Fournier's gangrene is a polymicrobial infection of perineal and scrotal regions that manifests as a rapidly progressive necrotizing fasciitis. Fournier's gangrene following a surgical procedure is not frequently seen. We report a very rare case of Fournier's gangrene following inguinal hernia repair.
La gangrena de Fournier es una infección polimicrobiana de la región perineoescrotal, que se manifiesta como una fascitis necrosante, rápidamente progresiva. La gangrena de Fournier, después de un procedimiento quirúrgico no se ve con frecuencia. Se presenta un caso muy raro de la gangrena de Fournier después de la reparación de la hernia inguinal.
Fournier's gangrene is a polymicrobial infection of perineal and scrotal regions that manifests as a rapidly progressing necrotizing fasciitis.1,2 Firstly, in 1883, it was described by Jean Alfred Fournier. In 1883 and 1884, Fournier presented five cases of a rapidly progressing gangrenous infection in five otherwise healthy young men. In the following decades different terms were used to describe this clinical entity although Wilson introduced the term ‘necrotizing fasciitis’ in 1952, which is still used today. The most common complications of hernia repair are hematomas, including penile or scrotal ecchymosis; seromas; and wound infection.3 Fournier's gangrene following inguinal hernia repair is uncommon. The morbidity and mortality in this severe complication depend on early diagnosis and aggressive surgical management.
Case reportA 52 year-old male with a history of right inguinal hernia repair (high ligation and prolene mesh) 40 days ago, referral to our department from another hospital. This patient was referred us because of widespread necrosis and gangrene extending from the perianal region and scrotum to the right inguinal region. His medical history was unremarkable except presence mild heart failure. Clinically, the patient had a temperature of 37°C and his peripheral pulses were palpable. His blood analysis was leukocytosis as 13000 (range: 4000–10000) and elevated CRP levels as 4.5 (range: 0–0.5).
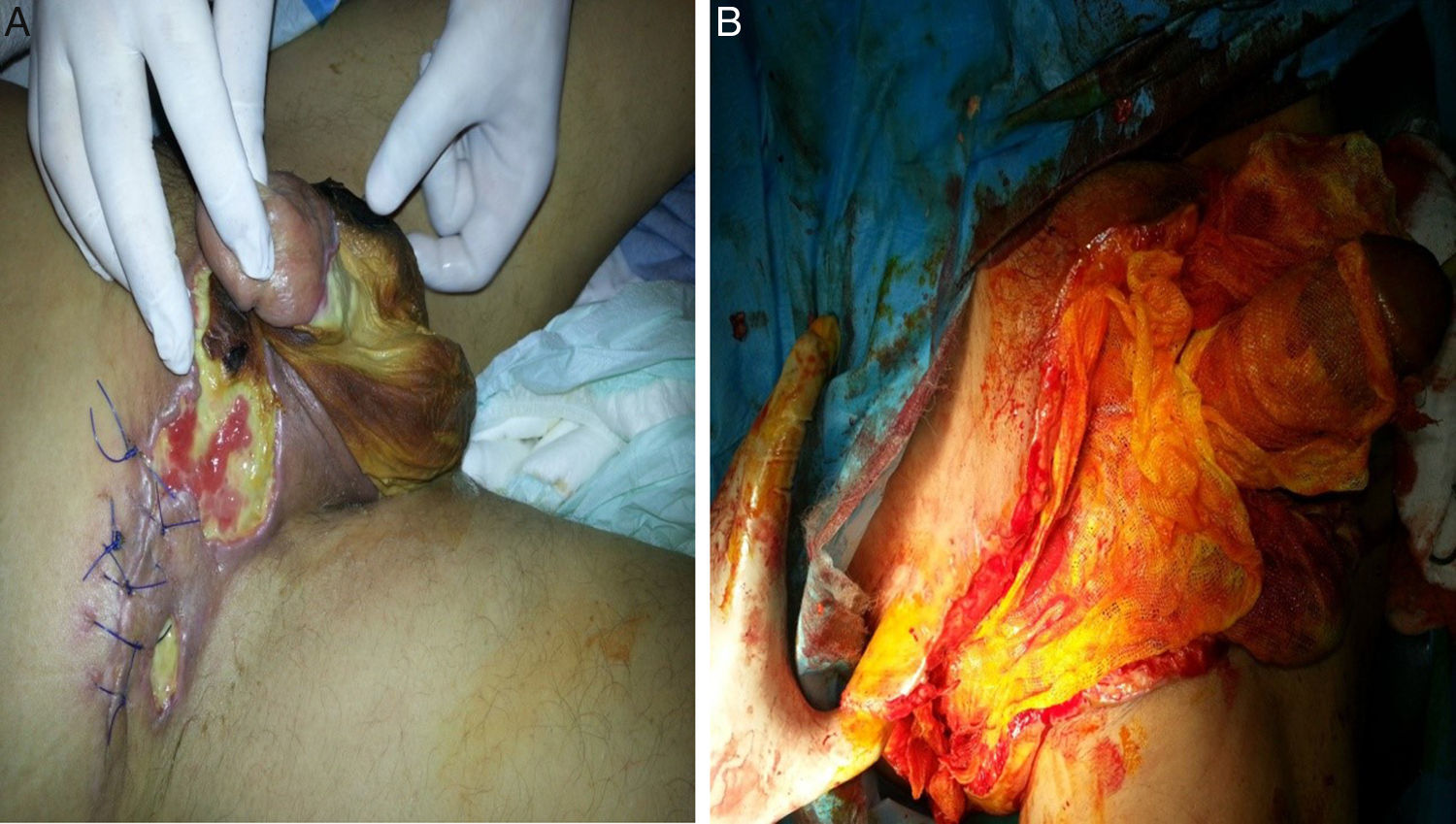
On postoperative 1st day after right inguinal hernia repair, scrotal hematoma was developed which necessitated evacuation. Afterwards cellulitis which was starting from the incision line, aggravated to diffuse subcutaneous abscess formation. Then a subcutaneous drainage catheter was placed in the right lower abdominal quadrant for abscess drainage. In addition, the patient received hyperbaric oxygen therapy and intravenous antibiotherapy for 10 days. Subsequently, the patient consulted to our department. His physical examination revealed an edematous, necrotic and infected area extending from the right lower abdominal quadrant to penoscrotal region. The lesion was much closed to the anal region. Penile shaft all the way to the glans was also involved (Fig. 1A).
Ultrasound report revealed that both testicular arterial and venous blood supply were normal and symmetrical. Wound culture disclosed growth of multiple microorganisms with a gram-positive predominance.
From the first day of his hospitalization, metronidazole and ceftriaxone treatment was initiated. After informed consent of the patient was obtained, an extensive surgery debridement encompassing the scrotal region was planned. Scrotum was totally resected but testicles were preserved. Even though infected necrotic area was extending up to the level of spina iliaca anterior superior, all of necrotic tissues were excised (Fig. 1B). Appropriate dressings were applied and upon observance of surgical improvement on postoperative 7th day, he was discharged. Then we consulted him to the clinic of plastic and reconstructive surgery. Postoperative 2nd month, appearance of the surgical area was pointing a healing (Fig. 2).
DiscussionFournier's gangrene is a well-known, often fatal fasciitis of the pelvic floor with infectious etiology. Predisposing factors include diabetes because of microangiopathy and polyneuropathy, alcoholism, immune-defects, and consumptive diseases.4 Fournier's gangrene begins as a local infection that is caused by bacteria inhabiting the lower gastrointestinal tract, urogenital tract or the perineum. The synergistic action of aerobic and anaerobic organisms plays a major role in the progressive course of the infection.5 An understanding of the spread of Fournier's gangrene requires knowledge of the fascial structures of the pelvic floor and anogenital region. Colles’ fascia, which is the superficial fascia of the perineum, plays an important role in this context.6 The Dartos fascia is the continuation of this layer over the scrotum and penis. Colles’ fascia is attached to the urogenital diaphragm and merges with Scarpa's fascia of the anterior abdominal wall. The spread of infection along these fascial planes was reported in Fournier's original description of a gangrene ‘de la verge’.
Generally, E. coli, P. aeruginosa, S. aureus and Bacteriodes were reported as the mainly agents. However in the large recent studies the anaerobic culturing rates were in a wide range (7–38%) but it should be considered that anaerobic culturing techniqually more difficult than the routine ones. Depending on this literature knowledge, we observed that the role of anaerobic bacterium in Fournier's gangrene was declining. The hyperbaric oxygen therapy for anaerobes loosed its popularity during last decade among the treatment modalities.7 So that surgery is still considered as the first line treatment in Fournier's gangrene.
Hernia is a general term describing a bulge or protrusion of an organ or tissue through an abnormal opening within the anatomic structure. Although there are many different types of hernias, they are usually related to the abdomen, with approximately 75% of all hernias occurring in the inguinal region.8 Inguinal hernias have a 9:1 male predominance, with a higher incidence among men 40–59 years of age.8 The most common complications of hernia repair are hematomas, including penile or scrotal ecchymosis; seromas; and wound infection. Although these are uncommon, family physicians should be vigilant because patients may present to them postoperatively. Chronic pain is the most common long-term problem after hernia repair, occurring in 5%–12% of the patients and is related to nerve scarification, mesh contraction, chronic inflammation, or osteitis pubis.
In the literature a few case reports on Fournier's gangrene developed during postoperative period have been cited. Al-Ali et al. reported a case of Fournier's gangrene developed in a 78-old-male patient after elective hydrocelectomy.9 Patel et al. reported a case of Fournier's gangrene in a 31-year-old male-patient after vasectomy performed under local anesthesia and they were compelled to carry on radical resection.10 Onakpoya et al. reported a case of Fournier's gangrene in a 75-year-old male patient developed following ruptured Richter's hernia.11
Development of Fournier's gangrene was not anticipated after inguinal herniorrhaphy. Our literature review revealed that ours was the second case observed after elective inguinal hernia operation. Firstly, Dinc et al.12 were reported Fournier's gangrene as a postoperative complication of inguinal hernia repair. They performed orchiectomy ipsilateral side of the inguinal hernia but we preserved testicles.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors declare no conflict of interest.
Haydarpasa Numune Research and Training Hospital, Istanbul, Turkey.