Poor adherence to treatment is a problem of great importance and striking magnitude. Its consequences are increased health care costs and poor health outcomes. It defined the objective of this research, which is the study of psychological characteristics of patients with different degrees of adherence to rehabilitation treatment after coronary bypass surgery. Ninety male and female patients with CHD, aged 46–71, were examined. The study was carried out using the questionnaire of ways of coping and the technique for diagnosing the types of attitude toward the disease, and the study of medical history. The analysis of the types of attitude toward the disease revealed that adherent patients show higher values on the harmonious type; patients with poor adherence show higher values on the apathetic, as well as the melancholic type of attitude toward illness. This study shows that wide range of psychological characteristics is significant for the definition of adherence to treatment. It is essential to consider the patient's personality and his characteristics, such as attitude toward the disease, because they influence the adherence and, therefore, the effectiveness of therapy in the postoperative period.
La escasa adherencia a la terapia es un problema de gran importancia ampliamente extendido. Sus consecuencias son el aumento de costes del tratamiento y su baja eficacia. El objetivo de la investigación fue el estudio de las características psicológicas de pacientes con diferentes grados de adherencia al tratamiento de rehabilitación después de la cirugía de derivación coronaria. Se recogieron datos clínicos de 90 pacientes de ambos sexos con cardiopatía coronaria, sometidos a cirugía de derivación coronaria, con edades comprendidas entre 46-71 años. Los cuestionarios administrados fueron el cuestionario de estilos de afrontamiento y la técnica de diagnóstico de tipos de actitud hacia la enfermedad. Además se realizó un estudio del historial médico. Se reveló que los pacientes adherentes mostraban puntuaciones más altas en el tipo “armonioso” de actitud hacia la enfermedad, y los pacientes con escasa adherencia, en los tipos “apático” y “melancólico”. El estudio confirma que las características psicológicas son significativas para la definición de la adherencia. Es imprescindible tener en cuenta tanto la personalidad del paciente y sus características como su actitud hacia la enfermedad, ya que ésta influye en la adherencia y, por lo tanto, la eficacia de la terapia en el periodo postoperatorio.
Nowadays the problem of adherence to long-term treatment in patients with chronic diseases is actual and significant (World Health Organization, 2014). This issue is relevant to a wide variety of diseases such as diabetes, depression, cancer, asthma, etc. According to the statistics of the World Health Organization, about half of patients with chronic diseases do not comply with medical prescriptions (World Health Organization, 2003).
The present-day medicine is at a high level of development. The process of treatment now is characterized by numerous restrictions for patients, by many limitations of their habits. Currently, the widespread use of drugs leads to the transition of the responsibility for the results of treatment from the health care professional to the patient.
Among the various branches of medicine, the problem of adherence to treatment in cardiology is particularly important, for the cause of existence of a vital threat among patients due to their disease. According to the World Health Organization statistics, cardiovascular diseases are the leading cause (48%) of death from non-communicable diseases among people aged 30–70 years (World Health Organization, 2013). In cardiovascular mortality the first position is occupied by the coronary heart disease, the rates of which in the Russian Federation reached 53.1% of all causes of death from cardiovascular diseases (Federal’naya sluzhba gosudarstvennoy statistiki, 2013; Surinov, 2011).
Today, in cardiology the surgical methods of treatment based on myocardial revascularization are recognized as the most promising in terms of improving the quality of life and prognosis of patients with severe coronary heart disease (Bockeria, Gudkova, & Stupakov, 2010), which is currently treated very effectively by surgical methods. In the last ten years the number of bypass operations, especially coronary artery bypass grafting, or CABG surgery has increased 5.2 times, and they allow to achieve very good health indicators in patients (Botnar, 2009). However, the recovery process after the surgery often does not lead to the expected results. Patients do not return to work, health indicators do not improve and relapses of the disease that cause rehospitalizations occur. Despite the efficacy of surgical treatment and objective health improvement, markers of the physical health and quality of life in some patients worsen because of their lack of adherence to the rehabilitation process. Therefore, adherence to treatment is an important determining factor of overall health outcomes also after surgery.
Therefore, it is necessary to pay attention to the postoperative recovery period and also to the patients’ willingness to accept treatment, their level of awareness of the disease severity and, consequently, the degree of adherence to therapy.
The literature on the subject finds the lack of adherence to treatment among patients with coronary heart disease after coronary bypass surgery. There are several reasons for it, the patients’ firm belief that they are completely healthy after surgery is one of them. In fact, the surgery allows to restore fully the blood flow in the myocardium, therefore the result of the surgery is a radical cure of coronary heart disease (Shal’nova & Deev, 2011). However, patients should take the prescribed medication lifelong in order to avoid relapses of the disease. Their wellbeing after surgery, the complete restoration of body functions and the underestimation of the importance of maintenance therapy cause a very poor adherence among patients undergoing this type of surgery.
The term adherence to therapy (treatment) first of all requires determination. The World Health Organization presents its definition in the report “Adherence to longterm therapies, evidence for action” (World Health Organization, 2003). Adherence to long-term therapy is considered as the extent to which a person’ behavior –taking medication, following a diet, and/or performing the life-style changes, corresponds with agreed recommendations from a health care professional. It should be emphasized that, however the drug treatment (adherence to it is usually evaluated excluding other factors) is important, it is essential to consider adherence also to the prescribed diet, the rejection of harmful habits (such as smoking or alcohol consumption), increase of physical activity, and so on. In the case of lack of attention to any of them, the treatment effect may be impaired, often the patient is rehospitalized and the cost of treatment increases.
We should also pay attention to the differences between the concepts adherence and compliance, which have also been defined in the report of the World Health Organization (World Health Organization, 2003). The main difference is that adherence to therapy requires the patient's consent to the recommendations. Patients should be active partners with medical care professionals on the issue of their own health care, and good communication between the patient and the health professional is essential for effective clinical practice.
The question about the factors that influence on adherence to treatment remains unanswered. There is a great number of studies that aim to understand what leads to an adherent or non-adherent behavior, but still there is no clear evidence of the influence (or prevalence) of any of the factors (World Health Organization, 2003). Current studies try to determine the effect of medical, socio-demographic, economic, organizational, and other factors.
At the same time, it is evident that individual patients’ characteristics play a particular role in forming an adherent behavior. Previous experience with health care professionals, medical history, the coincidence of real facts with patients’ expectations, their ways of thinking and attitudes, such as the attitude toward the disease, patients’ character attributes, their skills in self-management, etc. may influence adherence to therapy.
Despite the apparent evidence of this fact there are not so many researches of the psychological factors of adherence. The available data are contradictory, so there is no clear answer to the question about the influence of the psychological characteristics of patients on their adherence to therapy.
The mentioned problem of adherence to therapy in patients with coronary heart disease defined the objective of this research: the study and comparative analysis of the psychological characteristics of patients suffering from coronary heart disease, with different degrees of adherence to rehabilitation treatment after coronary bypass surgery.
A complex research program, which includes the study of emotional, cognitive, motivational characteristics of patients with coronary heart disease as well as their personality characteristics and coping strategies, was developed. The obtained data is numerous, and requires a detailed analysis and profound interpretation. In this article the results of the analysis of two aspects (patients’ coping strategies and their attitude toward the disease) are presented. The research was conducted in the Federal Almazov North-West Medical Research Center (St. Petersburg, Russia).
MethodSampleThe sample consisted of 90 patients of both genders with coronary heart disease, undergoing coronary bypass surgery. The average age of participants was 60.99 years (SD=7.33), with ages between 46 and 71 years, and gender distribution of 74 men (82%) and 16 women (18%). Most of the patients suffer from coronary heart disease for quite a while: approximately 65% admit the presence of cardiac symptoms for six years or more. Not all of them were treated for cardiovascular diseases; many of the patients in all that time did not even consult the doctor. They were divided into two groups: adherent to treatment (patients who regularly implement the recommended drug therapy and non-drug treatment, 47 persons, 52.2%) and non-adherent patients (those who do not regularly follow the medical recommendations of the drug therapy, control and correction of risk factors, and non-drug treatment, 43 persons, 47.8%). The division into groups was carried out by a procedure performed by experts (an interdisciplinary team of clinical psychologists, cardiologists).
ToolsThe research was conducted by the detailed study of patients’ medical records, a semi-structured interview which consists in a range of questions, grouped into sections (clinical and physiological characteristics, socioeconomic, psychological, etc.), and two psychometric techniques.
The first is the Lazarus and Folkman Ways of Coping Questionnaire, adapted and standardized by Vasserman et al. (2009). Its test-retests reliability is 0.84.
The second, the Technique for Diagnosing the Types of Attitude toward the Disease (originally “TOБOЛ”) (Vasserman, Iovlev, Karpova, & Vuks, 2005). This psychometric test is a procedure which aims to diagnose various types of personal reaction to the disease (i.e., attitude toward the disease) in patients with somatic diseases, mainly chronic. The test constructed in the form of a questionnaire allows to diagnose 12 types of attitude toward the disease (see Table 1), based on information about the patient's reaction to a series of problems and life situations, potentially important to him, and directly or indirectly related to his disease. These “subsystems” of individuals’ relationships with their environment formed the basis for structuring the content of the test in 12 dimensions: attitude toward the disease, toward the treatment, toward healthcare personnel, family, work (or studying), the atmosphere, the loneliness, the future, as well as the mood, the physical wellbeing, sleep and appetite. Each of these dimensions includes, in turn, several statements, compiled on the base of the clinical experience of the expert group. The patient must choose two statements suitable to him in all the dimensions. The diagnosis of the type of attitude toward the disease is based on the fact that the highest score in any of the scales indicates a higher probability of patient's affiliation with the type associated with this scale. Therefore, the type of attitude toward the disease can be determined by the highest score of the scales.
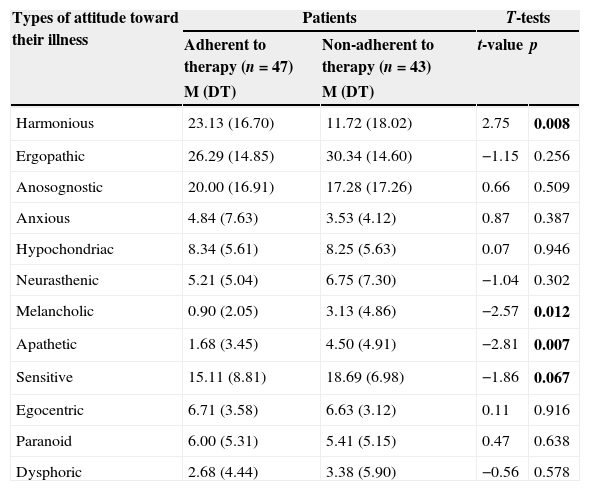
Mean scores in groups of patients.
| Types of attitude toward their illness | Patients | T-tests | ||
|---|---|---|---|---|
| Adherent to therapy (n=47) | Non-adherent to therapy (n=43) | t-value | p | |
| M (DT) | M (DT) | |||
| Harmonious | 23.13 (16.70) | 11.72 (18.02) | 2.75 | 0.008 |
| Ergopathic | 26.29 (14.85) | 30.34 (14.60) | −1.15 | 0.256 |
| Anosognostic | 20.00 (16.91) | 17.28 (17.26) | 0.66 | 0.509 |
| Anxious | 4.84 (7.63) | 3.53 (4.12) | 0.87 | 0.387 |
| Hypochondriac | 8.34 (5.61) | 8.25 (5.63) | 0.07 | 0.946 |
| Neurasthenic | 5.21 (5.04) | 6.75 (7.30) | −1.04 | 0.302 |
| Melancholic | 0.90 (2.05) | 3.13 (4.86) | −2.57 | 0.012 |
| Apathetic | 1.68 (3.45) | 4.50 (4.91) | −2.81 | 0.007 |
| Sensitive | 15.11 (8.81) | 18.69 (6.98) | −1.86 | 0.067 |
| Egocentric | 6.71 (3.58) | 6.63 (3.12) | 0.11 | 0.916 |
| Paranoid | 6.00 (5.31) | 5.41 (5.15) | 0.47 | 0.638 |
| Dysphoric | 2.68 (4.44) | 3.38 (5.90) | −0.56 | 0.578 |
The study was performed during the hospital stay (after surgery) of patients, and then on outpatient basis. Patients were observed by cardiologists both before surgery and several months after it. Adherence to therapy was evaluated three months after surgery, when patients had returned to their usual lifestyle, their work, and when their physical recovery was complete. Subsequently, data on adherence was verified during the patients’ planned visits to the clinic (at six months and one year).
ResultsThe study of patients undergoing coronary bypass surgery showed that a wide range of their psychological characteristics is potentially significant for the definition of adherence.
It was found that one of the most important aspects of the psychological factor of adherence to treatment is the patients’ attitude toward their illness. The analysis of the patients’ average scores in each of the 12 types of attitude toward the disease revealed that the group of adherent patients shows higher values in the scale related to the “harmonious” type in contrast to patients of the non-adherent to therapy group (t=2.75; p<0.01). The type called “harmonious” is usually associated with the fact that patients evaluate their condition without exaggerating its seriousness, as well as without underestimating the severity of the disease, and also with their desire to contribute actively to the success of treatment.
Patients with poor adherence to therapy show higher values on the scale of the “apathetic” (or “anergic”) type of attitude toward the disease (t=−2.81; p<0.01) and the “melancholic” type (t=−2.57; p<0.05) compared to adherent patients. Two mentioned types are associated with the patients’ indifference about their fate, the consequences of the disease and treatment outcomes, and also with the loss of interest in life (the “apathetic” type), and with the lack of confidence in the recovery and possible improvement due to the effect of treatment, and a pessimistic outlook on everything (in type called “melancholic”) (Table 1).
In both groups of patients the predominance of types of attitude toward the disease in which mental and social adaptation is not significantly altered, was found.
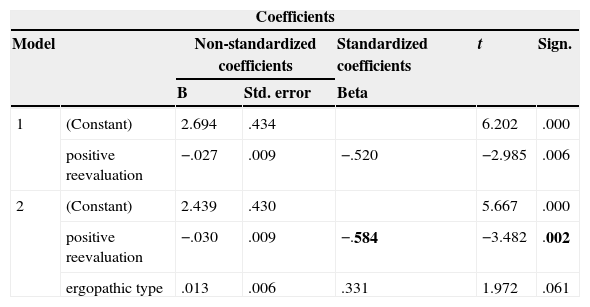
As part of our research the prognostic value of psychological characteristics in reference to the degree of patients’ adherence to therapy was also examined. The data of 50 patients were processed using a multiple regression analysis and discriminant analysis: 25 of the first group (adherent to therapy), and 25 of the second (non-adherent to therapy). In the regression analysis several models were considered, but the selected and used model was the one which includes two variables: coping strategy “positive reevaluation” and the “ergopathic” type of attitude toward the disease (model 2, see Table 2). The combination of these two factors explains about 38% of dispersion of the variable “group” (adherent and non-adherent to therapy patients).
Coefficients of multiple regression analysis.
| Coefficients | ||||||
|---|---|---|---|---|---|---|
| Model | Non-standardized coefficients | Standardized coefficients | t | Sign. | ||
| B | Std. error | Beta | ||||
| 1 | (Constant) | 2.694 | .434 | 6.202 | .000 | |
| positive reevaluation | −.027 | .009 | −.520 | −2.985 | .006 | |
| 2 | (Constant) | 2.439 | .430 | 5.667 | .000 | |
| positive reevaluation | −.030 | .009 | −.584 | −3.482 | .002 | |
| ergopathic type | .013 | .006 | .331 | 1.972 | .061 | |
Based on this analysis, it can be said that the major contribution to the prediction of the patient's group is made by the variable “positive reevaluation” in combination with the variable “ergopathic” type (Table 2). The beta coefficient (standard regression coefficient) is −0.58 (p<0.01), i.e., there is an inverse correlation between the variable “positive reevaluation” and the group. By itself, the variable “ergopathic” type does not contribute significantly to the regression model.
The data obtained from the regression analysis is confirmed by the discriminant analysis; a model that contains the same two variables was analyzed. The discriminatory power of the canonical function is reliable on a high level of statistical significance (Wilks’ Lambda=0.62, χ2=10.85; p<0.01). The contribution of the variables in the canonical function (i.e., the probability of assigning the patient undergone the test to one group or another): “positive reevaluation” 1.03; “ergopathic” type -0.66. That is, we can say that the canonical function includes two variables with unequal contribution. The higher the value of the variable “positive reevaluation” is and the lower the value of the variable “ergopathic” type is, the greater the probability of classifying patients in the adherent to therapy group is.
Thus, the rare use of the coping strategy “positive reevaluation” in combination with high rates of the “ergopathic” type of attitude toward the disease is significantly associated with non-adherent behavior.
The “ergopathic” type is characterized as a responsible attitude toward work, sometimes even obsessive, and is associated with the desire to maintain professional status and the opportunity to continue active work at the same level by all means.
Coping strategy “positive reevaluation” describes the strategy when patients try to overcome negative experiences related with the problem by rethinking the past in a positive way. They focus on a philosophical understanding of the situation related with the problem, and try to include it in the context of their own experience for the better development of their personality.
Discussion and conclusionsIn the studies over the last decades it is paid attention to the factors that influence adherence to therapy. There are several researches devoted to the study of economic and social factors (DiMatteo, 2004), demographic (such as patients’ age or sex), factors associated with patient – health care professional relationship (Marchena-Giráldez, Calero-Elvira, & Galván-Domínguez, 2013; Escolar-Gutiérrez, López-Moya, Portabales Barreiro, Carcedo-Robles, & Alonso-Abolafia, 2014).
At the same time attempts to systematize the data are made. Thus, there are various classifications of the factors that influence on adherence to therapy. For example, they are divided into the following groups: social and economic factors; factors related to the therapy; factors related to the patient; factors related to the health care system (Mathes, Jaschinski, & Pieper, 2014). In other sources the classifications are somewhat different, but still quite similar to the mentioned above. They are generally based on a detailed review of the literature and the analysis of numerous studies carried out in the area of adherence to therapy (Jin, Sklar, Min Sen Oh, & Chuen Li, 2008; Alsolami, Hou, & Correa-Velez, 2012).
The concept “patient-related factors” in the abovementioned studies is usually referred to such aspects as age, sex, ethnicity, and so on. Studies focusing on the analysis of the effect of patients’ beliefs about their health status and therapy in the degree of their adherence were also conducted (Vermeire, Hearnshaw, Van Royen, & Denekens, 2001; Phillips, Leventhal, & Leventhal, 2013; Horne et al., 2013).
However, the psychological characteristics of the patients are usually not included in the classifications of the factors that influence adherence to treatment, and are often excluded completely from the study. Researches of the psychological factors and its influence on the degree of adherence are found less frequent and contain contradictory data (World Health Organization, 2003).
The results of this research do not contradict the data from previous studies. The study performed by Zelenskaya, Demchenko, and Lubinskaya (2011) also revealed that the adherent and non-adherent to treatment patients are characterized by different types of attitude toward the disease. According to their data, the differences between the groups of patients respect to the mentioned characteristic are similar to those found in the present study. One of the most common types of attitude toward the disease among adherent to treatment patients is the “harmonious” (16% of the group) (Zelenskaya et al., 2011). The “sensitive” and “apathetic” types of attitude toward the disease are more common in the group of patients with poor adherence to treatment, and are diagnosed in 33% and 12% of patients in this group respectively (Zelenskaya et al., 2011).
In summary, our study shows that some psychological characteristics influence the patients’ adherence to treatment. The attitude toward the disease is one of them, and according to the diagnosed type it can be associated with adherent or non-adherent behavior of patients. Due to the vital risks faced by patients with cardiovascular diseases, and the cost of treatment, especially the surgery, it is essential to continue the study of the psychological factor, because we consider its potential significance for the definition of adherence to treatment and consequently, for developing ways to increase the effectiveness of therapy.
The patient's personality and psychological characteristics, such as the attitude toward the disease, must be taken into account during the treatment, since it affects the adherence and therefore, the postoperative period in all.
The data obtained will help in advance to qualify the patients with high risk of non-adherent behavior and identify the targets of correction programs and psychological support for patients in the pre- and postoperative period, and to develop educational programs for patients with coronary heart disease.
FundingThis research was supported by the Russian Foundation for Humanities and Social Sciences (РГНФ No 14-06-00-163a).
Conflict of interestThe author declares no conflict of interest.