To examine the opinions, attitudes and perceptions of patients regarding the diagnosis and treatment protocols of erectile dysfunction (ED) and premature ejaculation (PE) and their interaction with the urology specialists.
Material and methodsObservational, national and multicentric study based on a self-designed online questionnaire in which ED and PE patients described their perception of ED and PE at diagnosis and during treatment and monitoring, the patient-physician relationship and the role of the patient's partner in the course of the disease.
Results306 ED and 70 PE participants were recruited. After the occurrence of the first symptoms, the time elapsed until the patient decided to go to the doctor was 28.6 months for PE and 14.0 months for ED (p<0.001). ED patients saw physicians more frequently (especially those aged between 60 and 69 years: 60.7%, p<0.001) than PE patients (52.1% vs 36.8%, respectively; p<0.001) and discussed this problem with their partner more (34.0% vs 22.8%, p<0.001). These disorders were mainly diagnosed at the urologist's office (ED: 74.8% vs 42.5%; PE: 75.7% vs 34.3%; diagnosis vs detection). One third of all participants reported that the sexual problem was not the main reason for the visit. The time elapsed between the first consultation for related symptoms and therapy was 8.7 months (oral drugs) and 7.6 months (dapoxetine) for ED and PE, respectively. ED patients and their partners felt particularly better once treatment had started (p<0.001). PE patients presented the highest degree of sexual dissatisfaction (78%). 50% of the patients agreed with the statement that initiating a discussion about sexual concerns was regarded as taboo and most of them did not say that their partner had encouraged them to seek medical advice.
ConclusionA concerted effort is called for to expand ED and PE patients’ proactivity in taking care of their own and their partner's sexual health. Current therapies would appear to have a benefit in couples’ sexual relationships.
Analizar las opiniones, actitudes y percepciones de los pacientes respecto a los protocolos de diagnóstico y tratamiento de la disfunción eréctil (DE) y la eyaculación precoz (EP) así como su interacción con los especialistas en urología.
Material y métodosEstudio observacional, nacional y multicéntrico, a través de un cuestionario online predefinido, en el que los pacientes con DE y EP describieron su percepción acerca de la DE y la EP, en el diagnóstico, durante el tratamiento y seguimiento, así como la relación médico-paciente y el papel de la pareja en el trascurso de la enfermedad.
ResultadosSe incluyeron 306 participantes con DE y 70 con PE. El tiempo transcurrido, desde la aparición de los primeros síntomas hasta que el paciente decidió acudir al médico, fue de 28,6 meses para la EP y de 14,0 meses para la DE (p < 0,001). Los pacientes con DE acudieron al médico con mayor frecuencia (especialmente en edades entre 60 y 69 años: 60,7%, p < 0,001) respecto a los pacientes con EP (52,1 vs. 36,8%, respectivamente; p < 0,001) y comentaron más el problema con su pareja (34,0 vs. 22,8%, p < 0,001). El diagnóstico de ambas disfunciones se llevó a cabo principalmente en consultas de urología (DE: 74,8 vs. 42,5%; EP: 75,7 vs. 34,3%; diagnóstico vs. detección). Una tercera parte de todos los participantes indicó que el problema sexual no motivó principalmente la visita. El tiempo transcurrido, desde la primera consulta motivada por síntomas relacionados y el establecimiento de terapia, fue de 8,7 meses (fármacos orales) y 7,6 meses (dapoxetina) para la DE y la EP, respectivamente. Los pacientes con EP presentaron mayor grado de insatisfacción sexual (78%). De los pacientes estudiados, 50% mostró acuerdo con la afirmación de que iniciar una conversación sobre las preocupaciones sexuales se consideraba un tabú y la mayoría reconoció que su pareja no le había animado a la hora de buscar consejo médico.
ConclusionesEs necesario un esfuerzo coordinado para aumentar la proactividad de los pacientes con DE y EP en el cuidado de su propia salud sexual y la de su pareja. Las terapias actuales parecen favorecerían las relaciones sexuales en pareja.
Erectile dysfunction (ED) and premature ejaculation (PE) are major issues in men's health and have a significant effect on their physical and psychosocial health and on the quality of life of patients and partners alike.1–3 ED was described as the inability of getting and keeping a satisfactory erection during sexual intercourse,4 whereas PE was defined as a phenomenon that happens when a man's ejaculation occurs earlier than intended during sexual activity.5
Both patients and healthcare practitioners encounter many cultural or moral difficulties in addressing problems of a sexual nature during visits. This may be responsible for the scarcity of existing epidemiologic data on ED and PE and contributes to a considerable proportion of ED and PE patients remaining underdiagnosed and consequently undertreated. In our country, only 5% of males with erection problems are diagnosed with ED, of whom only 50% were treated, as reported by a population of 544 Spanish primary care physicians.6
The first epidemiologic research studies on ED and PE conducted in Spain demonstrated that 12.1% of males (1.5–2.0 million men) suffered from ED, though only 16.5% of them had seen a doctor.7 In December 2009, the Spanish Association of Andrology, Sexual, and Reproductive Medicine (ASESA) released the results of the Demographic Study on Premature Ejaculation (DEEP, unpublished), performed with 1000 Spaniards. DEEP showed that 43% of the study population (aged 18–59 years) suffer from PE at some point in their life, although only 38% of PE men felt that they should see a doctor.
The acknowledgement of these high rates of prevalence for ED and PE led to the need to reduce the commonality of underdiagnosis and undertreatment of both sexual conditions. We therefore hypothesised that the clinical management of ED and PE is suboptimal, which encouraged us to initiate the PANDORA Project (Overview of Erectile Dysfunction and Premature Ejaculation) Approach Recommendations [Panorama de la Disfunción Eréctil y la Eyaculación Precoz. Recomendaciones para su Abordaje]) in 2019. This research project was sponsored and designed by ASESA in collaboration with the Menarini group. PANDORA is a first-in-class sociological study that provides information about ED- and PE-related opinions, attitudes and perceptions of 3 different groups: the general healthy male population,8 urologists (also submitted to this Journal) and patients. This study includes the findings obtained in this last group.
In this study, we set out to assess ED and PE patients’ opinions, attitudes and perceptions of diagnosis and treatments, their interaction with urologists and the impact of these disorders on the sex life of the patients and their partners before and after diagnosis and treatment.
Material and methodsStudy setting and designThis was an observational and multicentric study developed and conducted in Spain with a sample of 306 patients with ED and 70 patients with PE. It should be noted that a total sample of 960 patients (n=600, ED; n=360, PE) was originally calculated to obtain a precision level of 4.4% (global) and of 4.9% for each subgroup of ED and PE subjects. However, the COVID-19 pandemic situation made it extremely difficult for patients to visit their specialist in person and the informed consent could therefore not be signed by the number of patients originally calculated, as would have been the case in normal (non-pandemic) circumstances. Therefore, based on these assumptions, the sample was finally comprised of 306 ED patients (precision achieved: 5.6%) and 70 patients with PE (precision achieved: 11.6%).
For this study, a self-administered online questionnaire was created and validated by a National and Regional Committee of the PANDORA project comprised of a group of 17 prestigious and highly-experienced Spanish andrologists (one per Autonomous Community). This objective of the survey was to conduct an observational study on ED and PE based on a quantitative methodology.
Patient selectionThe patients were selected consecutively; each investigator-urologist (n=30) included a maximum of the first 20 patients who came to their office for ED and the first 12 patients who attended a PE visit. The patients selected fulfilled the following inclusion criteria: be aged over 18 years with a known diagnosis of ED or PE, have seen the urologist for the routine control of their disorder and provide their written informed consent. Following recruitment, any ED or PE patients who turned out to be participating in a clinical trial related to any of these sexual conditions were excluded from our study. To guarantee strict screening, patients with any type of alteration that compromised their ability to grant their written informed consent and/or to comply with the study protocol were also excluded. Regarding ethical aspects, this study was approved as a post-authorization observational study by the Spanish Agency of Medicinal Products and Medical Devices (AEMPS). All the forms of the documents related to this study were approved by the Ethical Committee (EC) of the Hospital General Universitario Reina Sofía (Córdoba, Spain), which was chosen as the reference EC. All patient data extracted from each survey were anonymised for the analysis. The confidentiality commitment and statistical secrecy were maintained pursuant to the Pharmaceutical Industry Code of Ethics and the Regulation (EU) 2016/679, of 27 April 2016, the General Data Protection Regulation (GDPR) and the applicable national regulations.
Data collectionThe study questionnaire was designed to ascertain the opinion, attitude and expectations of ED and PE patients regarding: disease detection (onset of symptoms, time to visit and specialist seen, their degree of satisfaction with their sex life before treatment); diagnosis (time from diagnosis, specialist physician and healthcare setting) and treatment (time to treatment, therapeutic strategies, perception of efficacy and level of satisfaction with sex life after treatment); the patient-physician relationship; and finally, the partner's role in the course of and in the clinical monitoring of ED and PE. The questionnaire was also intended to describe the general profile of ED and PE patients in Spain (age, geographic region, educational level, employment situation, drinking and smoking habits).
Statistical analysisQualitative variables were described with frequencies and percentages. The quantitative variables were described by: n, mean, standard deviation, median, and interquartile range (IQR) according to their distribution. For the evaluation of the patient-doctor relationship and the partner's role in the disease, a 7-point ordinal Likert Scale (1, totally disagree-7, totally agree) was used to assess the respondents’ level of (dis)agreement. The Chi-Square (χ2) statistical test was used to compare contingency tables for nominal variables. For continuous variables, and when the assumptions of normality were met, the ANOVA test was performed, or failing that its non-parametric equivalent.
ResultsA final population of 306 ED and 70 PE patients (mean age 60.3 years in the ED group vs 46.5 years in the PE group; p<0.001), with over 50% of the sample having completed secondary or higher education, and mainly in employment, was included in this study. Alcohol intake (64.4% in ED, 33.0% intake 2–4 times a month vs 51.4% in PE, 44.4% intake 2–4 times a month) and smoking habits (24.8% in ED, average: 14.7 cigarettes/day; 33% in PE, average: 11.9 cigarettes/day) were the most prevalent self-reported conditions.
The differences in detection and diagnosis between ED and PE in Spain were investigated (Table 1). Significant differences were observed in the time elapsed between the onset of symptoms and when the patient decided to see the doctor (28.6 months for PE (median 12.0; Q1 6.0; Q3 24.0) compared to 14.0 months (median 12.0; Q1 6.0; Q3 18.0) for ED; p<0.001). More than 80% of the participants acknowledged the appearance of one or some of the symptoms of these sexual problems and went to a public healthcare centre. However, ED patients visited physicians more frequently (especially those aged between 60 and 69 years: 60.7%, p<0.001) than PE patients (52.1% vs 36.8%, respectively; p<0.001) and discussed this problem more with their partner (34.0% vs 22.8%, p<0.001), whereas PE participants admitted to having more proactively sought information about the disease on the Internet (35.1% vs 15.1%, p<0.001). Although the majority of men with ED above 70 saw a urologist (data not shown in the table; 60.8%, p=0.044), a primary care physician (PCP) was chosen by 51.3% of ED and 57.1% of PE cases as first option for their medical visit. Nonetheless, although these disorders were originally detection by PCPs, the conditions were diagnosed mainly by a urologist (ED: 74.8% vs 42.5%; PE: 75.7% vs 34.3%; diagnosis vs detection). No statistical difference was detected regarding the diagnosis rates of ED compared to PE, although these differences were reported by both groups when they stated the time between diagnosis and recruitment (4.2 years (median 2.8; Q1 1.7; Q3 5.2) as of the ED diagnosis vs 1.9 years (median 1.3; Q1 0.8; Q3 2.0) as of the PE diagnosis, p<0.001). About one third of the participants reported that their sexual problem was not the main reason for the visit, but rather that the topic emerged during the conversation with their doctor. More particularly, a subgroup of PE patients aged above 45 years was significantly less open or forthright about their sexual condition with the doctor (data not shown in the table; 41%, p=0.029), although the majority of them were diagnosed with acquired PE (92.3%, p=0.001).
Differences in detection and diagnosis between patients with ED (n=300) and patients with PE (n=70).
| Item investigated | ED | PE | p-Value |
|---|---|---|---|
| Time to seek medical help as of the onset of symptoms (average months) | 14.0 | 28.6 | <0.001 |
| Recognition of disease symptoms (% of patients) | 86.6 | 81.4 | 0.532 |
| Reaction to the onset of symptoms (% of patients) | |||
| • See the doctor | 52.1 | 36.8 | <0.001 |
| • Talk to partner | 34.0 | 22.8 | |
| • Search the Internet for symptoms | 15,1 | 35.1 | |
| • An issue related to stress/anxiety | 20.4 | 22.8 | |
| • Side effect of current medication | 14.7 | 1.8 | |
| • Talk to family and friends | 8.3 | 5.3 | |
| • Go to the pharmacist | 4.9 | 0.0 | |
| Time from diagnosis to recruitment in this survey (average years) | 4.2 | 1.9 | <0.001 |
| Physician diagnosing the sexual disordera(% of patients) | |||
| • Urologist | 74.8 | 75.7 | 0.444 |
| • PCPb | 19.6 | 17.1 | |
| • Cardiologist | 1.6 | 0.0 | |
| • Psychiatrist | 0.7 | 0.0 | |
| • Endocrinologist | 0.7 | 0.0 | |
| • Other | 1.3 | 4.3 | |
| • Undisclosed | 1.3 | 2.9 | |
PCP, primary care physicians.
After the onset of symptoms, PCP were chosen for the first visit by 51.3% of patients with ED compared to 57.1% of patients with PE (p=0.617), but the disease was not diagnosed unless patients were referred to the urologist. p-value: statistical differences were observed among the surveyed population when the answers were grouped by type of disease (patients with ED vs patients with PE).
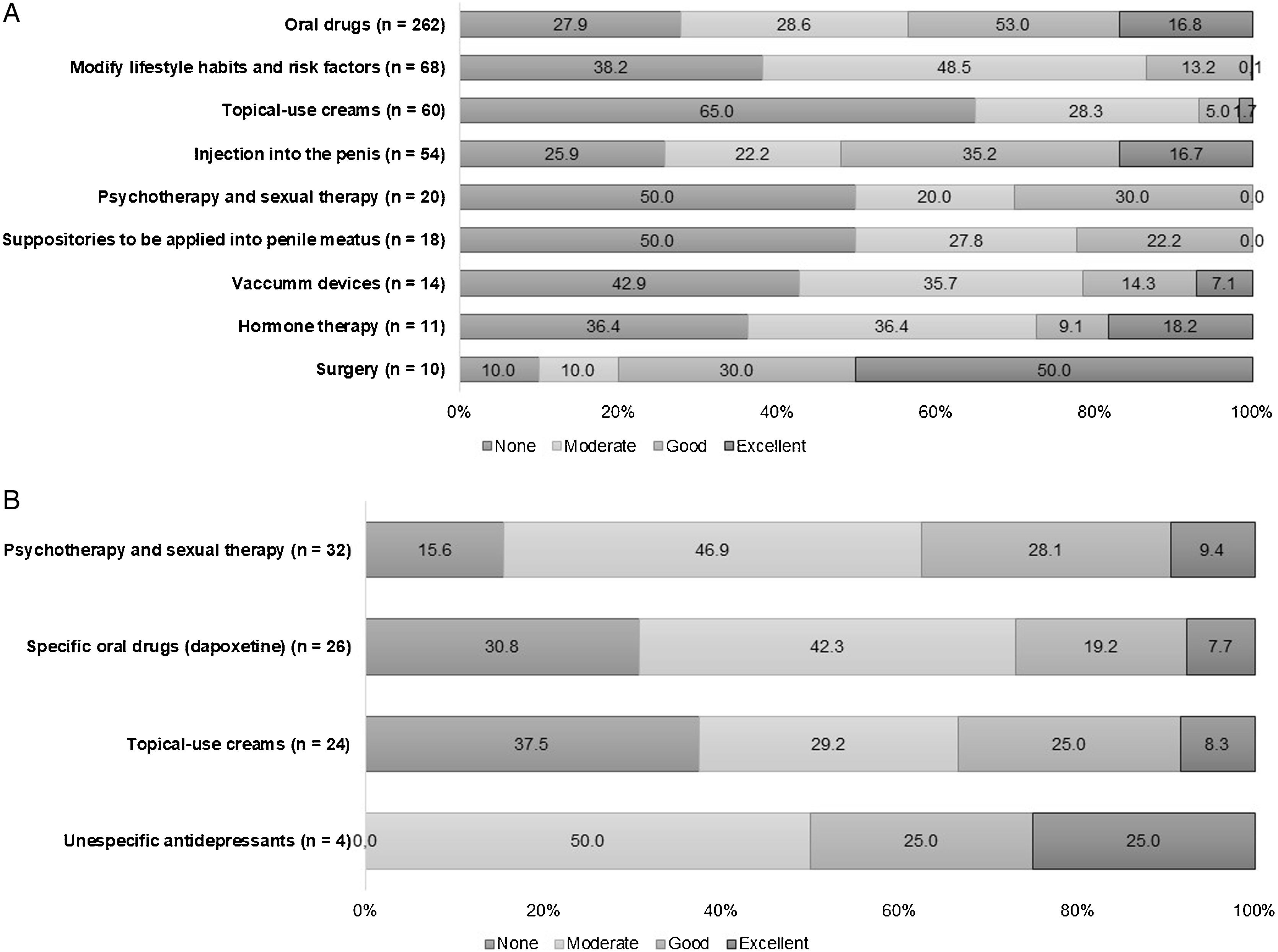
The study population was also questioned about different topics related to their treatment: treatment start time and the corresponding reported efficacy (Fig. 1). The time elapsed between the first consultation for related symptoms and treatment was not statistically different between ED (8.7 months (median 6.0; Q1 3.0; Q3 12.0)) and PE patients (7.6 months (median 5.5; Q1 2.0; Q3 10.5)) and the vast majority of cases in both groups had received a therapeutic regimen when they were recruited (ED: 91.2% and PE: 84.3%; data not shown). An in-depth analysis of the type of treatment used and the corresponding participant-perceived degree of efficacy showed that oral drugs had been used by 93.5% (n=262) of the patients in the ED cohort (Fig. 1a), whereas other therapies such as hormone replacement or surgery were used residually (3.9% in both cases). Paradoxically, oral therapies were reported to be inefficacious by two thirds of the respondents and efficacy was rated as ‘Excellent’ by half of the cohort who underwent a surgical procedure and by nearly 20% of those in whom a hormone therapy regimen had been initiated. A non-pharmacological approach was used by 54.2% of the PE patients, although its efficacy seemed to be highly questioned by at least 62.5% of the sample (Fig. 1b). Of the pharmacological therapies, dapoxetine, which holds a specific authorisation for the treatment of PE, was prescribed in 42.4% of the cases (n=26). 42.3% (11/26 reports) of the patients that were given treatment with dapoxetine rated its efficacy as moderate. Interestingly, despite the fact that oral antidepressants were used by only 4 patients, it accounted on a ‘Good’ to ‘Excellent’ efficacy selected by 2 of those treated with these non-specific PE drugs (Fig. 1b). Topical creams for PE were prescribed in 24/60 PE patients, although their potential to improve ejaculatory latency seemed to be null for 37.5% of this subgroup (9 out of 24).
Patient-reported perceived efficacy of each therapeutic option. The participants diagnosed with ED (n=300) or PE (n=70) rated the efficacy related to the ED (a) and PE (b) treatment options. When indicated, data are shown as a percentage (%) of the patients who rated treatment efficacy as None/Moderate/Good/Excellent. No statistical differences were observed in the surveyed populations with ED vs PE for any therapeutic option. ED, erectile dysfunction; PE, premature ejaculation.
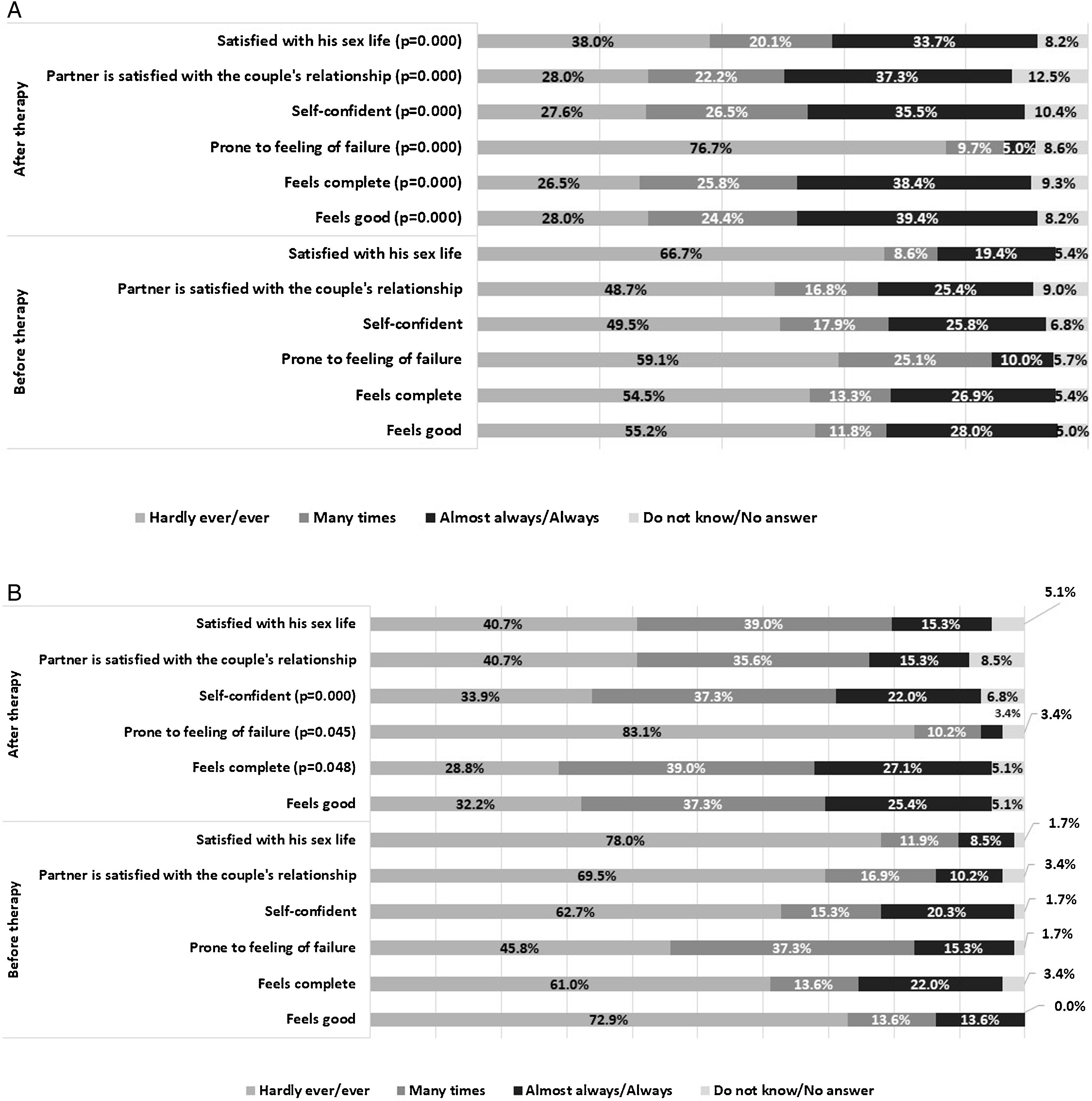
Sex life changes reported by patients before and after treatment were also assessed (Fig. 2). All the males included in this study answered some questions about the impact of treatment on their sexual experiences and their partner's degree of satisfaction with their sex life, self-confidence, propensity to failure, and feeling of completeness as a man and self-worth. In the cohort of patients with ED who received treatment (n=279), statistically significant differences were observed for all items following the comparison of their experience of sexual intercourse before and after treatment (Fig. 2a). ED patients and their partners particularly felt better once the treatment had been started (p<0.001). PE patient records present a scenario of greater distress, with the highest prevalence of sexual dissatisfaction (78%) until they were treated. However, the diagnosis and treatment of PE contributed significantly to their evincing an attitude less prone to the feeling of failure (p=0.045), a deeper sense of completeness reported by almost 70% of the study cohort (p=0.048) and greater self-confidence with sexual intercourse (35% in untreated vs 60% in treated PE patients, p<0.001) (Fig. 2b). Treatment correlates also included the partner's satisfaction, particularly in couples affected by ED, in which the partners were statistically more satisfied than in PE couples (49.8% vs 23.8%, respectively, p=0.003).
Sex life changes in the surveyed patients before and after treatment in (a): men with ED (n=279); and in (b): men with PE (n=59). When indicated, data are shown as a percentage (%) of the patients who stated that they experienced any of the items specified in the graph by different levels of frequency: Hardly ever/Never/Seldom, Very often, Mostly/Almost always/Always and Do not know/No answer. Statistical differences were observed between the surveyed populations with ED or PE when the answers were grouped before vs after therapy (ED: * p<0.001 for all items after therapy; PE: *p=0.003; **p=0.045; ***p=0.048). ED, erectile dysfunction; PE, premature ejaculation.
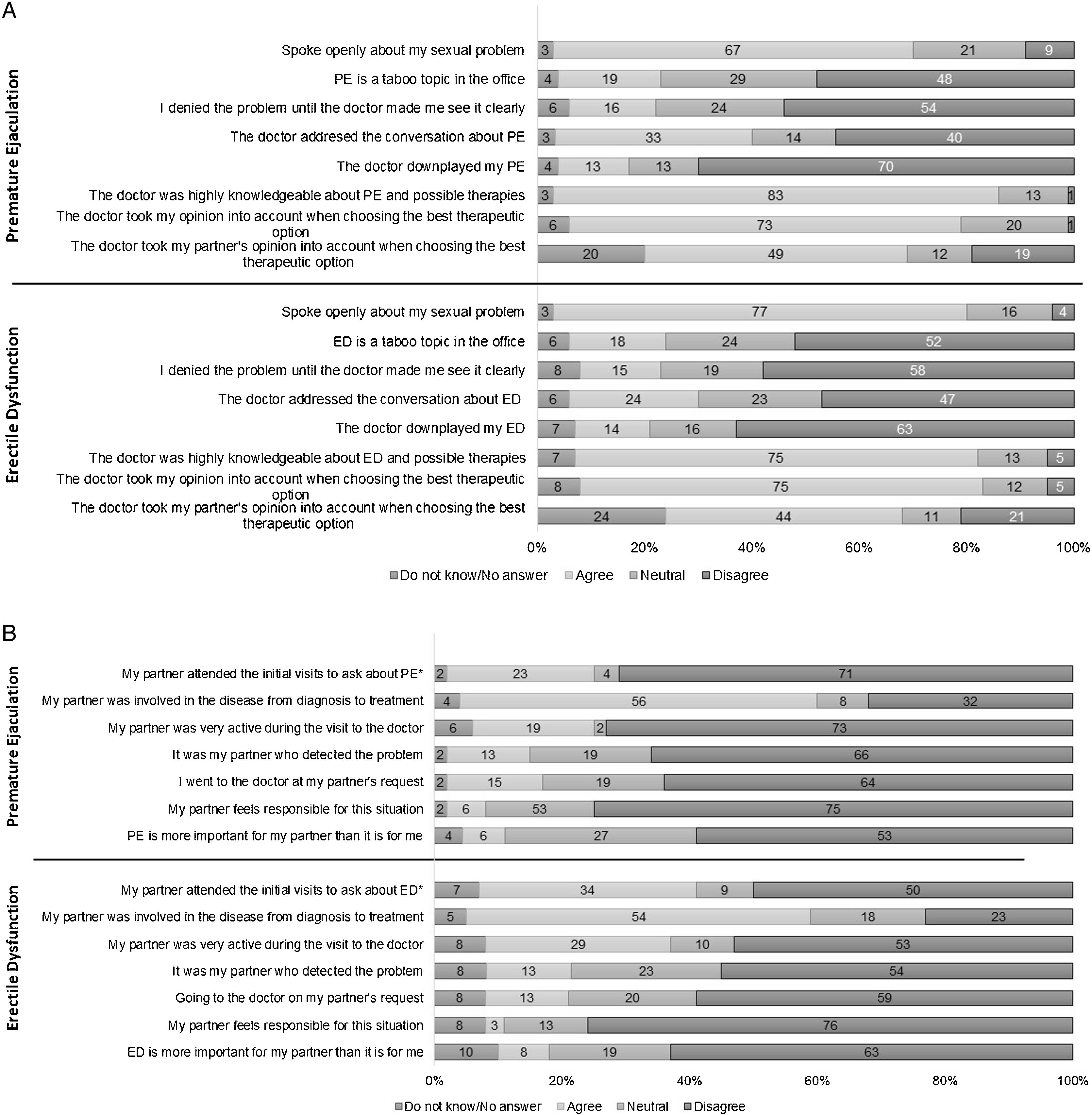
This survey reflected the communication between patients and physicians, as well as the impact of ED and PE on the couple's relationship (Fig. 3). In the survey overall, a high percentage agreed that the doctor took the patient's opinion into account in choosing the best treatment (76% for ED and 73% for PE), although they did not pay a great deal of attention to their partner's opinion (44% for ED and 49% for PE) (Fig. 3a). Approximately 80% of the entire population of participants concurred that their doctors had extensive knowledge of both disorders and the possible therapies and they could talk openly to their doctor about ED (77%) or PE (67%) problems. Nonetheless, half the sample population agreed with the statement that initiating a discussion on sexual concerns of this nature was ‘taboo’, especially elderly subjects (≥70 years; 21.6%, p=0.011). A range of 60–70% of respondents did not agree that their physicians downplayed the occurrence of male sexual diseases (Fig. 3a).
Patients with ED (n=306) and PE (n=70) answered questions about a set of statements related to their communication flow with their doctor (a). Patients with ED (n=239) and PE (n=48) responded to questions about a set of statements related to the impact of these disorders on the couple's relationship and sex life. When indicated, data are shown as a percentage (%) of agreement. The agreement score ranged from 1 (strongly disagree) to 7 (strongly agree). *Statistical differences were only observed among the surveyed population for the item ‘My partner attended the initial medical visits’ (partners accompanied more in ED compared to PE; p=0.048). ED, erectile dysfunction; PE, premature ejaculation.
About one third of the sample whose marital status had changed indicated that this change had largely been prompted by their sexual problem (10/30 ED cases; 2/6 PE cases). In this regard, the questions shown in Fig. 3b helped us to understand the roles of ED and PE couples and the differences between them. Just over 50% of the respondents agreed that their partners were thoroughly involved, from diagnosis through to the treatment of the disease, although they did not accompany the patients in the initial visits (34.3% for ED vs 22.9% for PE; p=0.048) and nor did they actively share their impressions about the problem (52.7% for ED vs 72.9% for PE). ED and PE patients mostly disagreed with the statements that their partner felt responsible for the situation (76.2% vs 75%, respectively), attached greater importance to the disease than the actual patient (63.6% vs 62.5%), was the one who detected the problem (54.8% vs 66.7%) or encouraged the patient to seek medical advice (59.4% vs 64.6%).
DiscussionEarly ejaculation and difficulty sustaining an erection produce feelings of distress that have a profound impact on the individual's perception of their sex life quality.9,10 However, they are still the most underdiagnosed, and therefore the most undertreated, disorders.11
The prevalence and related risk factors of ED and PE among middle-aged and older adults have been investigated in a number of studies, although there are no studies about the sociological map of these sexual disorders.12–14 To this end, ASESA led the PANDORA study, an original initiative launched in Spain to obtain the most accurate map possible of the different stakeholders in ED and PE: specialist physicians, undiagnosed healthy males and a significant and representative population of patients with ED or PE. This survey includes the viewpoint of a large cohort of ED and PE patients about the detection, diagnosis and therapies of both disorders.
In general, and regarding symptom detection, the help-seeking behaviour patterns observed in our survey were similar to those published by other studies.15 Spanish patients were very inactive in seeking medical help for their sexual problems, particularly PE patients, who see the doctor or talk to their partner less frequently than ED patients.
These results are in line with those of the first study of the PANDORA project,8 showing that around 70% of Spanish men barely ever worry about ED or PE. In another Spanish study, of a total of 512 males who had experienced some kind of erection issue, only 20% had sought a medical solution to their problem, taking 1.7 years on average to do so.16
As described elsewhere,17 patients do not seek help from the urologist or other specialists out of feelings of shame and embarrassment. In addition, many of the affected may not fully comprehend the gravity of ED or PE and may put off seeking help until the sexual problem becomes extremely severe. Actually, in our study sexual problems were not the main reason for seeking medical aid in more than one third of the participants, as had already been demonstrated by our group.8 Only 9.5% and 25% of a cohort of 2515 healthy males had seen a doctor for a possible diagnosis of PE and ED, respectively.
The time to self-reported PE diagnosis seems to be lower than that of ED (1.9 vs 4.2 years, respectively). Several studies have observed this difference, showing that the prevalence of self-reported PE may be lower because it is confounded with other sexual dysfunctions, particularly ED.18,19
Our investigation shows that oral therapies are prescribed mostly among ED patients, although their efficacy is much more poorly rated than other strategies that are used far less, such as testosterone replacement or penile surgery. Both sexual satisfaction and rigidity of erection scores increased with primary testosterone supplementation, unless in patients with hypogonadism.20 Penile prosthesis implantation is considered a valuable option for ED patients who do not respond to pharmacotherapy or seek a permanent solution to their problem.21 One year after surgery, patient-reported satisfaction was high in terms of prosthesis function, their relationship with their partner and their perceived self-image,22 and the treatment was found to continue to work properly even>10 years after the original implant.23
Non-pharmacological psychological/behavioural therapies and several types of pharmacotherapy, such as topical anaesthetic agents, phosphodiesterase type 5 inhibitors, antidepressants and some opioids have been reported to treat PE with varying degrees of success, although they are all off-label uses for PE treatment.24 According to our results, most PE patients did not see much benefit from the non-pharmacological approach, despite the fact that it was used in more than 50% of the cases. Albeit with moderate efficacy, dapoxetine seems to be generally prescribed among our PE study population. This result may be explained by the fact that dapoxetine, a short-acting serotonin reuptake blocker which can prolong intra-ejaculatory latency time, is the only oral medication licensed for the on-demand treatment of PE.25 However, 30% of our study sample claimed a lack of efficacy of dapoxetine treatment. This finding is consistent with clinical practice reports, in which one third of PE cases discontinue dapoxetine treatment within 1 month mainly due to unmet expectations and side effects.26 On the contrary, the efficacy of using topical anaesthetics to treat PE was rated as good to excellent by more than 60% of the sample.
ED and PE are associated with a reduction in sexual functioning, sexual satisfaction and quality of life, which may further result in mental health concerns and interpersonal difficulties.27 In the current study, we assessed the relative impact of these disorders in men, quantifying different items related to sex life (levels of self-confidence, satisfaction, feeling of failure and completeness) before and after treatment. Proven therapies resulted in an improved sexual behaviour profile for both ED and PE patients, although the records seem to favour ED, with a significant higher degree of satisfaction among patients and their partners. Indeed, the number of partners in ED couples stated to be more satisfied after ED therapy has been started (25% prior to vs 40% after treatment; p<0.001). In terms of related findings, the female partners of men with ED are known to report a substantial decline in all sexual function aspects.28 Therefore, the treatment of the male partner's ED results in a substantial improvement in the female partner's sexual function.29,30 In our study, PE respondents also reported considerably low sexual satisfaction rates and a general feeling of failure and unhappiness with themselves. These results are in line with previous findings, where men's dissatisfaction correlated strongly with the dissatisfaction they attributed to their partner.31
Finally, this study offers a complementary view based on patient-physician communication and a couple-focused perspective. Spanish urologists are rated as knowledgeable physicians who take the patient's opinion into consideration when prescribing a treatment and are willing to talk about patients’ sexual problems without downplaying them. However, and in line with our previous research,8 sexuality continues to be a taboo subject for half of the participants and heightens with age. Several studies have demonstrated that it is common for men not to acknowledge that they have a sexual disorder, underestimate it or feel too embarrassed to discuss it with their doctor.15,32 Although our objective was to emphasise that PE and ED should be regarded as a problem to be shared between men and their partners, nearly 50% of the patients surveyed claimed that their partner's opinion was not taken into account during visits.
While several studies have investigated the effects of ED and PE on the partner's sexual function, the partner's role in diagnosis and treatment is usually ignored. In this survey, the patients quantified the extent of their agreement with certain statements related to their partner's role during the initial appointments with the specialist to discuss the sexual dysfunction and its diagnosis. More than 50% of the panel agreed that their partners were involved throughout the disease process, from diagnosis to treatment. Nevertheless, most patients disagreed that their partner felt responsible for the problem, was the one who detected the problem, insisted that their partner seek medical help or even attached greater importance to the problem than the actual patient. Our results do not coincide with the reports of other groups,27,33 who have provided scientific evidence of the partner's crucial role in medical procedures for addressing ED or PE.
Some significant shortcomings of our study were the heterogeneity of the respondents, from different regions of Spain with different diagnostic and treatment programmes, as well as the receptiveness and interest of ED and PE patients to address their disease, which might not be representative of the general Spanish patient population. Another limitation of this study was a direct consequence of the COVID-19 pandemic, which rendered it impossible to recruit a larger sample size (376 patients recruited vs 960 patients originally intended). However, to the best of our knowledge, there are no published surveys other than our own that describe patient perceptions related to the management and impact of PE and ED. It would be worthwhile to compare the outcomes of this study to the results obtained from the group of Spanish urologists (submitted to this Journal) to see if their clinical patterns correspond to patient perception and needs.
ConclusionsThis is a first-in-kind study developed in Spain, gathering the opinions, attitudes and perceptions of ED and PE patients regarding the diagnosis, treatment and quality of sex life in a couple's relationship and the role of the partner during the clinical course of these disorders. Spanish patients put off seeking medical aid, and one third of them still do not regard a sexual disorder as a cause for concern and a reason to see a doctor. Most treatments used in ED (oral therapies) and PE (dapoxetine) proved to have a significant benefit in sexual intercourse for patients and their partners. The patients regarded the specialist physicians as well-versed in sexual diseases and open to discussing treatment options, although broaching the subject of sexual problems continues to constitute a major difficulty for patients in the doctor's office. Surprisingly, however, and while the partners were considered to be involved from diagnosis through to the treatment of these sexual diseases, their role was not as relevant as has been cited throughout the literature.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingPANDORA is an initiative of the Spanish Association of Andrology, Sexual and Reproductive Medicine, which has been funded with an unconditional grant from Grupo Menarini España.
Conflicts of interestPuigvert-Martínez AM and Prieto-Castro R have received personal fees from Menarini. Artigas-Feliu R, Cruz-Culebra N and Illán-Mateo P work in the medical department of Menarini.
The authors would like to thank all the members of the PANDORA Project Regional Committee for their contribution to the development of the research and drafting of the manuscript: Alcaraz Reverte, José Pascual (Policlínico Hospital Perpetuo Socorro, Murcia); Arrondo Arrondo, José Luis (Hospital de Navarra, Navarra); Campos Juanatey, Félix (Hospital U. Marqués de Valdecilla, Cantabria); Corral Molina, Juan Manuel (Hospital Clínic i Provincial de Barcelona, Barcelona); Cortiñas González, José Ramón (Hospital U. del Río Hortega, Valladolid); Fernández Rosaenz, Jesús (Hospital Viamed Los Manzanos, La Rioja); Jorge Manuel González Suárez (Hospital Universitario Central de Asturias); Gutiérrez Hernández, Pedro Ramón (Hospital U. de Canarias, Santa Cruz de Tenerife); Jara Rascón, José (Hospital General U. Gregorio Marañón, Madrid); Leibar Tamayo, Asier (Hospital U. Infanta Sofía, Madrid); Martínez Jabaloyas, José María (Hospital Clínico U. de Valencia, Valencia); Mateos Blanco, Jesús (Hospital U. de Badajoz, Badajoz); Meijide Rico, Fernando (Hospital Povisa de Vigo, Pontevedra); Rodríguez Vela, Luís (Hospital U. Miguel Servet, Zaragoza); Rosselló Gayá, Mariano (Instituto Médico Rosselló, Balearic Islands); Valero Rosa, José (Hospital U. Reina Sofía, Córdoba); Vela Jiménez, Francisco José (Hospital General U. de Ciudad Real, Ciudad Real).