In Spain, more than 10% of road traffic accidents are legally deemed work-related accidents, with whiplash being one of the main resulting injuries. Nevertheless, despite its high incidence and socio-economic repercussions, there are very few studies of work-related whiplash in the literature. In this paper, we review a large sample of these cases with the aim of broadening our scarce knowledge of the subject, and to ascertain whether the profile of work-related whiplash differs from non-work-related whiplash.
Material and methodsWe studied 690 cases of whiplash deemed to be workplace accidents that were assessed and treated following a recently-published multiaxial protocol. The analysis extended to a review of the applicable literature.
ResultsThe results revealed several peculiarities in the work-related whiplash group, such as higher rates of sick leave for drivers and differing length of temporary disability according to profession or day of the accident. Some whiplash-related injuries, such as disc herniation, thoracic outlet syndrome or shoulder injuries, were associated with longer periods of temporary incapacity. A history of previous work-related accidents was also associated with longer sick leave.
ConclusionsWe emphasise the need to share the existing databases in order to identify the rate and repercussion of work-related whiplash compared to all road traffic accidents. Certain deficiencies were found, such as a lack of information, dispersion of the institutional databases and discrepancies between the available sources.
The relevance of postganglionic and extracervical conditions are underlined, together with disc herniation, in cases with longer clinical courses. A multiaxial model for diagnosing, treating and assessing work-related whiplash is proposed as a method to minimise sick leave, sequelae and to understand the singular profile of work-related whiplash.
En España más de un 10% de los accidentes de circulación tienen la consideración de accidentes de trabajo. Entre sus consecuencias un buen número son esguinces cervicales. Sin embargo, pese a su incidencia y repercusión socioeconómica existe poca literatura sobre el esguince cervical laboral. En el presente trabajo revisamos una extensa muestra de estos casos con el objetivo de aportar información sobre el tema, hasta ahora escasa, así como valorar si el perfil de los traumatismos cervicales menores laborales difiere de los no laborales.
Material y métodosSe analizan 690 casos de esguinces cervicales que tuvieron la consideración de accidente laboral, valorados y tratados según un protocolo multiaxial recientemente publicado. El análisis se extiende a la revisión de la literatura al respecto.
ResultadosLos resultados muestran particularidades en el grupo laboral, como cifras de baja laboral superiores en conductores, plazos de incapacidad temporal diferentes por profesiones o día del accidente. Algunas lesiones concurrentes como: hernia de disco, síndrome de encrucijada cervicotorácica y afección de hombro se asociaron a periodos de incapacidad temporal más prolongados. La existencia de accidentes laborales previos se asoció también a periodos de baja más dilatados.
ConclusionesSe enfatiza la necesidad de compartir las bases de datos existentes para identificar la incidencia y repercusión de los esguinces cervicales laborales dentro del total de accidentes de circulación. Se detectan algunas deficiencias como falta de información, dispersión de las bases institucionales y discrepancias entre las fuentes en la literatura. Se subraya la importancia de las enfermedades posganglionares y extracervicales, así como de la hernia discal en las evoluciones más prolongadas. Se resalta la utilidad del modelo multiaxial en el diagnóstico, tratamiento y valoración del esguince cervical para reducir el periodo de baja, las secuelas y también para entender la singularidad de los esguinces cervicales laborales.
Cervical strain (CS) is not an exclusively medical condition.1 Biological, psychological and legal2 factors, as well as associated3 and pre-existing conditions, have an impact on CS.
All this makes CS the perfect target for a multiaxial approach, both when assessing and treating the same. This approach considers different axes to determine the symptoms, to learn about the therapies available and to detect distorted or unreliable response styles.4–6
In Spain, we distinguish between several types of work-related cervical strain (WCS).
The first type includes accidents that occur on the way to and from work (CSTFW). The second type corresponds to accidents that occur in displacements during working hours due to occupational accidents (CSOA). The third type arises from “on-the-job” accidents; i.e., those that occur in displacements while completing a work-related task outside the workplace.
There are hardly any publications on the incidence and characteristics of WCSs in Spain. The few papers published to date are descriptive and do not include statistically significant analyses.7
This paper includes an extensive sample of WCSs, treated with a standard protocol of an insurance fund, with a view to providing information on the subject for healthcare, medical and legal purposes, and investigating possible differences in relation to non-work-related CSs.
Material and methodsAn analysis was performed of all diagnoses of road accident injuries taken from the database of a workers’ compensation insurance fund between 2010 and 2014. The healthcare coverage area of the fund included the entire national territory of Spain. Inclusion criteria included patients over the age of 18 years treated through this insurance fund for minor cervical trauma caused by an accident occurring on the way to and from work or during working hours. Exclusion criteria included multiple trauma, severe trauma disorders (fractures, dislocations, cranial trauma with Glasgow Coma Score of 13 or less) and traumatic shock. WCSs without sick leave were also excluded.
700 cases were obtained, discarding 10 owing to diagnostic doubts or lack of data. The final sample comprised 690 patients.
All patients were studied using a multiaxial protocol, considering the following axes6:
Axis I. Accident.
Axis II. Physical lesions of the cervical spine.
Axis III. Pre-existing condition.
Axis IV. Associated lesions outside the cervical spine.
Axis V. Psychological factors. Simulation-exaggeration.
According to this protocol, patients were received at A&E and referred to a rehabilitation unit, where they were diagnosed and treated as per the protocol cited. The diagnostic procedures depended on the patients’ clinical state, examinations and progression. They included screening for past and present cervical lesions and associated disorders. The tests performed were, depending on the case, one or more of the following: simple and dynamic radiography; magnetic resonance imaging (MRI) of the cervical spine; Doppler ultrasound of the supra-aortic trunks with thoracic outlet manoeuvres; electromyogram/electroneurogram; and MRI of other areas (shoulder, cervicothoracic junction).
Cases with conservative treatment failure were referred to neurosurgery.
Patients with suspected distorted or unreliable response style2 were referred to the fund's specific department for expert assessment of disabilities.
The following variables were collected: age, gender, medical history, associated disorders, location of accident, profession, days of sick leave, and final degree of work capacity.
Data were subjected to statistical analysis through descriptive study, analysis of variance and bivariate or multiple regression.
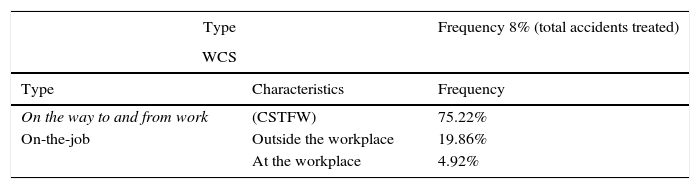
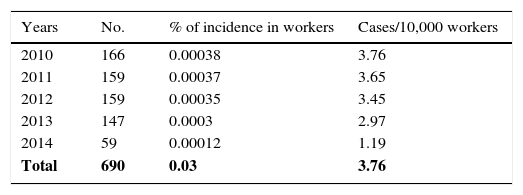
ResultsIncidenceThe total number of traffic accidents treated through the fund during this period was: 8.616. Our WCS sample (n=690) represents 8% of the total number of accidents treated (Table 1). The distribution of WCS by years and workers covered by the fund's healthcare is given in Table 2.
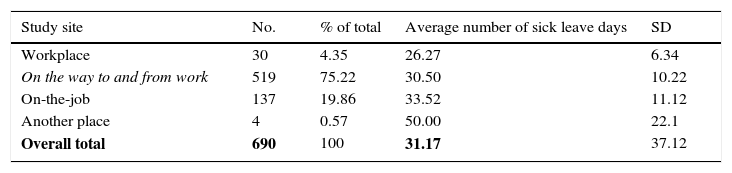
Most WCSs were classified as occurring on the way to and from work or “on-the-job” (75.22% and 19.86%, respectively). The rest occurred at the workplace (Table 1).
The mean age was 34.41 years, while 363 of the persons studied were women (52.61%) and 327 men (47.39%). The difference in age between genders was not significant.
The weekly incidence was a reflection of work activity, with accidents occurring less frequently during the weekend.
Temporary work disabilityThe risk of suffering a WCS with temporary work disability (TD) was 0.03–0.04% of workers (3.76 cases per 10,000) (Table 2).
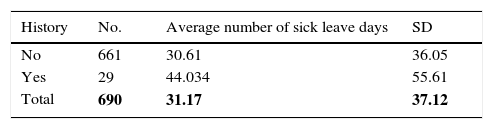
The mean number of TD days was 31.17 (SD: 37.12). The range was 1–447 days, the mean 23 and the mode 7.
Men had shorter mean TD than women (men: 29.35 days, SD: 40.82; women: 32.82 days, SD: 33.42), but this difference was not statistically significant.
One interesting fact was that the injured workers (n=38) had significantly higher mean TD on Saturdays than the rest of the days (20-day difference, p=0.0273; ANOVA).
History4.2% of the cases (n=29) had received treatment for previous trauma through the fund. The mean TD were higher in this group (14 more days) (ANOVA: p=0.046). There was no correlation between the mean days of TD in previous procedures and in the current CS (Table 3).
Location of accidentThe highest incidence of cases was accidents that occurred on the way to and from work (75.22%), followed by “on-the- job” (almost 25%). It should be noted that a small number of accidents occurred at the workplace, either on the premises or outside (4.35% and 0.57%, respectively) (Table 4).
Mean number of sick leave days according to the location of accident.
| Study site | No. | % of total | Average number of sick leave days | SD |
|---|---|---|---|---|
| Workplace | 30 | 4.35 | 26.27 | 6.34 |
| On the way to and from work | 519 | 75.22 | 30.50 | 10.22 |
| On-the-job | 137 | 19.86 | 33.52 | 11.12 |
| Another place | 4 | 0.57 | 50.00 | 22.1 |
| Overall total | 690 | 100 | 31.17 | 37.12 |
Total numbers in bold.
No statistically significant differences were found in the TD means according to the location of accident (Table 4).
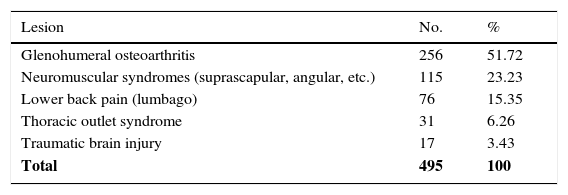
Associated lesionsThere were 495 associated extracervical lesions at a rate of 0.71; i.e., slightly fewer than one lesion per case. The types of lesion are summarised in Table 5.
Lesions associated with CS.
| Lesion | No. | % |
|---|---|---|
| Glenohumeral osteoarthritis | 256 | 51.72 |
| Neuromuscular syndromes (suprascapular, angular, etc.) | 115 | 23.23 |
| Lower back pain (lumbago) | 76 | 15.35 |
| Thoracic outlet syndrome | 31 | 6.26 |
| Traumatic brain injury | 17 | 3.43 |
| Total | 495 | 100 |
| Disorders responsible for stabilisation times greater than 180 days | |||
|---|---|---|---|
| Disease | No. | % of total | %>180 |
| Abnormal response style | 12 | 1.74 | 26.08 |
| Cervicothoracic junction disorder | 11 | 1.59 | 23.91 |
| Other | 9 | 1.30 | 19.56 |
| Shoulder disorder | 6 | 0.87 | 13.04 |
| Herniated disc | 5 | 0.72 | 10.86 |
| Pre-existing condition | 3 | 0.43 | 6.52 |
| Total | 46 | 6.67 | 100 |
Total numbers in bold.
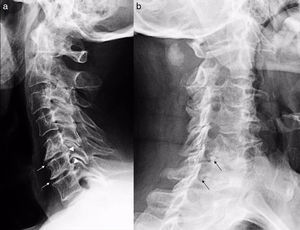
In 37 patients the duration of the TD was greater than 3 months. 46 associated disorders were identified in this group. Disc herniation was treated in some patients (n=5; surgery=4) (Table 5 and Fig. 1). Others experienced a shoulder injury (periarthritis, rotator cuff tears, etc.) (6 patients). Another group suffered from thoracic outlet syndrome (TOS) (n=11) (Fig. 2). Others had cervical osteoarthritis as a pre-existing condition. The latter group suffered from more frequent dizziness and headaches (n=3) (Figs. 3 and 4).
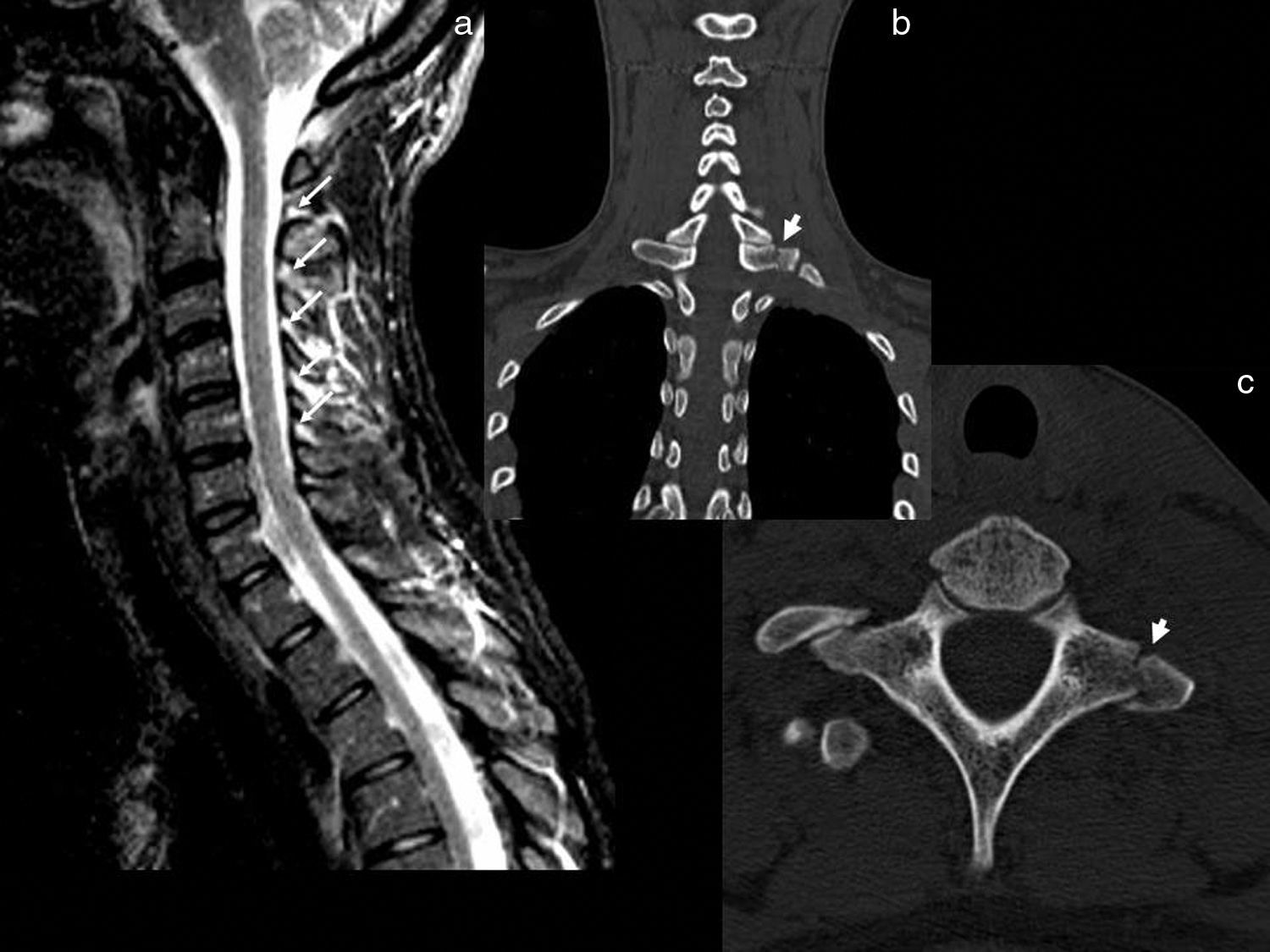
Acute disc herniation after traffic accident with initially minor trauma. The patient progressively developed left cervicobrachialgia and was diagnosed with a herniated disc 3 weeks after the accident (arrows in a and c). The central image (b) corresponds to the postoperative control X-ray. An intersomatic cage in C5–C6 is visible due to the radiopaque markers (arrowheads in b).
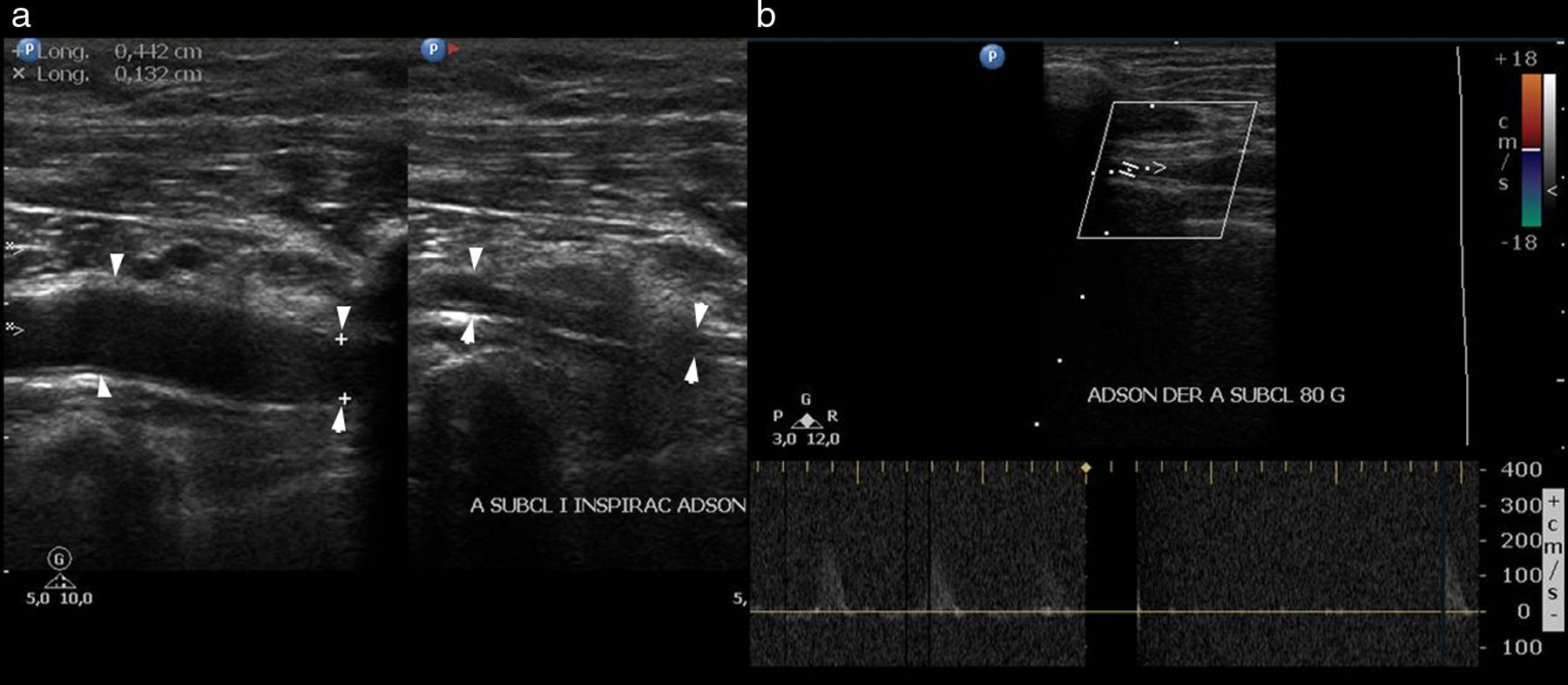
Doppler ultrasound of the supra-aortic trunks with thoracic outlet manoeuvres. Note the morphologically arterial compression (arrows in a, which show reduced breathing) and in the Doppler ultrasound of the subclavian arteries, with Adson's manoeuvre (loss of the pulse in b with abduction, extension and external rotation of the shoulder). This lesion, associated with or aggravated by CS, often goes unnoticed, unless tests such as Doppler ultrasound are performed with this type of manoeuvre.
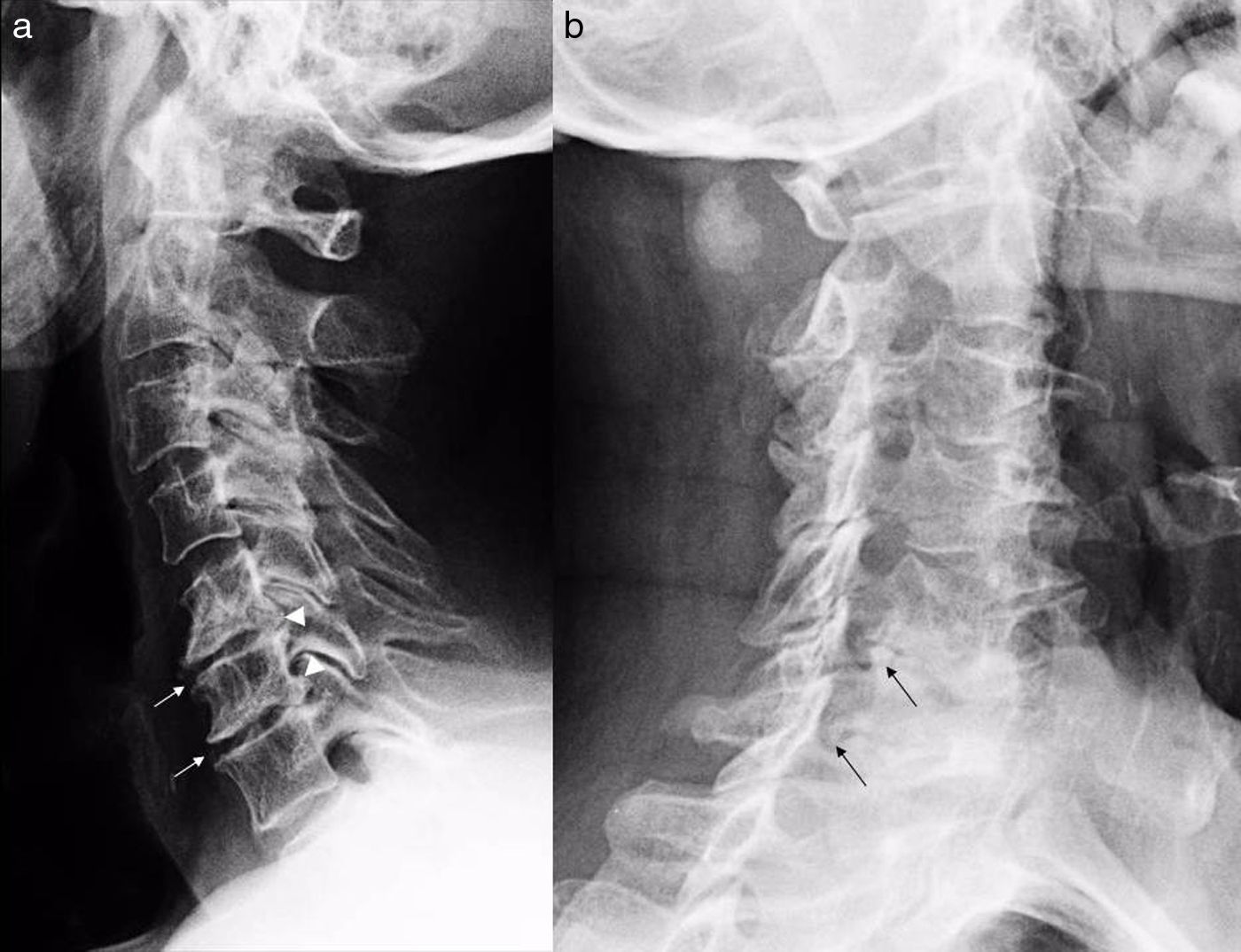
Patient with CS with minimal strain energy who, however, developed symptoms that lasted more than 3 months (cervicobrachialgia and dizziness). The image shows a rigid block (C5–C6–C7) secondary to osteoarthritis (see anterior osteophytes: arrows in “a”, and posterior osteophytes: arrowheads in “a”). Osteophyte stenosis at the intervertebral foramina can be seen in “b” (arrows). In our series, the existence of osteoarthritis with rigid blocks was associated with longer progression and headaches.
Patient with CS and extension of the stabilisation period beyond 2 months. The existence of a pre-existing condition is emphasised (osteophytes: arrow in a), as well as signs of redundant posterior ligaments (thick arrows in b) and redundant discs in C4–C5, C5–C6 and C6–C7. Note the anterior disc extension (thin arrows in b). In our series, longer periods of sick leave were associated with signs of a previous pathological condition.
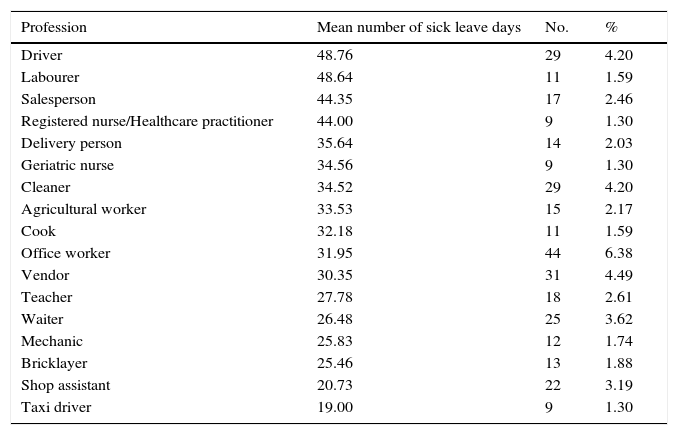
The professionals with the highest incidence of WCS were: administrative, sales and cleaning personnel (Table 6).
Distribution of average number of sick leave days by profession.
| Profession | Mean number of sick leave days | No. | % |
|---|---|---|---|
| Driver | 48.76 | 29 | 4.20 |
| Labourer | 48.64 | 11 | 1.59 |
| Salesperson | 44.35 | 17 | 2.46 |
| Registered nurse/Healthcare practitioner | 44.00 | 9 | 1.30 |
| Delivery person | 35.64 | 14 | 2.03 |
| Geriatric nurse | 34.56 | 9 | 1.30 |
| Cleaner | 34.52 | 29 | 4.20 |
| Agricultural worker | 33.53 | 15 | 2.17 |
| Cook | 32.18 | 11 | 1.59 |
| Office worker | 31.95 | 44 | 6.38 |
| Vendor | 30.35 | 31 | 4.49 |
| Teacher | 27.78 | 18 | 2.61 |
| Waiter | 26.48 | 25 | 3.62 |
| Mechanic | 25.83 | 12 | 1.74 |
| Bricklayer | 25.46 | 13 | 1.88 |
| Shop assistant | 20.73 | 22 | 3.19 |
| Taxi driver | 19.00 | 9 | 1.30 |
| Professional categories and duration of sick leave | ||
|---|---|---|
| Groups | Difference of mean number of recovery days | ANOVA |
| Driver vs non-driver | 17.16 | (p=0.023) |
| Driver vs waiter | 22.27 | (p<0.05) |
| Driver vs taxi driver | 29.75 | (p<0.05) |
| Driver vs shop assistant | 28.03 | (p<0.05) |
In drivers (non-commercial vehicles only) (n=29, 4.2%), the mean TD was higher than the other professions (49 days). However, in taxi drivers (n=9; 1.30%) the mean TD was 19 days (29.75 fewer days than in all other drivers).
Some health professions (nursing) had higher mean TD than the other professions (44 days). The same was true for with sales personnel and labourers (48.64 days).
DisabilitiesIn our setting, WCSs had a low incidence of permanent disabilities. There were only 3 cases with total permanent disability (TPD), 2 with herniated discs and one with vertigo incompatible with the worker's profession. More than 99% returned to work.
Thus, for the purpose of returning to work, the vast majority of patients were considered to be cured without sequelae. The sequelae provided for in Spanish Royal Decree No 8/2004 or in Act No 35/2015 are not included in the work environment, owing to which no data can be offered in this regard.
Psychological axis and unreliable response styleSome cases presented with symptoms of the psychological axis: post-traumatic stress disorder, depression or simulation (12 patients in total). Only in one case were the symptoms classified as true simulation.2
Delays in diagnosis or treatmentLastly, 9 patients out of 37 with stabilisation periods in excess of 3 months had no associated lesions. Significant delays in diagnosis or treatment were observed in these cases.
DiscussionIn Spain, 471,223 work-related accidents with TD were reported in 2012. Of these, 408,537 occurred at work and 62,686 on the way to and from work (86.7% and 13.3% of the total, respectively).8 Taking into account that the number of National Insurance members at the time was 14,340,000, the annual incidence of traffic accidents considered as accidents occurring on the way to and from work with TD would be 4 accidents per 1000 workers.
However, these figures do not report on other traffic accidents not occurring on the way to and from work. Nor can it be ascertained how many of those classified as “during working hours” are traffic accidents.
A number of studies indicate that, of the total number of traffic accidents in Spain, those occurring on the way to and from work account for 7.1–9.28% of the total.7,9 Since we know that the incidence of work-related traffic accidents reaches 10.76% of all traffic accidents,9 it could be deduced that 1–3% of traffic accidents correspond to travel during working hours.8
Nonetheless, these are indirect deductions based on published sources, without it being possible to confirm the exact incidence of traffic accidents occurring during working hours. Nor do we know how many traffic accidents occur at the workplace or while performing a task outside the workplace.
Therefore, one of the main conclusions of our study is that we do not have detailed and reliable figures on the actual incidence of different types of traffic accident considered as work-related accidents. Each publication contemplates a section of them, but none provides information on the incidence of each subtype (on the way to and from work, on-the-job, while performing a task outside the workplace, or at the workplace itself). This may be a shortcoming in the design of preventive policies for traffic accidents, as it does not allow these measures to be adjusted to the specific type of accident.
In Spain, most work-related motor accidents occurred on the way to and from work or during working hours (75.22% and 19.86%, respectively). 4.92% of traffic accidents occur at the workplace (Table 4). This group is rarely mentioned in the literature and may go unnoticed in a non-detailed study; hence, more information about these cases is needed.
The incidence of CS is around 12% of all traffic accidents.10 Our study shows that work-related cases with sick leave account for 8% of the total number of traffic accidents treated, which is in line with the overall incidence of CS. However, other data also from insurance funds have indicated a higher frequency (55.10%).11
The incidence of CS with sick leave in our sample was in the region of 0.04% of the total number of workers. That is to say: 0.37/1000 workers. These figures are lower than those of other studies on workforce treated through an insurance fund, which cite 1.5–2 cases per 1000 workers.7
The reasons for this discrepancy may be due to the nature of the samples. One of the most detailed studies analyses a sample 10 times smaller than ours; it includes only 2 years, compared with the 4.5 years in our study, and considers accidents with and without sick leave.7
It has been noted that around one third (31.2%) of CS cases in the general population do not require sick leave. This may explain why we found lower incidence rates. According to our data, we could estimate, therefore, that around 3.7 workers/10,000 are treated annually through an insurance fund for CS caused by work-related traffic accidents, for which they require sick leave.
None of these figures shows the incidence of work-related CS in the sub-population of traffic accident victims. The published data only allow for partial estimates, and the information provided by insurance funds shows discrepancies among said bodies.
There is therefore a lack of cooperation between traffic accident databases and those which, in the main from insurance funds (but also the public health system), include work-related accidents. One of the main conclusions of this paper is that progress needs to be made in this area to facilitate the creation of common databases or interaction between existing ones.
The incidence figures by gender in our study are similar to those in the literature for general CS,12 although female predominance is not as pronounced as in non-work-related strains (52.6% vs 54–57%, respectively). Moreover, this difference was not statistically significant. This implies a particularity of work-related CS in relation to non-work-related CS, in which there is a greater incidence in women. The injury stabilisation period was longer in women (29.35 vs 32.82 days), but it was not statistically significant either.
A number of studies have linked age to recovery from CS, attributing worse expectations of recovery after the age of 40.13 Others point out that there is a lower risk of CS after the age of 65.10 Age played no significant role in stabilisation periods in our series, probably as our population was predominantly young (18–63 years). We do not know whether other variables, such as regular physical activity, or work aspects, such as better health control, may explain this finding, which is also different from non-work-related strain.
A further difference in relation to non-work-related strain is the day of the accident. The incidence we found is lower at weekends, as might be expected, given the reduced work activity. One relevant fact is that accidents occurring on Saturdays had higher TD means than for all the other days. We have found no data in the literature with which to compare this finding. Pastor points out that Tuesday and Wednesday include more strain, although the mean number sick leave days is not cited.7 It would therefore be useful to study the subgroup of work-related traffic accidents occurring on Saturdays to assess, among other aspects, the role of factors such as unfavourable working conditions (shift work, job insecurity, etc.). More studies are needed to clarify the validity of this finding.
The mean TD duration in our study was 31.17 days. The application of the multiaxial model could justify this short duration compared with that of general CS, as at our fund the mean TD for CS in 2006–2009 was 36.79 days and, after applying this system, the figures were reduced even further.
The mean TD in the literature varies. The figures of similar studies in the workplace are close to ours.7,11 Other studies on CS (work-related and non-work-related) showed longer stabilisation means (52.78 days). It has been mentioned that when follow-up is carried out through the public health system or an insurance fund, the number of days on sick leave is lower. Thus, if the follow-up is carried out through the public health system, the average number of days of incapacity is 43.19 days, 54.37 days if it is carried out through an insurance fund, 58.01 if it is private and 68.06 if it is mixed: public–private).12 As we can see, the mean TD periods in our study and other similar ones coincide, at around 1.5 months.
A number of studies have found that in non-work-related CS, the percentage of those taking more than 12 weeks’ sick leave is around 4.9%,14 while others indicate that up to 50% of patients have not returned after a period of 6 months.15 We found the percentage of patients who had not recovered at 12 weeks to be 19.4% (n=37).
We also identified shorter periods of sick leave than those of non-work-related strain. The multiaxial model, the specialised assessment, the distinction between attending physicians and experts, the rapidity in additional tests, and the early and continuous use of rehabilitative treatments16 are probably the reasons for this shorter duration.
Regarding the type of work, it has been pointed out that professions such as secretarial ones have shorter periods of sick leave than heavy industry.17 It has also been shown that the prolongation of recovery beyond 6 months does not depend on social class, type of work or nature of the trauma.14
Nonetheless, in our sample the type of work does seem to result in variations in the duration of TD. Thus, drivers have significantly longer TD periods than the rest of the professions. Some studies show longer periods in long-distance drivers, although the data cannot be extrapolated to western countries.18
We also found significant differences within the group of drivers. One of the most striking was that the profession of taxi driver has significantly shorter TD periods than the so-called “drivers” group. This is probably because the group includes a great number of freelancers, for whom there is much less incentive to prolong their sick leave than for the rest. It is known that the existence of paid leave can have a bearing on how quickly people return to work.14
On the other hand, it would seem logical to think that, given their greater exposure to these types of injury and longer TD periods, professions related to driving are the group that could benefit the most from preventive actions aimed at controlling their health and preventing accidents. It is therefore worthwhile reviewing the actions taken in this area.
It has also been argued that a low level of education, low income, unemployment, or less skilled or blue-collar jobs are predictors of a greater impairment of the patient's ability to work.19,20 This may also be of interest when developing preventive measures and actions.
It has also been pointed out that the longest injury stabilisation periods are those of housewives.12 Our study does not include them, which may have a bearing on the comparison of TD with other professions.
Some accidental variables are factors that prolong TD. In our study, we did not include variables of axis I (accident), although its characteristics are summarised in all cases. This generally enables us to estimate the extent thereof. A number of authors have indicated that the damage sustained by a vehicle is related to treatment duration.21 Others point out that the vehicle being parked and not being responsible for the accident are elements that prolong duration and worsen the prognosis.22
The above factors (axis III) are indicators of poor progression. Periods of sick leave of between one and 18 weeks within a 5-year period before a collision doubles the risk of long-term cervical pain after an accident.19 Some studies indicate that having a medical history reduces the ability to work after CS.23 Others confirm this fact, highlighting the role of previous psychological history as a factor leading to a worse prognosis.17 It has been argued that sociodemographic factors, previous psychological history and post-traumatic stress disorder impair post-whiplash quality of life.24 Dorado et al.12 show that the existence of these factors increases the injury stabilisation period and sequelae.
Our study confirms that the existence of previous factors with sick leave is also a risk factor for TD prolongation in work-related CS. This emphasises the importance of pre-existing conditions as capable of aggravating the progression of a CS. It is not clear whether this arises from previous experience or greater bio-psychological vulnerability resulting from pre-existing conditions.
Associated injuries play an important role in the increase of TD and sequelae. Postganglionic (cervicothoracic junction disorder, neuromuscular disorders) or shoulder lesions may go undiagnosed, being attributed erroneously to intracervical disorder. The association of extracervical disorder with CS reached 52.6%.24
Our study highlights the importance of identifying and treating these associated lesions, as incidence thereof is highly significant and patients suffering from them have higher TD rates than the rest. Perhaps the kinetics of the accident should be reviewed in these cases, as attention is often paid only to the biomechanics of the neck, whereas CS behaves more like shoulder-girdle syndrome.
It is possible, for example, that the incidence of cervicothoracic junction disorder in association with, or as a consequence of, CS is underestimated.3 The same could occur with skip spinal injuries.25 Lower back pain, for example, is associated with CS in 13.2%.25 Our figures for these disorders are similar to those published and they stress the need to pay attention to these concurrent, often undervalued, injuries.
Dorado indicates a 5.2% incidence for disc herniation or protrusion due to CS. Other sources have found frequencies of 3.4%.26 Our figures were similar (22 patients [3.18%], 5 of whom had TD values above 180 days). Our paper included a large number of professional drivers at a high risk of degenerative disc disease.27 Our study confirms that herniated discs have an impact on poor progression and influence the existence of disabilities in work-related CS.
Neurosurgical assessment is therefore an element to be considered in these cases.
Regarding sequelae, it is said that, after one year of CS, around 56% of patients reported not having recovered their health condition. 31% reported that pain had an impact on their work.28
Although our study is not aimed at assessing sequelae, it is worth noting the high rate of return to work, which is probably indicative of a very low impact of sequelae on patients’ work-related activities. Sequelae of this type are not usually considered in the work environment, unless their impact on the subject's activity is relevant.
The problem with CS sequelae is that many are subjective, and the studies are based on questionnaires filled out by patients (self report type) after the accident.29
For this reason, we believe it is essential to distinguish between experts and attending physicians. All the cases in our study that presented with progression or sequelae and were unsupported by objective findings were analysed by a department that performs case-by-case assessments and is not related to healthcare. This department conducts biomechanical analysis that provides objective information on the spine.
This system probably ensures that subjective sequelae are not considered, unless they are supported by objective elements, and this analysis was carried out by professionals not involved in healthcare.
The new injury compensation scale seems to run along the same lines when compensating CSs as temporary injuries. In fact, a comprehensive medical report is required for assessing sequelae.30 The attending physician is obliged to treat the patients’ subjective complaints; nonetheless, in terms of value, what matters is the objectification or not of subjective sequelae.
The need for a clear distinction between the role of attending physicians and experts has been emphasised.31 These same studies conducted in different European countries highlight the importance of applying objective criteria, both to the analysis and the causality of CS. This can only be done when specialists with experience in the field treat and assess CS in a way that is independent of the medical and legal assessment of the case.
The results of our study indicate that the so-called WCS sequelae (subjective in their majority) have little or no objective impact on the patients’ work when they are analysed by experts who are not related to healthcare.
Finally, the need for specialised assessment of CS should be emphasised. Many injuries go unnoticed as many patients are not assessed by specialists. The new Law 35/2015,30 which is fairly restrictive as far as CS is concerned, is nevertheless highly specific when requesting a conclusive medical report to assess the sequelae of CS, without allowing for compensation of CS alone as a temporary injury. Although the purpose of this paper is not to analyse sequelae according to the scale of this law, many of our cases, after expert radiological and neurosurgical assessment, involve associated disorders that go beyond minor cervical trauma and, therefore, alter the consideration of CS from what is provided for in the new law. This law considers that minor cervical trauma cannot be confirmed by means of additional tests. Our experience in the analysis of associated injuries is that, if an expert analysis of these tests is conducted, injuries are often found that confirm the existence of trauma and are, therefore, not minor trauma in the strict sense of the term (Fig. 5). Consequently, we believe that our results can be useful both in the work-related assessment of sequelae and TD periods, and in the classification of minor cervical trauma pursuant to Act No 35/2015.
Patient diagnosed with mild cervical symptoms who was assessed by us at 3 weeks for persistent pain. MRI (a) shows oedema in the STIR sequence of the C3–C6 interspinous ligaments (arrows). A subsequent CT scan revealed the existence of transverse fractures in C7 and D1 (arrows in b and c). This case emphasises the need for specialised assessment of CSs.
It should be stressed that, consistent with the provisions of the new law on the need for conclusive medical reports to confirm existing sequelae, in these cases a high degree of specialisation is required and opinions must be requested by accredited professionals.
ConclusionsWCS can be distinguished from non-work-related CS due to epidemiological particularities. It also involves shorter injury stabilisation periods and fewer sequelae, and depends on different care methods and demographic variables.
There is a lack of epidemiological data to help determine the actual incidence of work-related traffic accidents and their subtypes (on the way to and from work, on-the-job or at the workplace). This can hinder the adoption of preventive measures based on data that combine various types.
The adoption of multiaxial diagnostic and healthcare protocols in specialised areas results in the reduction of stabilisation periods for CS. This methodology, along with the distinction between attending physicians and experts, shortens the medical and legal parameters of physical injury compared with non-work-related strain.
Some professions, such as driving, show higher stabilisation figures than the rest. This group is likely to adopt therapeutic or training measures that could reduce the impact of WCS.
Differences in the injury assessment parameters used for WCS and non-work-related CS reinforce the concept of WCS as a multidimensional condition, and classify its biological substrate as mild.
However, it is essential that the symptoms of WCS be studied and assessed by specialists and professionals with experience in the field. Otherwise, some associated injuries may go unnoticed and a case may be described as minor cervical trauma when, in fact, it is not.
Conflicts of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Aso Escario J, Martínez Quiñones JV, Aso-Vizán A, Sebastián Sebastián C, Arregui Calvo R, Bosque Arbiol A. El esguince cervical como accidente laboral. Epidemiología y resultados de un protocolo de abordaje multiaxial. Rev Esp Med Legal. 2017;43:47–57.