Pythiosis is caused by the agent Pythium insidiosum, an aquatic oomycete of the kingdom Stramenopila.
AimsTo describe the symptoms, pathological changes and diagnosis methods of gastric pythiosis in dogs.
MethodsA three-year-old female German shepherd, with access to wetlands, was attended due to vomiting and recurrent diarrhea of 30 days of duration. A palpable mass in the abdomen filling the left epigastric region was identified in the clinical examination. Simple and contrasted radiological examination and ultrasound of abdominal cavity were performed. The animal was referred for exploratory laparotomy for the removal of the mass. The extent of the mass prevented from the excision and the animal was euthanized. Samples of the tumor mass were collected and sent for morphological study and immunohistochemistry.
ResultsThe changes observed in imaging studies were consistent with gastric pythiosis. In cytology and histopathology, non-septate hyphae were identified, and in immunohistochemistry a strong positivity of anti-Pythium antibodies was observed, confirming the diagnosis of pythiosis.
ConclusionsPythiosis in dogs is diagnosed late and tends to evolve in the animal's death. The definitive diagnosis is by cytology, histology and immunohistochemistry.
El patógeno responsable de la pitiosis es Pythium insidiosum, un oomiceto acuático, perteneciente a la familia Pythiaceae, orden Peronosporales, clase Oomycetes, y perteneciente al reino Stramenopila.
ObjetivosDescribir la sintomatología, los cambios anatomopatológicos y métodos de diagnóstico de la pitiosis gástrica en perros.
MétodosUna perra hembra de raza Pastor Alemán, de 3 años de edad, y con acceso a tierras pantanosas, fue llevada a consulta por un cuadro de vómitos con diarrea recurrente de 30 días de evolución. Durante la exploración clínica, se identificó una masa palpable en el abdomen que ocupaba la región epigástrica izquierda, por lo que se procedió a la realización de un examen radiológico, simple y con contraste, junto con una ecografía abdominal. Más tarde, fue derivada para una laparotomía exploratoria con la finalidad de proceder a la exéresis de la masa. Debido a su tamaño, la exéresis no fue posible, por lo que se sacrificó al animal. Se obtuvieron muestras del tumor y se enviaron al laboratorio para su análisis morfológico e inmunohistoquímico.
ResultadosLos cambios observados en los estudios de diagnóstico por imagen eran compatibles con un diagnóstico de pitiosis gástrica. En el examen citológico e histopatológico se identificaron hifas no tabicadas, mientras que el examen inmunohistoquímico fue intensamente positivo para la presencia de anticuerpos anti-Pythium, confirmando el diagnóstico de pitiosis.
ConclusionesEl diagnóstico de pitiosis en perros se establece tardíamente, por lo que suele evolucionar hacia la muerte del animal. El diagnóstico definitivo debe establecerse a través de exámenes citológicos, histológicos e inmunohistoquímicos.
A three-year-old female German shepherd that lived in flooded areas, with complaints of poor appetite and recurrent vomiting in the last 30 days was seen. During the clinical evaluation, the dog was lethargic, with progressive weight loss, presenting an arching of the spine in the lumbar region. The animal presented fever (40.3°C), heart rate within the physiological range, tachypnea and dyspnea. During the palpation of the abdominal cavity, sensitivity was observed, which was accentuated when examining the cranial area on the left side where a mass of firm consistency was located. Blood samples were collected for hematology and determination of serum alanine aminotransferase (ALT), alkaline phosphatase (ALP), urea and creatinine.
To evaluate the abdominal mass noted in the clinical examination, simple and contrasted radiological examination and ultrasound of the abdominal cavity was performed. Treatment for reducing symptoms using fluid therapy, analgesic, antacid and antiemetic was recommended in order to maintain the quality of life and well being of the animal. The animal was referred for exploratory laparotomy for excision of the mass, and biopsy was performed with fine needle aspiration cytology (FNAC). The slides obtained by the FNAC were stained with rapid panoptic and viewed under a light microscope (100–400×). The extent of tumor mass prevented the excision, and the animal was euthanized.
Samples from the tumor mass were collected, fixed in 10% formalin and later on embedded in paraffin, cut into 5μm slides and stained with hematoxylin and eosin (HE) and Grocott methenamine silver (GMS). For the confirmation of pythiosis immunochemistry using polyclonal antibody (anti-Pythium) was performed, searching for marking structures morphologically compatible with Pythium insidiosum. The immunohistochemistry technique was performed according to the routine protocol that included blocking of endogenous peroxidase, antigen retrieval by microwave oven, blocking by non-fat dry milk and incubation of the sections with anti-P. insidiosum polyclonal antibody produced in rabbits. After that, they were incubated with biotinylated secondary antibody. This was followed by the incubation with estreptavidim-peroxidase complex. The washes were performed with PBST. The developing was performed with DAB. The sections were counterstained with Harris hematoxylin. Histological sections of equine cutaneous pythiosis cases were used as positive control. As negative control the primary antibody was replaced by antibody diluent in the sections tested.
In this clinical case, there were possibly pre-existing gastric lesions and with the ingestion of contaminated water with P. insidiosum zoospores the penetration in the sub-mucosal layer occurred, with the colonization and progressive development of the mass.6,7,10,13,15
The dog was a large-sized young adult female, living in temperate climate wetland area, with symptoms of vomiting, diarrhea and abdominal pain, as described in other studies on dog pythiosis.2,17–19 In the blood cell count exam arregenerative anemia (hematocrit 30.3%) and eosinophilia (1274μL) were observed. These hematological changes were described in dogs with pythiosis.2,21 The values of ALT, ALP and creatinine were within the physiological range with the exception of urea that was slightly increased possibly due to episodes of vomiting associated with anorexia.20
In X-ray examination solid radiopaque region and reduction in the gastric lumen were observed. In the ultrasound examination marked thickening of the gastric wall was viewed, with irregularity of the mucosal surface, neo-formation projected inside the organ, echogenic, with thin areas and liquid content with hypoechogenic fluid with suspension points. The changes observed in imaging studies were consistent with gastric pythiosis.5
During the necropsy it was possible to observe that the stomach was enlarged, thickened from the mucous layer to the serosa to the full extent of the greater curvature. Histopathology of the gastric wall revealed multifocal areas of caseous necrosis surrounded by inflammatory infiltrate of macrophages, epithelioid cells and giant cells and few neutrophils and eosinophils, especially in the mucosa. Within these necrotic areas by hematoxylin and eosin, tubuliform negative images compatible with fungal hyphae were observed, which in special Grocott staining, were found to be compatible with P. insidiosum. The macroscopic and microscopic changes were similar to those described in the literature.16,17
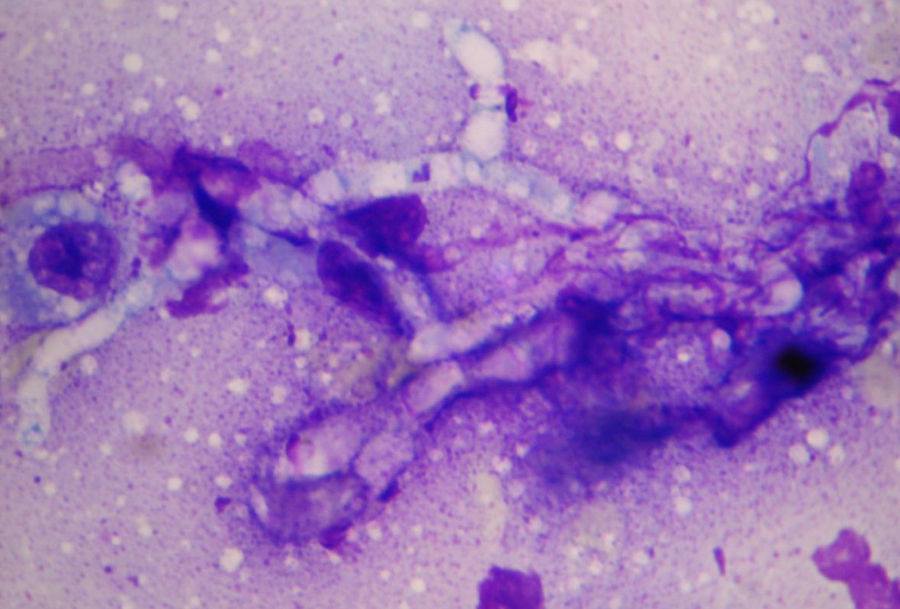
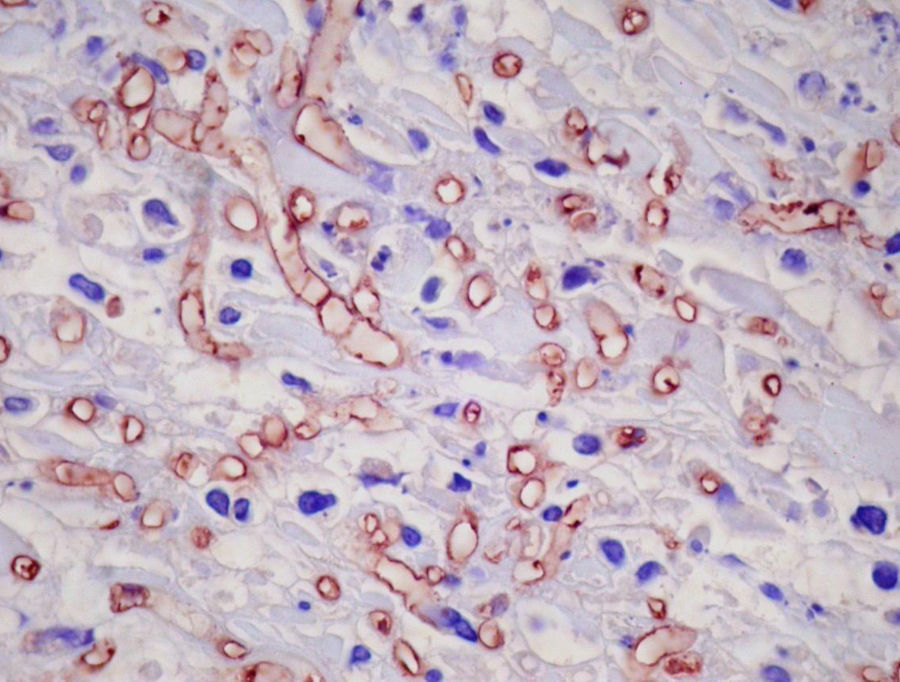
During cytology, a high concentration of inflammatory cells such as neutrophils and eosinophils was observed, along with the presence of thick-walled hyphae, sparsely septate, irregularly branched at right angles, suggesting the diagnosis of pythiosis (Fig. 1). In the immunohistochemistry a strongly positive marking of the antibodies anti-Pythium was observed, making it possible for the confirmation of the diagnosis of pythiosis (Fig. 2). The differentiation between the pathogens of pythiosis, zygomycosis and langenidose is important;7,19 therefore, more specific tests such as immunohistochemistry, ELISA (enzyme linked immunosorbent assay), CRP (Protein C reactive), among others2,6,12,14 should be used.
Pythiosis affecting the skin and the gastrointestinal tract is the most frequent manifestation in dogs. In this report there was only pythiosis development of the stomach, and the involvement of small and large intestine as described in other cases5,21 was not observed. Case reports of pythiosis in dogs indicate that due to the extent of the masses, the dogs did not present survival greater than three to four months, even with excision of the mass.2,3 Drug treatment of pythiosis in dogs as in other species has not been effective.17,21 The agent does not present in its cell wall ergosterol, the target substance of most antifungal drugs.21 Although in vitro studies using antifungal agents against isolates of P. insidiosum have shown satisfactory results indicating synergism.1,8 A recent study in a dog with gastrointestinal pythiosis treated with a combination of itraconazole, terbinafine and mefenoxam showed satisfactory results during the 18 months of administration.8 Other studies in horses and in experimental animals, adjuvant in the immune response showed satisfactory effects.4,9,11
Pythiosis should be included in the differential diagnosis in young dogs that live in an environment with access to water from lakes, rivers or irrigated crops and that have weight loss, chronic diarrhea and vomiting with a palpable mass in the abdomen. Pythiosis in dogs is diagnosed late and tends to evolve in the animal's death, and the definitive diagnosis is by cytology, histology and immunohistochemistry. Therefore, in order to have a greater survival of patients with pythiosis, there is a need for a diagnosis in early stages of the clinical development and, in the future, the use of immunotherapy may be a possibility to prolong survival in dogs with pythiosis.
Conflict of interestThe authors declare that there are no financial or personal relationship which can cause a conflict of interest regarding this article.
Hospital de Clinicas Veterinária – HCV of Federal University of Pelotas (UFPel) and profaDra Daniela Isabel Brayer Pereira for giving the antibodies used in immunohistochemistry technique acquired through the Mycological Research Laboratory LAPEMI/UFSM.