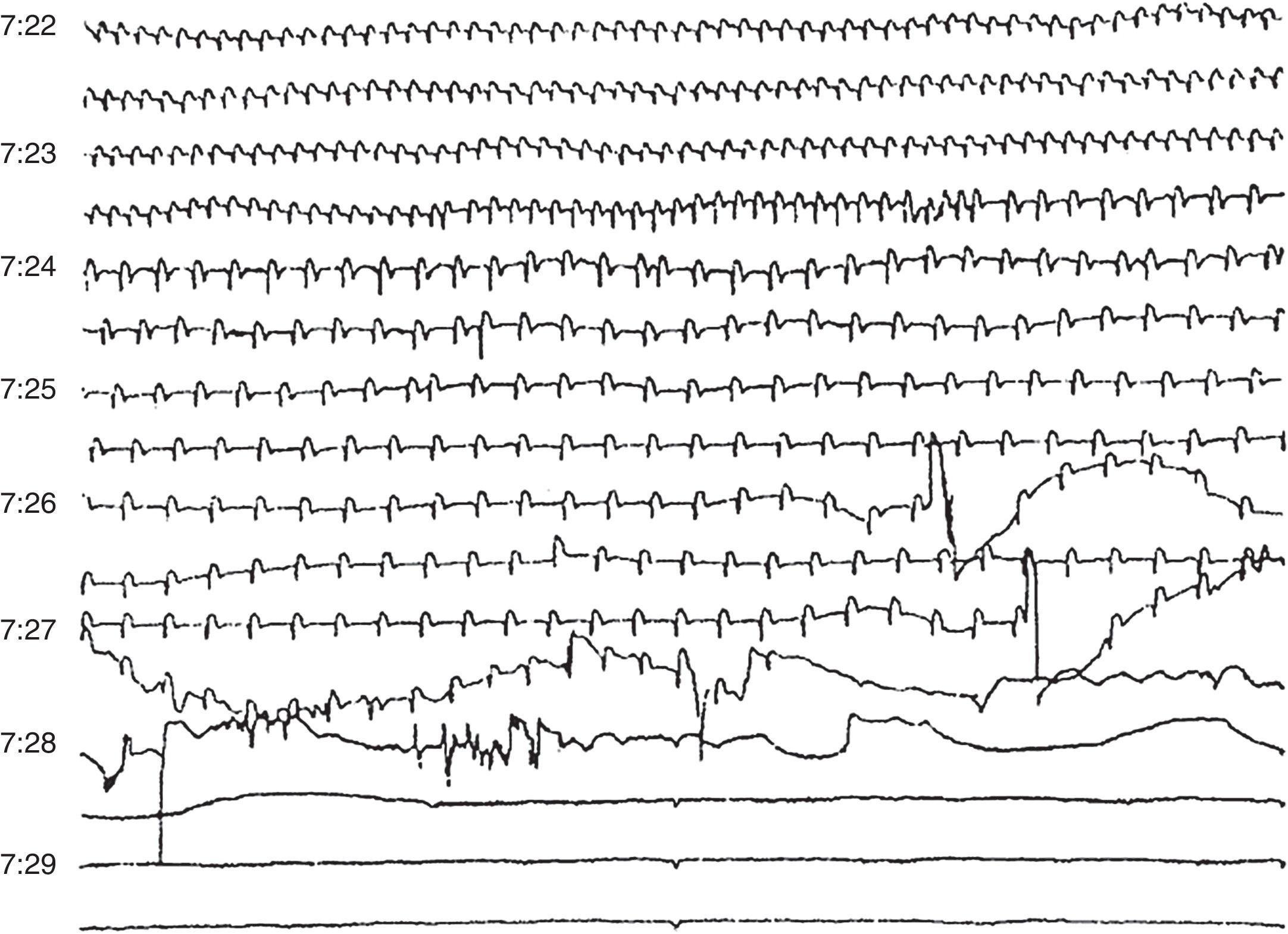
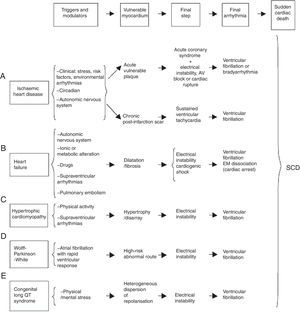
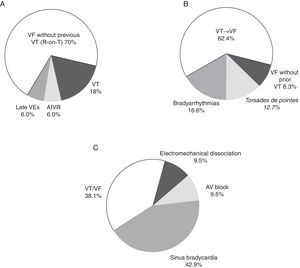
SD is the final stage in a chain of events leading to a cardiac arrest, in general, due to ventricular fibrillation (VF) or, less often, due to an extreme bradyarrhythmia.14 In all cases, there are a series of modulating or triggering factors which, acting on the vulnerable myocardium, precipitate SD. Fig. 3 shows how this chain of events occurs in different heart diseases. VF tends to be triggered by a premature ventricular contraction (PVC) in the presence of different modulating or triggering factors, among which an appropriate genetic and environmental setting, or the increase in sympathetic activity in relation to physical or mental stress should probably be included. Although this does not have consequences in normal situations, it could trigger SD in the presence of acute ischaemia (Fig. 4). VF is often triggered by sustained ventricular tachycardia (VT) (Fig. 5) or VT in torsades de pointes (Fig. 6). SD presents less frequently as a consequence of a bradyarrhythmia (Fig. 7).
Chain of events which precipitate sudden cardiac death (SCD) and parameters which the different diseases present in the different stages leading to SCD.
Source: Adapted from Bayés-Genís et al.14
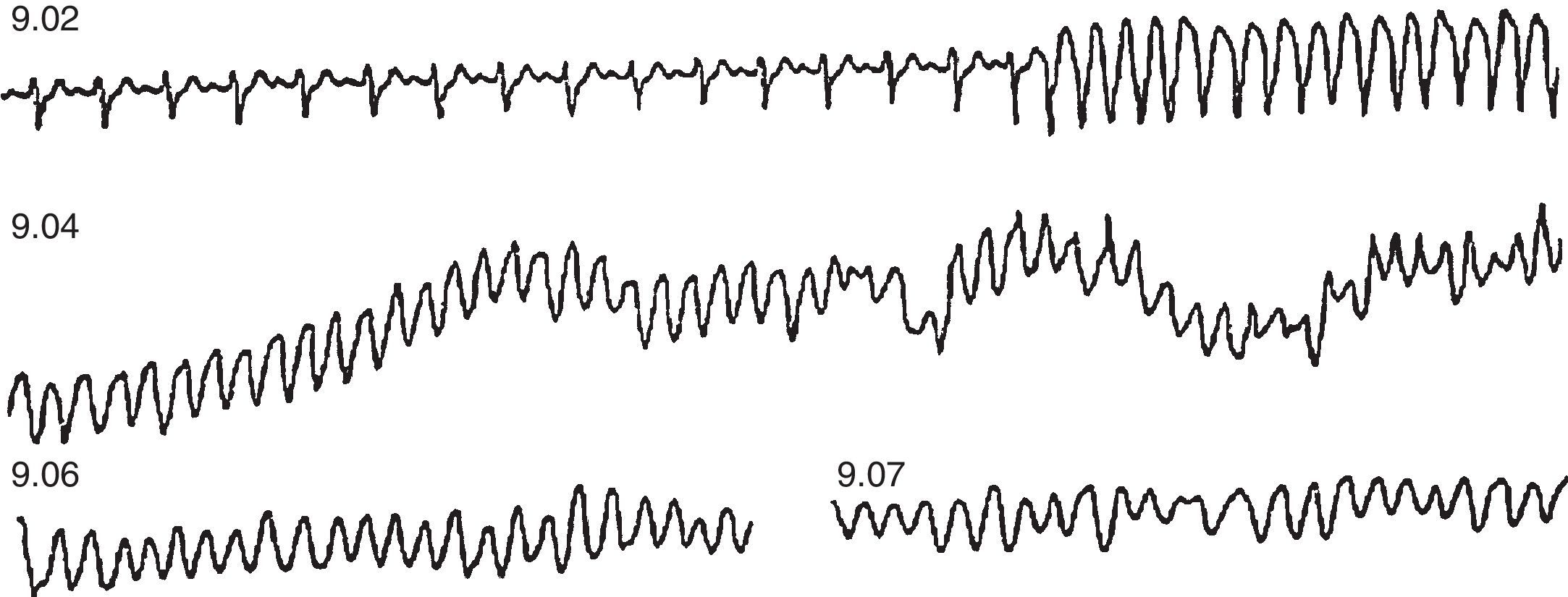
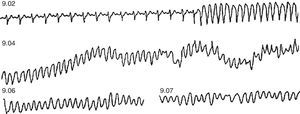
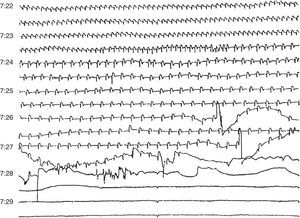
Outpatient sudden death from VF, of a coronary patient treated with amiodarone due to presenting frequent premature ventricular contractions. At 9.02 a.m., the patient suffered a sustained monomorphic VT, followed by a VF at 9.04 a.m. after an increased rhythm of the VT and a widening of the QRS complex.
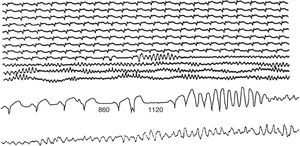
Outpatient sudden death from primary VF caused by ventricular extrasystole with short coupling interval, after post-extrasystolic pause (1.120ms) greater than the previous one, which had caused an isolated ventricular extrasystole. Note that the sequence of events started with an atrial extrasystole which caused the first shorter pause (860ms).
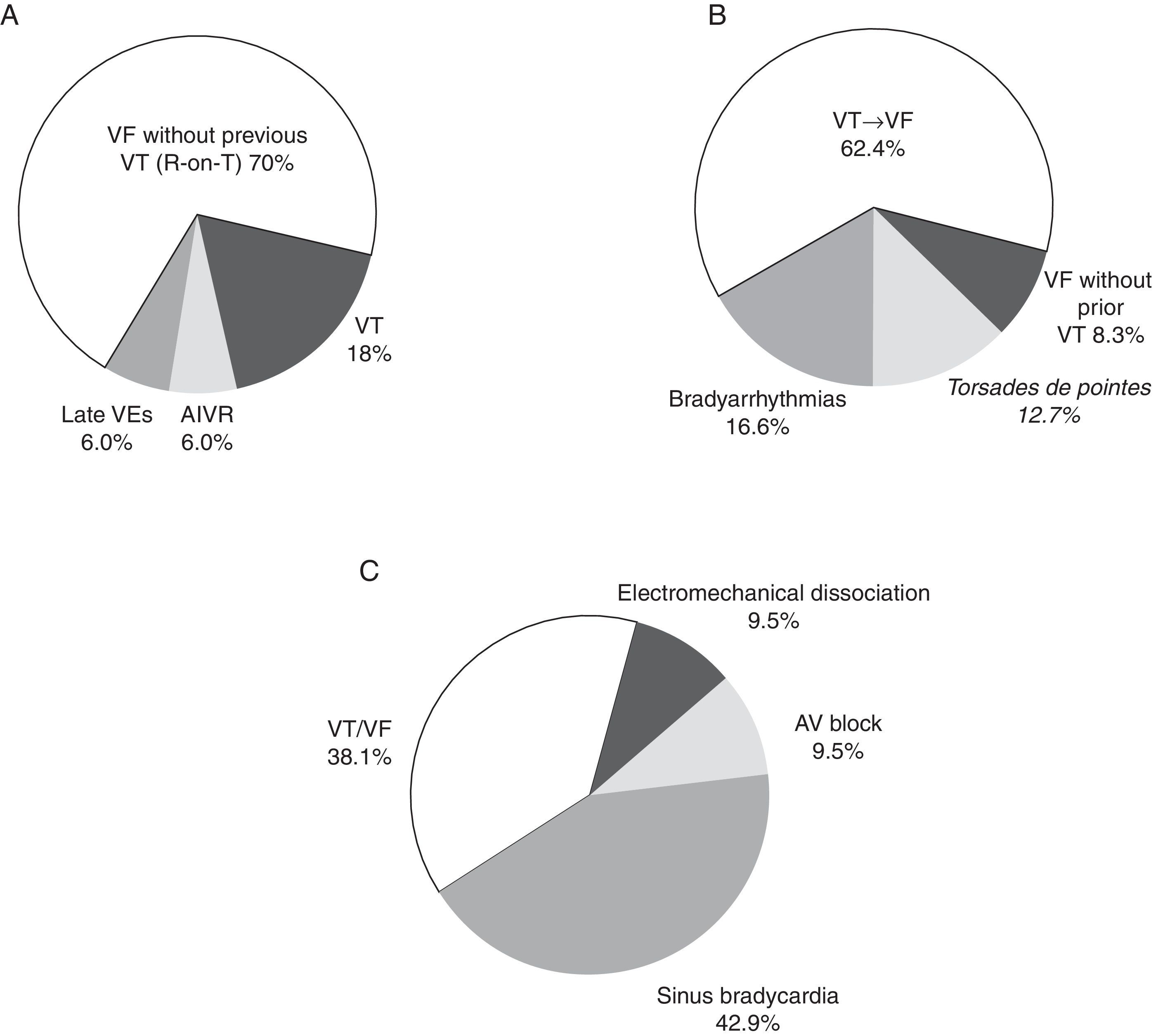
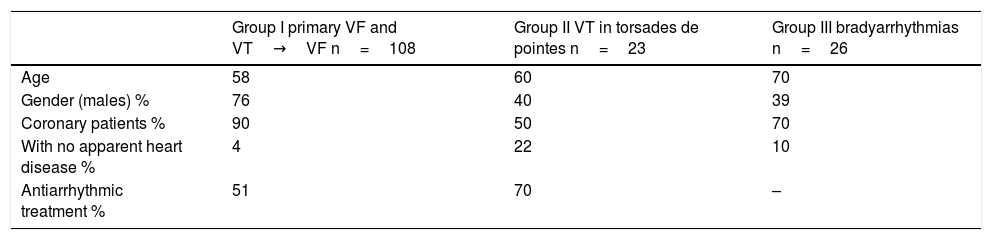
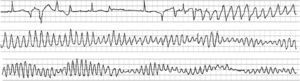
Final arrhythmias which precipitate SD are not always the same (Figs. 4–8). In a study, which we conducted, reviewing the tapes of 157 outpatients who died from SD while they were wearing a Holter monitor,15 we found (Fig. 8B and Table 2) that in two-thirds of the cases, the SD was due to a sustained VT which precipitated a VF, in general in the presence of a rapid baseline heart rate (sinus tachycardia or rapid atrial fibrillation), revealing an increase in sympathetic activity (Fig. 5). In contrast, VF not triggered by VT, which is often associated with acute IHD, is often presented as a consequence of a PVC with the R-on-T phenomenon. In our experience, in outpatients this pattern was observed in less than 10% of cases (Fig. 4). Curiously, in 13% of cases, SD was due to a VT in torsades de pointes which precipitated the VF. This generally occurred in patients without severe heart disease but who were taking class I antiarrhythmic drugs due to rare ventricular arrhythmias, often isolated PVCs (proarrhythmic effect). We believe that if this study was repeated now, the number of these cases would be much lower because there is evidence, from the CAST study,16 that type I antiarrhythmic drugs are dangerous, especially in patients with heart disease. Therefore, the prescription of class I antiarrhythmic drugs in post-acute myocardial infarction (post-AMI) patients is currently much lower. Lastly, when extreme bradyarrhythmia was the cause of SD (≈15% in our study) (Fig. 8B), it was due more to progressive depression of the sinus automatism and of the atrioventricular (AV) junction than to AV block (Fig. 7).
Clinical characteristics of patients who died suddenly while wearing a Holter monitor.
| Group I primary VF and VT→VF n=108 | Group II VT in torsades de pointes n=23 | Group III bradyarrhythmias n=26 | |
|---|---|---|---|
| Age | 58 | 60 | 70 |
| Gender (males) % | 76 | 40 | 39 |
| Coronary patients % | 90 | 50 | 70 |
| With no apparent heart disease % | 4 | 22 | 10 |
| Antiarrhythmic treatment % | 51 | 70 | – |
Fig. 8 shows the final arrhythmias which caused SD in patients with different clinical characteristics: (A) on route to the hospital, in a mobile coronary care unit with acute ischaemic symptoms17; (B) in outpatients (Holter monitor)15 and (C) in patients admitted due to severe HF.16 In the first case, a much higher number of cases of VF without prior VT was observed than in the group of outpatients in our study. This was certainly related to the fact that all patients in group A were in the acute phase of MI. In patients with advanced HF (group C), it was verified that there were many more cases of SD due to severe bradyarrhythmia. This could explain the ineffectiveness of antiarrhythmic drugs in preventing SD in patients with advanced HF. In our series (Fig. 8B), 80% of patients had a reduced ejection fraction, but their functional capacity was, in general, acceptable. These patients were too healthy to die, and many of these cases of SD could have been prevented with adequate treatment, which sometimes consists of not prescribing class I antiarrhythmic agents. We must remember the Hippocratic Oath: Primum non nocere (First, do no harm).
Our results were similar to those found in patients with an implantable cardioverter defibrillator with or without cardiac resynchronisation therapy. In this case, rapid VT also developed frequently and was treated with anti-tachycardia stimulation.18–20 On the other hand, in a small series of post-acute myocardial infarction patients with an ejection fraction below 40%, with an implantable loop recorder, who died suddenly, it was demonstrated that most cases of SD were due to primary VF not triggered by VT. However, the information on the clinical events around the time of the death was unknown. This lack of information and the reduced number of cases makes the comparison of these series with our results difficult. Furthermore, in most patients who died from different types of bradyarrhythmias, death occurred more than 1h after the onset of symptoms.21
Final considerationsTraditionally, forensic and legal medicine has undertaken the study of sudden cardiac death (SCD), along with other medical specialities. In recent years, several studies9 have underlined the importance of complementarity between different medical specialities, and the need for a multidisciplinary approach in order to tackle the problem correctly.22
Furthermore, the modernisation of forensic medicine in Spain currently allows for a study of SCD which offers homogeneous results. These results can contribute to an analysis of the clinical setting, and lead to forensic medicine and healthcare medicine interacting with each other, with an undeniable interest for public health.23 Therefore, an early diagnosis of the anatomical pathology results of deceased individuals, and the molecular analysis, are crucial to diagnose possible familial cardiomyopathies or channelopathies (e.g. Brugada syndrome) in order for correct prevention to be carried out in affected family members.24 There are multiple experiences of collaboration between medical examiners and cardiology specialists—such as the case of collaboration with physicians responsible for patients wearing an implantable cardioverter defibrillator—which can contribute to improving knowledge about these patients’ conditions, to detecting possible malfunctions in the devices and to optimising therapies.25
In this clear context of needing a multidisciplinary approach, we consider the coordination of healthcare services (hospital and primary care) with institutions of the Ministry of Justice, Justice departments of the autonomous communities and legal medicine and forensic science institutes, along with the responsible public health departments, to be necessary. This interrelationship would be very useful to determine the real incidence and to design SD prevention strategies, with regard to diagnostic methods, screening and immediate healthcare procedures in the event of an emergency situation occurring, as various authors have previously underlined.26,27 Likewise, it would also be desirable for the advisory bodies of both ministries (Health and Justice) to draft a comprehensive action plan which ensures the quality of post-mortem testing and the subsequent familial clinical and genetic testing.28
There are experiences of a multidisciplinary approach in areas such as Tarragona (Catalonia), which study the incidence and aetiology of SCD, integrating outpatient emergency departments and forensic and clinical sources (ReCapTa Study).29
Lastly, in the face of the common challenge of SD, we believe that it is necessary to create a national registry for cases of SD, funded by the health administration, in coordination with the Ministry of Justice and the autonomous communities competent in matters of Justice.30
Not forgetting the information programmes for citizens and the CPR training plans, it should be highlighted, within the prevention plans, that the use of semi-automatic defibrillators in public places is an important breakthrough as a treatment measure in cases of cardiac arrest. There is unanimity among most medical scientific societies that early defibrillation is the “key to survival”. The installation of defibrillator devices has become mainstream in non-professional sports venues and also in public places in Spain. However, Spain remains far behind other European countries such as Germany and France.31
Finally, it is important to emphasise again that, in the face of the most significant challenge in modern cardiology, the comprehensive collaboration of all individuals involved in the broad field of intervention in SD, starting with those who deal with the preventive side and ending with those who are in charge of the post-mortem diagnosis, is fundamental.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Bayés de Luna A, van-Roessel AM, Escobar-Robledo LA, Arimany-Manso J. Actualización de la muerte súbita cardiaca: epidemiología y estratificación del riesgo. Rev Esp Med Legal. 2018;44:5–12.