Current methods for the production of Histoplasma capsulatum antigens are problematic in terms of standardization, specificity, stability, repeatability and reproducibility.
AimsIn this study, we sought to optimize the methodology for producing H. capsulatum antigens, and to evaluate its applicability.
MethodsAntigenic preparations obtained from 12 H. capsulatum isolates were evaluated by double immunodiffusion and immunoblotting assays against homologous and heterologous sera.
ResultsThe evaluated and optimized protocol allowed a more stable production, as well as repeatable, reproducible, with shorter culture time and less costly. By double immunodiffusion and immunoblotting assays, the best pattern of reactivity was observed for antigens obtained with 33 days of culture from the isolates 200 and 406 against the M antigen and for the isolate 200 with 15 days against H antigen. The SDS-PAGE presented antigenic components of molecular masses between 17 and 119kDa. The immunoblotting sensitivity was 95.5% and 100% with histoplasmosis sera from ill patients and sera from H. capsulatum infected but otherwise healthy patients, respectively, to the antigen derived from isolates 200 and 406.
ConclusionsWe suggest the employment of the antigen from isolate 200, with 15 or 30 days of culture, in the double immunodiffusion and immunoblotting assays due to its good ability to discriminate both sera from patients with histoplasmosis illness and histoplasmosis infection, in addition to its high specificity against heterologous sera.
Los métodos actuales para la producción de antígenos de Histoplasma capsulatum son problemáticos en términos de estandarización, especificidad, estabilidad, repetitividad y reproducibilidad.
ObjetivosEn este estudio se buscó optimizar la metodología para la producción de antígenos y evaluar su aplicabilidad.
MétodosLas preparaciones antigénicas obtenidas de 12 cepas de H. capsulatum se evaluaron por doble inmunodifusión en gel de agar e inmunotransferencia frente a sueros homólogos y heterólogos.
ResultadosEl protocolo evaluado y optimizado permitió mayor sensibilidad en la producción, más estabilidad, repetitividad y reproducibilidad con menos tiempo de cultivo y menor coste. Los mejores patrones de reactividad por inmunodifusión en gel de agar e inmunotransferencia se observaron en el antígeno M obtenido tras 33 días de cultivo de las cepas 200 y 406, y en el antígeno H de la cepa 200 tras 15 días de cultivo. Con la técnica SDS-PAGE se separaron componentes antigénicos de masas moleculares entre 17 y 119kDa. La sensibilidad de la inmunotransferencia fue del 95,5% y del 100% con sueros obtenidos de pacientes con enfermedad y con sueros de pacientes infectados, pero sanos, respectivamente, con antígenos derivados de las cepas 200 y 406.
ConclusionesSugerimos el empleo del antígeno de la muestra 200, con 15 o 30 días de cultivo, en los ensayos de doble inmunodifusión en gel e inmunotransferencia debido a su buena capacidad para discriminar los sueros de pacientes enfermos de histoplasmosis y los de pacientes portadores sanos, además de su elevada especificidad frente a sueros heterólogos.
Histoplasma capsulatum, a dimorphic fungus, is the etiologic agent of classical histoplasmosis, a mycosis that principally affects the lungs and other organs of the reticulo-endothelial system.5 Histoplasmosis is the most common endemic mycosis in North America and in certain areas of Mexico and Central and South America.32 In Brazil, endemic areas are located in the Midwestern and Southeastern regions, where the prevalence ranges from 4.4 to 63.1% and 3.0 to 93.2%, respectively.10 The infection with H. capsulatum occurs by inhaling microconidia after disturbance of environmental sites containing the organism.5,10,20,32 Clinical manifestations of this illness depend on the degree, time and frequency of exposure, and size of inocula as well as age and immune status of the host.14,32 The majority of the exposed populations have a mild self-limiting or subclinical form of infection; however, infants and immunocompromised individuals may contract acute symptomatic or progressive life-threatening disseminated forms of the disease.32 The definitive diagnosis of histoplasmosis includes the isolation of H. capsulatum on specific culture media or the visualization of the yeast cells in direct examination of clinical specimens employing specific fungal staining techniques.2,10,11 However, these procedures are time-consuming as H. capsulatum may take as long as 4–6 weeks to grow at room temperature in the mold form, and requires a level 3 biosafety facilities.4,10,32 It is known that the isolation of H. capsulatum in culture is a critical component of the diagnostic process; however, the employment of serological assays has played an important role in the diagnosis of chronic cavitary pulmonary and acute pulmonary histoplasmosis in which a fourfold rise in antibody titer to H. capsulatum can be a diagnostic finding.11,24,26,29,32 The standard assays are the complement fixation and double immunodiffusion, but ELISA and immunoblotting may also be used.1,5,6,9,11,20,30 Two main antigenic molecules are important for antibody detection: the H antigen, against which antibodies are elicited during active histoplasmosis (disease), and the M antigen, that elicits antibodies in active and chronic histoplasmosis.10,11,17,32 The immunodiffusion assay is approximately 80% sensitive but is more specific than the complement fixation; however, it is considered an important serologic test for the detection of both H and M antigens in histoplasmosis.11,24,32 According to Wheat et al., H precipitins, present in less than 25% of patients, usually clear within the first 6 months after the infection, while M precipitins are present in 75% individuals and may persist for several years.32 Immunochemical analyses of H and M antigens indicated that both are glycoproteins, and carbohydrates constitute between 10 and 30% of the H antigen. The observed molecular masses of H and M antigens are 108–120kDa and 70–94kDa, respectively.7,34 Current methods for the production of H. capsulatum antigens are problematic in terms of standardization, specificity, stability, repeatability and reproducibility. Thus, in this study, we sought to optimize the methodology for the antigens production described by Standard and Kaufman,30 evaluating its applicability in histoplasmosis immunodiagnosis, especially by double immunodiffusion and immunoblotting assays.
Material and methodsH. capsulatum isolatesTwelve H. capsulatum isolates (49, 200, 212, 268, 299, 340, 361, 406, 584, 802, 2030 and RP) were selected for this study. Fifty percent of them were isolates from patients with an HIV infection (49, 212, 299, 340, 584 and 2030). Two samples, 802 and RP, were isolated from renal transplanted and diabetes mellitus patients, respectively. The isolates were maintained in the Culture Collection of the Mycology Laboratory of Instituto de Medicina Tropical de São Paulo, Brazil, on solid potato medium at room temperature (25–27°C) and subcultured every three months, in the mycelial form.
Preparation of H. capsulatum antigensTo prepare the antigens of each H. capsulatum isolate, we employed the Standard and Kaufman's method with some modifications.30 Briefly, mycelial cells of all isolates were grown in solid Sabouraud-dextrose (Difco Laboratories, Detroit, MI, USA) medium at 27°C during 15 and 33 days. After the incubation time, the cultures were treated with aqueous solution of thimerosal 1:5000 (Sigma Chemical Co. St. Louis, MO, USA) and left to stay for 24h at room temperature. Afterwards, the supernatants were filtered through Whatman® no. 1 paper (Whatman, Brentford, UK). The solution with the antigens were concentrated 10- to 20-fold by a lyophilization procedure. After protein dosage by the Bradford method,3 antigenic preparations were stored at −20°C until use.
Serum samplesSerum samples were obtained from the Mycological Serum Bank of the Immunodiagnosis Mycosis Laboratory of Instituto Adolfo Lutz, São Paulo, Brazil. Sera were obtained from patients with proven cases of histoplasmosis illness (22 cases), histoplasmosis infection without illness (3 cases), paracoccidioidomycosis (16 cases), aspergillosis (10 cases), cutaneous leishmaniasis (7 cases), and muco-cutaneous leishmaniasis (6 cases). In addition, 15 samples from healthy blood donors, 11 samples of patients with clinical suspicion of histoplasmosis and non-reactive against H. capsulatum reference antigen (Immuno-Mycologics, Inc, Norman, OK, USA), and 11 samples of spelunkers (non reactive against the H. capsulatum reference antigen previously selected) were used as negative controls. Anti-Paracoccidioides brasiliensis, anti-H. capsulatum and anti-Aspergillus fumigatus sera were produced in New Zealand with female rabbits immunized subcutaneously with 100μg of each exoantigen; sera were obtained after six weeks and the antigens were processed through Mckinney and Parkinson method.18 All samples were divided into aliquots and stored at −20°C until the moment of use. Informed consent was obtained from all subjects participating in this study, which was approved by Internal Scientific Commissions and Bioethics in Human Research Committee of Instituto Adolfo Lutz (CCD BM n° 06/2004), Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (CAPPesq n° 983/03) and Instituto de Medicina Tropical da Faculdade de Medicina da Universidade de São Paulo (n° 010/03).
Double immunodiffusion, sodium dodecyl sulfate polyacrylamide gel electrophoresis and immunoblotting assaysThe double immunodifusion assay was performed according to Freitas et al.,9 and the sodium dodecyl sulfate polyacrylamide gel electrophoresis and immunoblotting were performed as previously described by Laemmli and Towbin et al., modified by Freitas et al.9,15,31 To analyze the variables among the H. capsulatum antigens obtained from different H. capsulatum isolates, the Byes methodology (Minitab V13.1 Software-Minitab Inc., State College, PA) was applied.
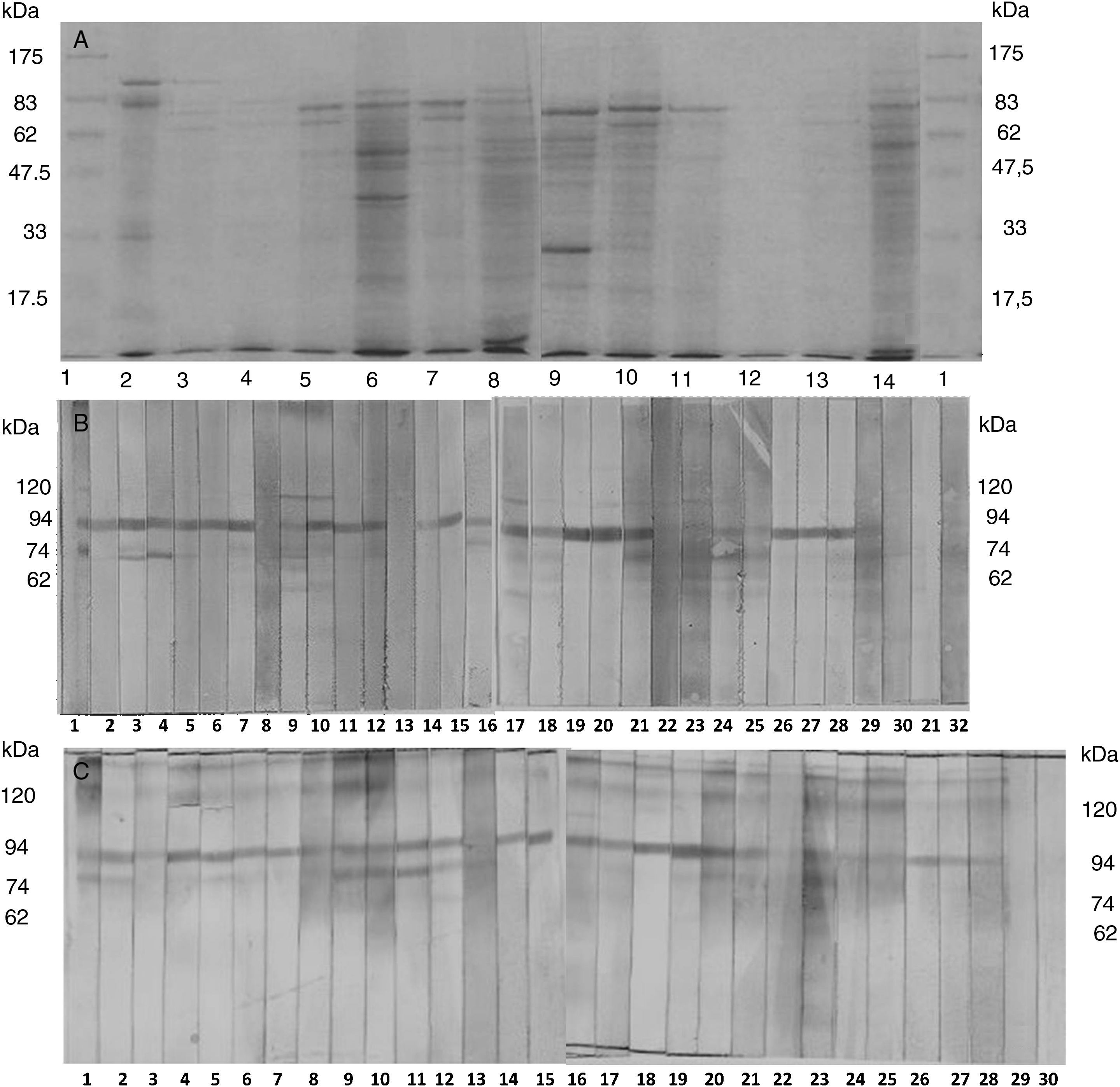
ResultsScreening of H. capsulatum antigensBy double immunodiffusion assay we observed that 83.3% (n=10) of the 10- or 20-fold concentrated H. capsulatum solutions, obtained after 15- and 33-day cultures in solid Sabouraud-dextrose medium, specifically recognized the positive control serum anti-H and M fractions (Immuno-Mycologics). We also observed that all antigenic preparations reacted against rabbit polyclonal anti-H. capsulatum exoantigen. No cross-reaction was observed against heterologous rabbit polyclonal antibodies (P. brasiliensis and A. fumigatus). The comparative analysis of electrophoretic profiles of the H. capsulatum antigens showed a great variation from isolate to isolate. Evaluating the electrophoretical mobility on SDS-PAGE we detected 20 different protein fractions after Coomassie Brilliant Blue staining (Fig. 1A). Isolate 268 showed the largest number of protein fractions with 17 antigenic fractions distributed in a range of a molecular weight from 10 to 94kDa. Moreover, it was possible to verify the presence of the H and/or M antigens in the antigenic fractions derived from isolates 49, 200, 268, 299, 340, 361, 406, 584 and RP. Analyzing these results, as well as those obtained by phenotypic observation, we selected four H. capsulatum isolates (49, 200, 268 and 406).
(A) Electrophoretic profile of the antigens of H. capsulatum, obtained according to Kaufman and Standard (1978), in agar-Sabouraud-dextrose, 27°C, 33 days of culture. Lane 1: molecular weight standard; Lane 2: antigen of reference; Lane 3: Ag Hc 49; Lane 4: Ag Hc 200; Lane 5: Ag Hc 212; Lane 6: Ag Hc 268; Lane 7: Ag Hc 299; Lane 8: Ag Hc 340; Lane 9: Ag Hc 361; Lane 10: Ag Hc 406; Lane 11: Ag Hc 584; Lane 12: Ag Hc 802; Lane 13: Ag Hc 2030 and Lane 14: Ag Hc RP. (B) Immunoreactivity pattern of circulating IgG anti-H.capsulatum antibodies from patients suffering histoplasmosis (1–22), H.capsulatum-infected but healthy patients (22–28), and sera from healthy subjects (29–32) against antigens derived from isolate 200, 10-fold concentrate, according to Kaufman and Standard, cultured in Sabouraud-dextrose agar, 27°C, for 33 days. (C) Immunoreactivity pattern of circulating IgG anti-H.capsulatum antibodies from patients suffering histoplasmosis (1–20), H. capsulatum-infected but healthy patients (21–27), and sera from healthy subjects (28–30) against antigens derived from isolate 200, 10-fold concentrate, according to Kaufman and Standard, cultured in Sabouraud-dextrose agar, 27°C, for 15 days.
Serum samples that had at least one line of precipitation against H. capsulatum antigenic preparation were considered reactive. The positivity rate of the 15-day culture antigens evaluated against sera from patients suffering histoplasmosis was 40.9% (n=9), 95.5% (n=21), 95.5% (n=21) and 4.5% (n=1) to antigens derived from isolates 49, 200, 406 and 268. Moreover, the discriminatory profile of these antigens against serum samples from infected, but otherwise healthy, patients was 85.7% (n=6), 71.4% (n=5), and 71.4% (n=5) to antigens derived from isolates 49, 200 and 406. On the other hand the percentage of reactivity of the antigenic preparations obtained after 33 days of culture against sera of ill patients was 77.3% (n=17), 95.5% (n=21), 95.5% (n=21) and 18.2% (n=4) to antigens derived from isolates 49, 200, 406 and 268; the percentages of reactivity with sera from patients only infected were 85.7% (n=6), 71.4% (n=5) and 71.4% (n=5) for antigens obtained from isolates 49, 200 and 406. We observed no difference in positivity degree when antigens obtained from cultures of 15 and 33 days were evaluated in pool; the discriminatory ability against sera from ill patients and infected but non-ill patients was 27.2% (n=6) and 85.7% (n=6), respectively, for both antigenic preparations. The specificity of antigens’ recognition was evaluated with sera from patients with paracoccidioidomycosis, aspergilosis, cutaneous leishmaniasis, muco-cutaneous leishmaniasis, as well with samples from healthy blood donors, samples of patients with clinical suspicion of histoplasmosis but not reactive against H. capsulatum reference antigen, and samples of spelunkers not reactive against H. capsulatum reference antigen, showing 100% specificity in all cases.
Immunoblotting assay analysisWe verified by immunoblotting that the isolates 49, 200, 268 and 406 produced, in addition of H (120kDa) and M (94kDa) fractions, a particular range of proteins that certainly deserve more attention in the future. When analyzing the different batches of the antigens produced after 15 and 33 days of culture of the tested isolates, we observed that 100% of the evaluated sera (sera from ill patients and sera from infected but healthy patients) recognized at least one antigenic fraction. We also observed stronger anti-M-antigen (94kDa) reaction against antigens derived from isolate 200 cultured for 33 days (Fig. 1B) and from isolates 268 and 406 cultured for 15 days. Moreover, we observed stronger anti-H-antigen (120kDa) binding against antigens obtained from isolates 200 (Fig. 1C), 268 and 406 cultured for 15 days. When we analyzed serum samples of 11 spelunkers that were not reactive by double immunodiffusion assay against the H. capsulatum reference antigen and the antigens produced in this study, it was demonstrated by immunoblotting assay that 94.1% (n=17) reacted with the 94kDa and/or 74kDa antigens. No cross reactivity was observed among the serum samples from blood bank donors.
Stability of H. capsulatum antigensThe stability of the antigens (15 and 33 days) lyophilized and stored at −20°C was analyzed by double immunodiffusion and immunoblotting assays after 6, 12, 24 and 36 months against positive control sera (anti-H and M fractions), and histoplasmosis sera (illness and infection). The results showed that both antigens retained their activity.
DiscussionInvasive fungal infections represent one of the main causes of morbidity and mortality especially in immunocompromised patients.21,26 Despite the activity of the host immune system, H. capsulatum can successfully cause a lung infection and, if left untreated, can spread to extrapulmonary sites.26,32 According to Prado et al.25 the mortality rate due to histoplasmosis as the primary cause of death in association with AIDS in Brazil from 1996 to 2006 was 4.73 per 1000. Thus, early and accurate diagnosis is essential for the establishment of effective and specific therapy to reduce the unnecessary use of toxic and/or empiric drugs, thereby minimizing the emergence of multidrug-resistant fungal strains.8 The studies about fungal antigens have gained considerable importance, especially with regard to their applicability as immunobiological reagents in assessing humoral and/or cellular immunity. In this study we have shown that a soluble antigen recovered from H. capsulatum mycelium is a stable and specific reagent that can be easily prepared, even for anyone with relatively few resources, and used for the serodiagnosis of histoplasmosis in double immunodiffusion and immunoblotting assays. However, many factors (fungal strain, inoculum size, culture medium, temperature and incubation time, incubation form, i.e., with or without agitation) are involved in the quality of the antigenic preparation; for H. capsulatum there is specifically a need to ensure the presence of H and M fractions.12,13,22,28,34 According to Pine et al.22 an optimal antigen is one which is highly sensitive and specific in reacting with the antibodies produced against the pathogen of interest, in this case H. capsulatum. The authors evaluated the effect of different media and chemical treatments on the relative antigenicity and specificity of different yeast-form H. capsulatum isolates. They concluded that the relative sensitivity and specificity of an antigen should be verified with several low, medium, and high titrated homologous and heterologous antisera, and the choice of the H. capsulatum strain is the most critical step in obtaining a higher order of specificity. Even though all the antigenic preparations evaluated by SDS-PAGE presented the H and/or M fractions, we observed differences in sensitivity by double immunodiffusion assay. The reactivity pattern against sera from patients suffering histoplasmosis was 77.3% to the antigen derived from isolate 49, 95.5% to the antigens from isolates 200 and 406, and 18.2% to the antigen obtained from isolate 268. The reactivity of these antigenic preparations against sera from infected but otherwise healthy individuals was 85.7% to the antigen produced from isolate 49, and 71.4% to the antigens from isolates 200 and 406. The results of the double immunodiffusion testing in Land et al.16 showed a higher sensitivity with mycelial antigens when compared with yeast-phase antigens or a combination of both. Passos et al.20 evaluated an outbreak in São Paulo related to a visit to a cave. In the first set of samples by double immunodiffusion quantitative test using mycelia antigens, only a single serum reacted with the antigens. However, when testing by means of immunoblotting, 61.8% of the sera were reactive. In a second set of samples, collected two months after the exposure, 96.7% of the sera were reactive by double immunodiffusion; when testing the sera by immunoblotting all of them reacted against H and M fractions, demonstrating that during the first month of illness serologic tests for antibodies searching can be negative. Wheat et al.33 provided a discussion of the role of antigen detection in the diagnosis of histoplasmosis by sandwich enzyme immunoassay using polyclonal antibodies to H. capsulatum, and they observed that negative results, occurring in up to 20% of disseminated cases and 25–30% of diffuse acute pulmonary cases, do not rule out the diagnosis of histoplasmosis. We observed that the presence of beige pigments in isolates 200 and 406 had, somehow, a relation with the antigenic expression, resulting in better results: both isolates expressed the 97 and 116kDa protein fractions, H and M fractions of H. capsulatum. On the other hand, we observed that samples with cotton texture and white pigmentation express preferentially fraction M of H. capsulatum. Concerning the method of extraction, our results are in agreement with the published literature in the use of thimerosal-borate solution12,13,19,27,28 in this antigenic preparations, demonstrating high indices of sensitivity and specificity, with an stability longer than 36 months. We have already mentioned that double immunodiffusion assay has been widely and routinely used in the immunodiagnosis of histoplasmosis; however this methodology has limitations, especially regarding the detection of antibodies anti-H. capsulatum in patients with acute and disseminated forms of the disease. In this study, we evaluated the sensitivity of immunoblotting assay employing antigens derived from isolates 200 and 406 of H. capsulatum. We found that sensitivity of immunoblotting was 95.5% with sera of patients suffering histoplasmosis and 100% with sera from H. capsulatum-infected but otherwise healthy people, and their specificity was in concordance with the literature. Western blot test with deglycosylated H and M antigens of histoplasmin provides a rapid, sensitive, and specific test to diagnose acute pulmonary histoplasmosis before precipitins can be detected; the glycosidic epitopes increased the specificity from 78 to 100% when periodate-treated H and M antigens were used.23 We used immunoblotting test in sera with clinical suspicious of histoplasmosis. In conclusion, the sensitivity, specificity, and stability of the serological tests depend on the methodology used in the antigenic preparation. The use in double immunodiffusion assay of the antigens produced by the isolates 200 and 406 showed high values of sensitivity and specificity for the detection of anti-M and anti-H antibodies. The immunoblotting was considered an important instrument in the confirmatory diagnostic of the histoplasmosis.
Author's contributionsRSdeF conducted laboratory evaluations. RSdeF drafted the first version of the article. APV and CMK made critical revision of the text. All authors read and approved the final manuscript.
Conflicts of interestThe authors declare that there is no conflict of interests.
We are grateful to Miss Lucia Cupertino Barreto, Mr. Vasco Gouveia, Mrs. Monica Candida G. Scola, Mrs. Lia Teixeira, Mr. Almir Robson Ferreira and Mrs. Maria Iranides Santana Oliveira for their technical assistance. We would like to thank Francisco Contreras Morales for the careful review of the Spanish. This study was supported by Instituto Adolfo Lutz-Coordenadoria de Controle de Doenças-Secretaria da Saúde do Estado de São Paulo (CTC-IAL # 107/97, # 13/2002 and # 05/04) and Instituto de Medicina Tropical da Universidade de São Paulo.