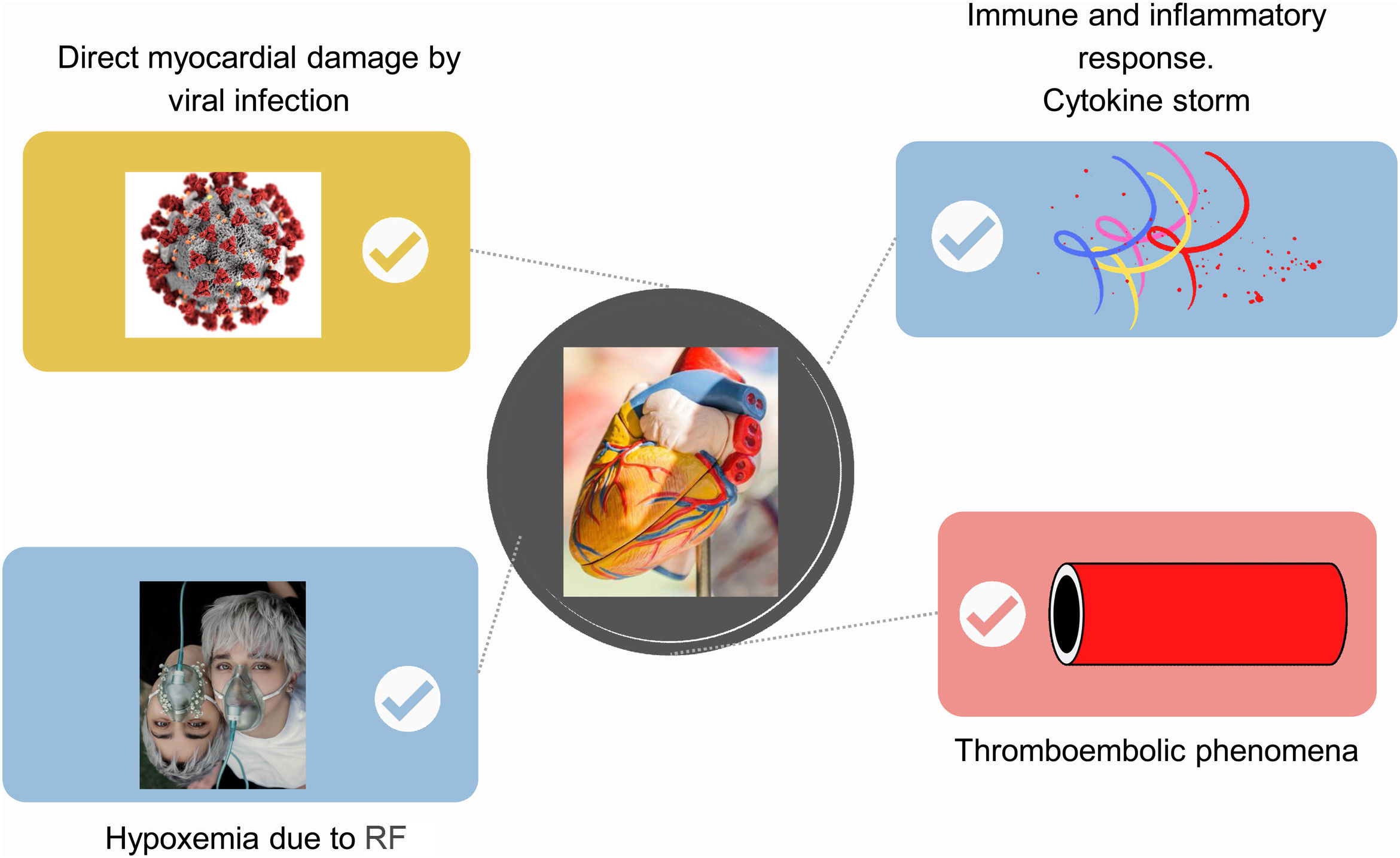
SARS-CoV-2 infection has a very important relationship with cardiovascular disease. Since the beginning of the pandemic, a close relationship has been observed between cardiovascular comorbidity and a worse prognosis in COVID-19 patients. The study of the pathophysiology of SARS-CoV-2 infection and cardiovascular disease suggests several concomitant hypotheses: direct myocardial damage by the virus, hypoxemia secondary to respiratory failure, inflammatory response to infection and/or thromboembolic phenomena. Cardiovascular damage can manifest in the acute phase of infection with acute myocardial infarction, myocarditis, arrhythmias…, during this phase Nuclear Cardiology procedures have not played a determining role in the diagnosis and management of these patients. On the other hand, in the subacute phase of the infection and in the post-acute COVID syndrome, Nuclear Cardiology seems to shed light on what happens in the cardiovascular system in this phase of the disease.
The COVID-19 pandemic has represented a great challenge for health systems, with a significant reduction in non-urgent diagnostic procedures with the aim of reducing the risk of transmission to patients and health personnel. Nuclear Cardiology has not been an exception. In addition to the prioritization of urgent/non-deferrable procedures and general screening, hygiene and distance measures, the main organizations and scientific societies of Nuclear Medicine and Nuclear Cardiology released recommendations and guidelines for safe practice, introducing significant changes in myocardial perfusion SPECT protocols.
La infección por SARS-CoV-2 tiene una relación muy importante con la patología cardiovascular. Desde el inicio de la pandemia se objetivó una relación estrecha entre la comorbilidad cardiovascular y un peor pronóstico de los pacientes COVID-19. El estudio de la fisiopatología de la infección por SARS-CoV-2 y la enfermedad cardiovascular sugieren varias hipótesis concomitantes: el daño miocárdico directo por el virus, la hipoxemia secundaria a la insuficiencia respiratoria, la respuesta inflamatoria a la infección y/o los fenómenos tromboembólicos. El daño cardiovascular se puede manifestar en la fase aguda de la infección con cuadros de infarto agudo de miocardio, miocarditis, arritmias…, durante esta fase los procedimientos de Cardiología Nuclear no han tenido un papel determinante en el diagnóstico y manejo de estos pacientes. En cambio, en la fase subaguda de la infección y en el síndrome del COVID post-agudo la Cardiología Nuclear parece ofrecer luz a lo que sucede en el sistema cardiovascular en esta fase de la enfermedad.
La pandemia de la COVID-19 ha representado un gran reto para los sistemas de salud constatándose una reducción importante de pruebas diagnósticas no urgentes con el objetivo de disminuir el riesgo de transmisión a pacientes y personal sanitario. La Cardiología Nuclear no ha sido una excepción. Además de la priorización de pruebas urgentes/preferentes y las medidas generales de screening, higiene y distancia, los principales organismos y sociedades científicas de Medicina Nuclear y Cardiología Nuclear han elaborado recomendaciones y guías para su práctica segura introduciendo notables cambios en los protocolos SPECT de perfusión miocárdica.
The relationship between SARS-CoV-2 infection and cardiovascular disease (CVD) is not anecdotal. Early studies published by Chinese expert groups described CVD as a common comorbidity in COVID-19 patients, with the association being stronger in those patients with more severe clinical disease: patients requiring hospital admission, admission to an intensive care unit or non-survivors1. The meta-analysis published by Jing Yang et al., which included eight Chinese studies with a total of 46,248 infected patients, showed that the most frequent comorbidities were hypertension (17%), diabetes mellitus (8%) and CVD (5%). Although the mechanism of association has not been clarified in the literature so far, the higher prevalence of CVD in older patients, immune system disorders or elevated angiotensin 2 levels have been described as potential causes; it was even suggested that CVD patients may be more predisposed to COVID-192.
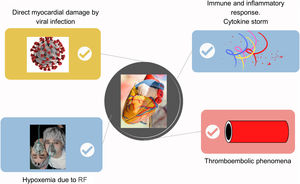
Based on the known clinical data and previous evidence on the immune system response to coronaviruses known to date, different theories have been developed for the pathophysiological mechanism causing the cardiovascular complications of COVID-19. It should be recalled that the SARS-CoV-2 S protein capable of mediating receptor binding and fusing with the cell membrane of epithelial cells is 80% genomically similar to the SARS (the virus of the acute respiratory syndrome) S protein, so they use the same receptor: angiotensin-converting enzyme 2 (ACE-2)3. Thus, the most relevant theories (Fig. 1) regarding cardiovascular damage are mainly four, bearing in mind that they are not mutually exclusive and there may even be synergies between them4. The first is direct myocardial damage due to viral infection. Acute myocarditis is a known complication of viral infections. Cases of fulminant myocarditis have been reported in COVID-19 patients. Although viral particles could not be demonstrated in myocardial biopsies from necropsies of COVID-19 patients, it is believed that it may act similarly to SARS in 2002 when viral RNA fragments were found in up to 35% of samples. SARS-CoV-2 infection may be direct infection of cardiomyocytes mediated by ACE-2, with cell lysis and activation of the innate immune response with release of pro-inflammatory cytokines.
Second, myocardial damage secondary to hypoxaemia due to respiratory failure. Tissue damage and secondary inflammatory processes with vasodilatation, endothelial permeability and leukocyte recruitment leading to increased lung damage would cause hypoxaemia and cardiovascular stress, which could lead to myocardial damage with elevated markers.
Third, the immune and inflammatory response secondary to infection, better known as cytokine storm. Cell invasion by SARS-CoV-2 causes an ineffective but amplified immune reaction, with release of inflammatory cytokines that can result in systemic inflammatory reaction, sepsis and multiorgan damage, in the case of the myocardium, believed to be the cause of myocarditis.
Finally, thromboembolic phenomena. The prothrombotic state has been highly described in COVID-19 patients. This state would be the cause of the instability and rupture of the atherosclerotic plaque, together with the suppression of ACE-2 expression due to an increase in Angiotensin-2, which generates oxidative stress, endothelial dysfunction and vasoconstriction related to plaque instability. In addition, there is a direct viral effect on endothelial cells and vascular pericytes.
Cardiovascular damage is translated into biochemical markers. Biomarkers of cardiomyocyte damage such as NT-proBNP or nitric oxide (NO) are important in both the diagnosis and prognosis of asymptomatic or early-stage CVD5. It has been found that these biomarkers are altered in patients with acute COVID-19 and even in post-acute COVID-19 syndrome, with elevated NT-proBNP and decreased NO levels reported, which seem to correlate with a worse prognosis of patients6. Likewise, elevated cardiac troponin as a marker of myocardial damage is a prognostic predictor in COVID-19 patients7. However, as demonstrated by Bardají's group, it behaves similarly to other clinical processes associated with possible cardiac involvement in the absence of type 1 myocardial infarction8.
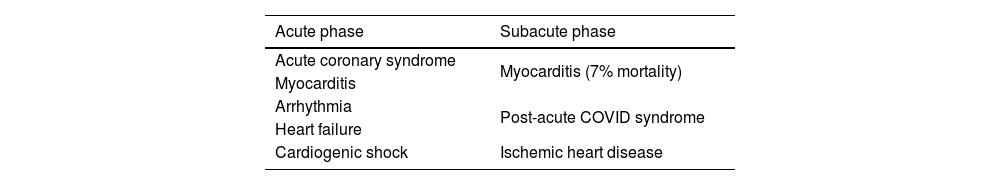
This translates clinically in different ways depending on the stage of the disease. In the acute phase, cardiovascular damage usually presents as acute coronary syndrome, myocarditis, arrhythmia or thromboembolism, even heart failure (HF) and cardiogenic shock9. While in the post-acute phase (3 weeks to 2 months after the acute phase), patients usually present with palpitations, chest pain, exertional fatigue or arrhythmias. In this phase, the most frequent complication is myocarditis with a 7% mortality rate10 (Table 1).
The literature review shows the potential benefits of nuclear cardiology (NC) in the diagnosis and management of some of these clinical pictures. Myocarditis is a disease characterised by inflammation of the myocardial tissue, its aetiology can be infectious or non-infectious. In the case of infectious causes, it may be due to infections by viruses, bacteria, fungi or protozoa, with viral causes being the most frequent. The most frequent viral pathogens are coxackievirus, parvovirus B19, influenzae virus and coronaviruses, including SARS-CoV-2. The gold standard for the diagnosis of myocarditis is endomyocardial biopsy (EMB), although it is seldom performed, its sensitivity is low and its false negative rate is high in the case of patchy involvement11. Therefore, the diagnostic management of these patients is usually based on a thorough clinical and physical examination, cardiac biomarkers, electrocardiogram and non-invasive imaging studies12. In fact, in the case of myocarditis caused by COVID-19, the European Society of Cardiology (ESC) guidelines do not recommend EMB and favour the use of cardiac imaging for diagnosis13. Due to its low cost, accessibility at the patient's bedside and portability, transthoracic echocardiography (TTE) is the first imaging modality indicated in suspected myocarditis in COVID-19 patients, as further recommended by the ESC myocardial and pericardial diseases working group14 and in fact has been extensively used in the acute phase of the pandemic, especially in patients on life support.
The association of COVID-19 infection with pulmonary respiratory disease and pulmonary thromboembolism has made iodinated contrast (IC) CT a widely used tool during the pandemic. Cardiac CT with delayed enhancement could be useful in tissue characterisation in patients with COVID-19 and suspected myocarditis15. There has been some experience with this but with very few patients studied16. Although it is widely known that delayed enhancement CT is still inferior to results obtained by magnetic resonance imaging (MRI)17. Thus, cardiac MRI is the Gold Standard non-invasive imaging technique for the diagnosis of myocarditis. It should be noted that cardiac MRI has its limitations due to the duration of the study and possible patient restrictions such as arrhythmias, inability to perform apnoea, claustrophobia, metal implants or contrast allergy, as well as its difficulty in intubated COVID patients. Therefore, experts recommend performing short, targeted studies and, once the patient is stable and not infectious, longer studies to rule out fibrotic phenomena18. In the case of NC, [18F]Fluorodeoxyglucose positron emission tomography (18F-FDG-PET) has been used in patients in whom other techniques were contraindicated, as in the case of patients with prosthetic valves. The role of PET/CT in the study of COVID-19 myocarditis is still unclear, and the COSMIC-19 study led by Alam et al. aims to answer these questions by being the first study to compare different imaging techniques, in particular 18F-FDG-PET/CT versus MRI in the assessment of myocarditis19. This study will also show the role of 18F-FDG-PET/CT in the evaluation of large vessels and the described cases of vasculitis where 18F-FDG-PET/CT could also provide information and even, as in the case of other pathologies, be a marker of response to treatment. All these unknowns highlight the value of the necessary research work that is still pending in this infectious pathology.
At the current time of the pandemic, probably most interesting are the findings related to the so-called post-acute Covid-19 syndrome, characterised by patients who after the acute phase of COVID-19 infection suffer from palpitations, chest pain, exertional fatigue and even arrhythmias10. Sariçamet et al. studied patients who had undergone acute COVID infection from 3 weeks to 2 months previously: a total of 105 patients, 40 asymptomatic and 65 symptomatic, all with normal cardiac structure and negative troponins. Symptomatic patients had elevated NT-proBNP and decreased NO levels. All patients underwent TTE, which was altered in only 2 patients in the symptomatic group. Only 15 cardiac MRI scans were performed with no alterations observed in any of them and of these patients only 5 underwent cardiac PET/CT, all of them showing patchy hyperfixations of 2[18F]Fluorodeoxyglucose. All this would suggest that 18F-FDG-PET/CT could provide further pathophysiological guidance for this condition or help in the diagnosis and management of these patients6. Although it must be said that caution should be exercised with these results and further studies are needed as the current evidence is very limited and its methodology is not entirely clear as it is not known if there is a correct preparation of the patient for the cardiac study.
Although acute coronary syndrome has been rare as the initial presentation of COVID-19, it has been reported to affect patients with healthy coronary arteries20. It is believed that endothelial dysfunction, progression of atheromatous plaque formation, emotional factors or hypoxia may be the cause of autonomic nervous system dysfunction characterised by an increased sympathetic system, increasing vascular tone and leading to atheromatous plaque instability, together with systemic inflammatory factors also affecting plaque stability, all according to current knowledge of the disease21.
In contrast, in the case of persistent COVID, chest pain is usually a recurrent symptom along with dyspnoea. Several imaging studies have demonstrated a relationship between these symptoms, especially chest pain and coronary vascular involvement. For example, the case described by Vallejo et al.22 in which a woman with no previous cardiological history came to the clinic for the presence of chest pain one month after recovering from COVID-19. The investigators detected the presence of microvascular ischaemia using adenosine cardiac MRI. Agarwal et al. describe the case of a young man with persistent dyspnoea on exertion being diagnosed with heart failure (HF) due to extensive post-COVID infarction without the presence of coronary artery disease23.
It is well known that myocardial perfusion scintigraphy is a fundamental imaging tool for the diagnosis of ischaemia and cardiovascular risk. Araz et al. have shown that myocardial perfusion studies are also a good tool for the assessment of patients with persistent COVID syndrome, especially those presenting with chest pain or dyspnoea21. In their retrospective study they assessed the COVID-19 group of patients against a control group demonstrating that there was a higher number of pathological studies in patients with a history of COVID-19 infection, even in those with no history of cardiovascular pathology. Furthermore, the need for an invasive coronary artery study or treatment was also higher in the COVID-19 group compared to the control group. The study by Ibrahim et al. also leaned in this direction. They studied myocardial flow reserve by PET in a prospective study of patients previously infected by COVID-19 and a control group with no known infection. Patients were matched for age, sex and cardiovascular risk factors. The authors observed a higher rate of reduced myocardial flow reserve as a marker of worse prognosis, as it correlated with a higher rate of cardiac events24. More studies are needed to better understand the pathophysiology of these conditions and to have more scientific evidence for the management of patients and to provide them adequate treatment and a better prognosis.
NC techniques in the study of myocardial perfusion and cardiovascular risk are widely validated and widespread, so they could offer a very interesting window for the study of these patients. In our humble opinion, a greater effort should be made with respect to cardiac PET in order to be able to offer this tool to our patients with current technology, both in terms of equipment and radiopharmaceuticals, based on scientific evidence and within the European environment in which we find ourselves.
Thus, based on current scientific knowledge, we can conclude that NC techniques are not the most indicated or the techniques of choice in the acute phase of COVID-19. Patients with associated heart disease tend to be complicated and life-threatening patients to whom it is difficult to apply Nuclear Medicine (NM) techniques, due to the fact that they tend to be long tests and difficult to use in this type of patient, who often cannot be transferred to the NM departments due to their high fragility. On the other hand, NC has a role in the detection of inflammatory and ischaemic pathology in post-COVID syndrome. It is vitally important to have a broad knowledge of the clinical pictures associated with CVD in COVID-19 patients, in order to have a correct clinical suspicion and to be able to apply the best technique with the best-expected results. To this end, interdisciplinary assessment and the application of the best technique with an integrated and holistic analysis of all findings is important. We need to continue research in CN techniques, especially hybrid single photon emission computed tomography (SPECT)/CT, PET/CT and PET/MRI techniques that can provide a lot of information to prevent and manage possible cardiovascular complications secondary to SARS-COV-2 infection such as HF with the socioeconomic implications that this disease can cause to our society.
Impact on Nuclear Cardiology practiceThe COVID-19 pandemic has been an unprecedented challenge for all health care systems worldwide, leading to a drastic reduction in the performance of non-urgent procedures with the aim of reducing the risk of transmission to patients and health care personnel. Non-urgent procedures, including cardiac diagnoses and therapeutic approaches have been postponed or directly cancelled25–27. CVD remains the principal cause of morbidity and mortality not only in high-income countries but also in medium-income and low-income countries and the prognosis is closely associated with early diagnosis and evidence-based therapies.
Thus, delays in diagnosis and therapy have produced a significant increase in mortality by ischemic heart disease and hypertensive processes globally25. In 2020, the Health Division of the International Atomic Energy Agency (IAEA) of the United Nations launched a very detailed online questionnaire aimed at all member countries to know the magnitude of the reduction of diagnostic cardiac procedures (non-invasive and invasive). The group carrying out the questionnaires is known as INCAPS-COVID, the first letters correspoding to IAEA Noninvasive Cardiology Protocols Study. Data were collected from 909 centers in 108 countries, including the participation of 27 Spanish centers. From March 2019 to April 2020 a 64% reduction in all diagnostic procedures and a 73% decrease in NM stress tests was reported, with the greatest reduction being observed in SPECT compared to PET modality26. With data collected from the questionnaires analyses focused on Italy, Europe, the United States, Oceania, Asia and South America were also performed27–32. In the Europe study countries were divided into 4 blocks: West, South (including Spain), North and East, with a greater reduction in procedures observed in the South block as well as in countries with a lower gross domestic product27.
Recommendations for performing Nuclear Cardiology studiesSpain was badly hit by the COVID-19 pandemic, with 98 cases per 100,000 inhabitants and 10% mortality at the peak of the first wave during lockdown.
The care of patients with COVID-19 in Spain and worldwide required the creation of health care infrastructures and adaptation of those already existing. In order to continue providing safe services it was necessary to implement changes and take precautions in health care at all levels, including NM and NC procedures.
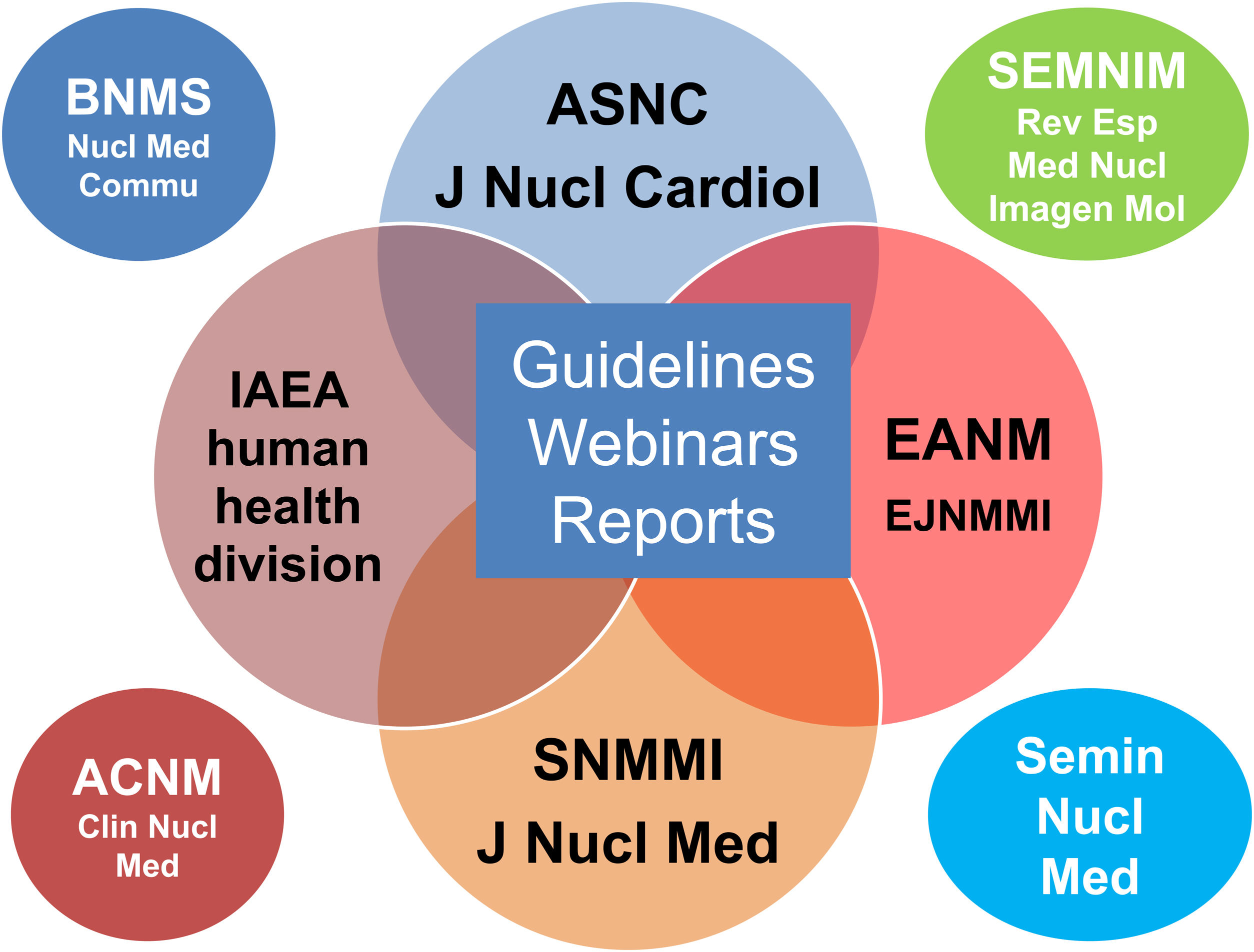
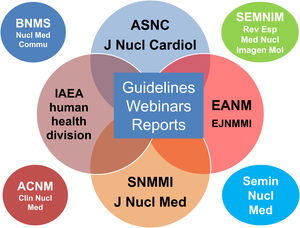
The scientific societies of NM and NC offered guidance and recommendations for the safe practice of our procedures during the worst moments of the pandemic in the form of webinars, guidelines and online publications (Fig. 2). Basic measures included the prioritization of emergency tests, symptom screening and COVID tests prior to the procedure, meticulous hygiene of spaces/surfaces and hand washing, physical distancing and the use of individual protection equipment (IPE)25 together with modifications in the study protocols as described in the next section. NM and NC societies also guided the reintroduction of non-urgent procedures as the pandemic receded until we reached the present chronic endemic state.
In March 2020, a few weeks after the declaration of the pandemic, the British Society of Nuclear Medicine (BSNM) published basic guidelines online for the prevention and control of infection in NM departments33. In addition to the previously mentioned general measures, the guideline included a classification by clinical priority of NM procedures into 3 categories:
- 1
Cannot be cancelled/postponed.
- 2
Discuss with requesting clinician prior to performing or cancelling/postponing a procedure.
- 3
Can be directly cancelled/postponed.
Myocardial perfusion studies for acute chest pain and radionuclide ventriculography (MUGA) in oncologic patients were among the procedures that could not be deferred or cancelled. Routine myocardial perfusion studies were in group 2 and cardiac amyloidosis (99mTc-DPD), innervation and viability with 201 Tl were in group 3. Shortly thereafter, a guideline and an editorial were published in Nuclear Medicine Communications34,35 containing greater details regarding changes to be made in the facilities, patient and personnel protection and slight modifications in the classification by clinical priority of the NM procedures with no changes in those related to NC. Soon after, the American Society of Nuclear Cardiology (ASNC) published a similar classification by priority, also with 3 categories, mainly related to patients without COVID-1936:
- 1
Perform without delay.
- 2
Postpone 2–4 months.
- 3
Postpone >4 months.
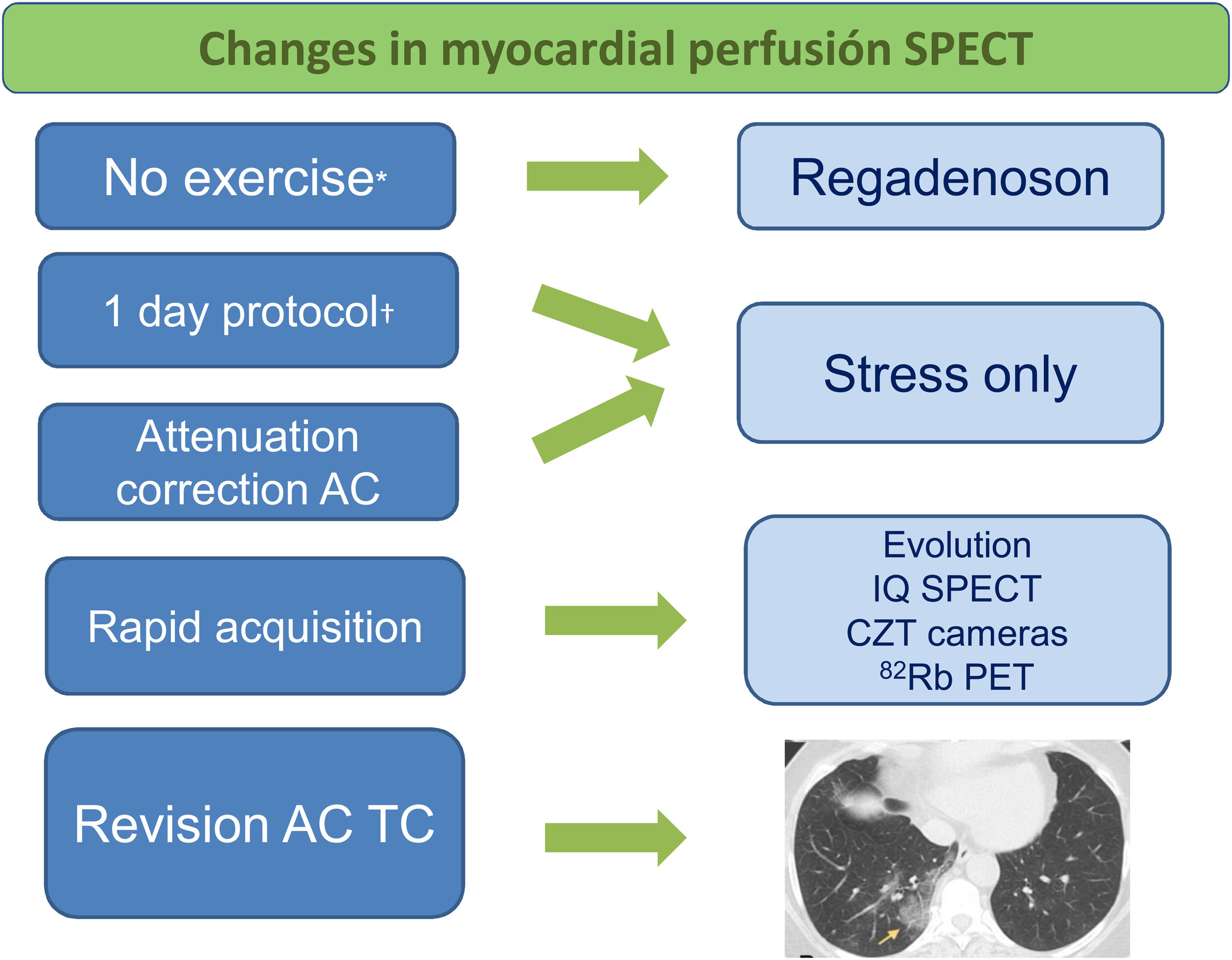
In addition to acute chest pain in its different clinical forms, priority 1 included preoperatory myocardial perfusion studies for evaluating ischemia in patients with moderate-high risk in cases of urgent surgery and when there was an option of revascularization and in selected cases of liver transplant surgery. Stable angina with no plan to perform urgent revascularization was given priority 2 or 3, according to each particular case. Studies of cardiac amyloidosis with 99mTc-PYP could be given priority 1 in selected cases and PET studies with 18F-FDG for sarcoidosis or endocarditis/device infection were priority 1 for the initial evaluation but not in the follow-up. MUGA studies related to cardiotoxic chemotherapy were classified as priority 1 both at baseline and during follow-up. In all cases, procedures were to be performed according to the criteria of appropriate use and based on clinical judgment, the urgency of decision making and the expected benefits in the short-term management of the patient36. In March 2020 ASNC also presented a webinar with faculty from China and Singapore, the first areas of the world to suffer the effects of the pandemic. The webinar was focused on the practice of NC and especially myocardial perfusion studies37. Already at this time pharmacologic stress with vasodilator agents were being recommended to avoid exposure to droplets produced by intense respiration during physical exercise, although it should be noted that exericse ECG testing (with or without NM) could be safely performed with protection equipment. In addition, preference was given to short acquisition protocols and systematic review of the attenuation correction CT component of SPECT/CT and PET/CT was proposed in search of possible COVID-19 findings. Review of the chest CT with lung window before patient discharge could show ground glass opacities and multilobar, rounded, posterior and peripheral condensations characteristic of the infection as well as air bronchograms and thickening of lobar septa25,38.
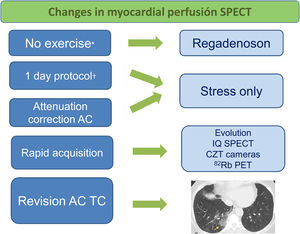
Since myocardial perfusion PET studies are scarcely performed in Spain, the short protocols basically refer to gamma cameras of cadmium/zinc/telluride (CZT) and to multifocal IQ-SPECT and special software in the case of conventional gamma cameras. In a multisociety webinar organized by IAEA in April 2020, these recommendations were confirmed39. Previously in March 2020, IAEA had launched a webinar40 on the safe practice of NM as a whole with the participation of an international panel of experts, which was later published in European Journal of Nuclear Medicine and Molecular Imaging41. In May 2020, a statement published by ASNC and Society of Nuclear Medicine and Molecular Imaging (SNMMI)36 added the preferential use of regadenoson due to its rapid and efficient protocol as well as the use of the PET modality (when available) versus SPECT, also due to its shorter duration. It should be noted that if regadenoson is not available, adenosine and dipyridamole may be used with longer infusion systems that allow maintaining a greater distance from the patient. A 1-day stress/rest protocol was also recommended to avoid both displacement of patients on different days and the rest phase when the stress phase was normal (stress only protocol). It must be emphasized that the use of attenuation correction CT reduces the proportion of equivocal studies, and thus helps to avoid unnecessary rest studies. The NC Working Group (GTCN acronym in Spanish) of the Spanish Society of Nuclear Medicine and Molecular Imaging (SEMNIM acronym in Spanish) released its recommendations in a statement made in July 202042. These included those mentioned above and also insisted on the value of MUGA studies for echocardiography cardiologists in oncologic patients as well as 18F-FDG PET/CT in patients with suspicion of endocarditis/cardiac device infection as the first option to avoid the closeness to patients when performing transesophageal echocardiography.
As the pandemic receded, a joint statement by ASNC, IAEA and SNMMI was published in 2020 for safely reestablishing non-urgent NC procedures43. This statement maintained the previous recommendations but also began to raise the possibility of performing the 2-day protocol in outpatients to reduce their time in the facilities. Later, in 2022, a new joint report was published on the transition from the pandemic state to a chronic endemic state44. Following the recommendations of avoiding stress with exercise in favour of pharmacologic stress in the peak phases and initial recession phases of the pandemic, in this chronic phase the important role of stress with exercise was re-asserted due to the substantial additional diagnostic and prognostic information provided (functional capacity, electrocardiogram, hemodynamics). Thus, it is recommended to consider performing stress with exercise in patients in whom it is indicated, taking into account the local incidence of COVID-19 and vaccination rates (patients and personnel) as well as the availability of IPE, spaces with ventilation systems and pretest COVID-19 screening. Fig. 3 shows the basic recommendations for performing myocardial perfusion studies.
Recommendations for safely performing myocardial perfusion SPECT for patients and health care personnel during the COVID-19 pandemic.
CZT: cadmium, zinc, telluride. *Following the peak phases and initial recession of the pandemic it was considered important to return to physical exercise if indicated. †In later phases of the pandemic the 2-day protocol was also recommended for the shorter time of patients in the facilities.