To investigate the sexual function in patients with macromastia and their partners.
Materials and methods48 patients with macromastia and 30 healthy controls and their partners were enrolled in the study. The sexual function of the women and their partners was evaluated by using the Index of Female Sexual Function (IFSF) and International Index of Erectile Function (IIEF), respectively.
ResultsMean ages of the patients and controls were respectively, 33.27±5.24 and 32.06±3.91 (p>0.05). Mean IFSF scores of the patients and controls were 23.21±3.16 and 27.33±4.94 (p=0.00), respectively. All of the subscale scores of IFSF in the patient group were significantly lower than in the control group. Mean IIEF scores of the patients’ and controls’ partners were 60.33±11.46 and 65.25±6.18 (p=0.04), respectively.
ConclusionIn this study, Macromastia was shown to affect sexual function of women and their partners adversely.
Investigar la función sexual en pacientes con macromastia y en sus parejas.
Material y método48 pacientes con macromastia y 30 controles sanos y sus parejas fueron inscritos en el estudio. La función sexual de las mujeres y sus parejas fueron evaluadas usando el Índice de Función Sexual Femenina (IFSF) y el Índice Internacional de Función Eréctil (IIEF), respectivamente.
ResultadosLa edad media de los pacientes y controles era de respectivamente 33,27±5,24 y 32,06±3,91 (p>0,05). Las puntuaciones medias de los pacientes y los controles eran de respectivamente 23,21±3,16 y 27,33±4,94 (p=0,00). Todas las puntuaciones en subescalas de IFSF en el grupo de los pacientes eran significativamente más bajas con respecto al grupo de control. La media de las puntuaciones del IIEF en las parejas de los pacientes y de los controles eran de respectivamente 60,33±11,46 y 65,25±6,18 (p=0,04).
ConclusionesEn este estudio, se demostró que la macromastia afecta la función sexual de las mujeres y sus parejas negativamente.
Macromastia is a common condition that negatively impacts the physical and mental health of adult women who have this disorder.1 Discomfort associated with large breast can include symptoms which present as: painful bra strap grooves ulceration from bra straps cutting into shoulders, chronic rash of the inframammary fold, upper and lower back pain, neck and shoulder pain, paresthesis of the arms and hands, headaches, painful kyphosis, and breast tenderness. They also have difficulty performing various physical exercises and daily activities, participating in sports or simply finding well-fitting bras or clothes.2 These physical complaints combined with psychological and social complaints can lower the patients’ quality of life.3
According to the National Health and Social Life Survey more women (43%) than men (31%) reported sexual problems. Of women who report any type of sexual difficulty, difficulty with sexual desire is the most common (mean 64%), followed by difficulty with orgasm (mean 35%), difficulty with arousal (mean 31%), and sexual pain (mean 26%).4 Sexual dysfunction is a term used to describe various sexual problems with overlapping biological, psychological, and interpersonal etiologies.5 Therefore, it is important to determine any underlying disorders or contributing biopsychosocial factors when evaluating a patient with sexual problems. Sexual dysfunction may actually be a symptom or side effect rather than a primary pathology.6
We hypothesized that macromastia may probably cause sexual dysfunction along with other symptoms mentioned above. In the present study, we investigated the sexual dysfunction in patients with macromastia and their partners by using, respectively, the Index of Female Sexual Function (IFSF)7 and International Index of Erectile Function (IIEF) to compare healthy women and their healthy partners.
Materials and methodsSubjects and study designThe study comprised 48 consecutive women with macromastia who had attended the plastic and reconstructive surgery clinic as outpatients and 30 healthy controls, and their partners. The patients were diagnosed with bilateral macromastia by plastic surgeons and had no history of breast surgery. Since there is no universally accepted definition for macromastia,8 all women presenting macromastia and demanding to have breast reduction, between July 2013 and February 2014, were invited to participate in the study. Patients with any disease that would affect their sexual function (e.g. genitourinary, gynecologic or psychiatric disorders, and malignancy) or patients with menopause were excluded from the study. Volunteer women in the control group were selected among healthy staff in our hospital. All participants were married and were informed about the aim of the study, and written consent forms were obtained from the couples. The study protocol was approved by the ethics committee of our institution.
InstrumentsIFSF was used to assess sexual function of the women in the patient and control groups. Sexual functions of their partners were assessed by using IIEF.
IFSF is used to quantify the female sexual function over the past month. It is psychometrically sound, easy to administer and has demonstrated ability to discriminate between clinical and non-clinical populations. This test is derived from the adaptation of the International Index of Erectile Function described by Rosen himself.7 The scale consists of 19 items divided into six subscales including sexual desire, sexual arousal, lubrication, orgasm, sexual satisfaction, and sexual pain with 2, 4, 4, 3, 3 and 3 items, respectively. The measure allows the calculation of specific indexes for each dimension as well as sexual function index (calculated through the sum of the specific dimensional indexes), with higher scores indicating greater levels of sexual functioning (desire: 1.2–6, arousal: 0–6, lubrication: 0–6, orgasm: 0–6, global satisfaction: 0.8–6, pain: 0–6, total: 2–36). Turkish version of the IFSF was validated by Aygin and Aslan.9
IIEF is used to assess the male sexual function over the past month. The scale consists of 15 items divided into five subscales including erectile function, orgasmic function, sexual desire, intercourse satisfaction, and overall satisfaction with 6, 2, 2, 3, and 2 items, respectively. The overall score ranges from 0 to 75, with higher scores indicating better sexual function. Turkish version of the IIEF was validated by Turkish Society of Andrology.10
Statistical methodsStudent's t test was used for comparison between data of the patient and control groups. Statistical analyses were done using the SPSS 13.0 (SPSS Inc). p value less than 0.05 was considered significant.
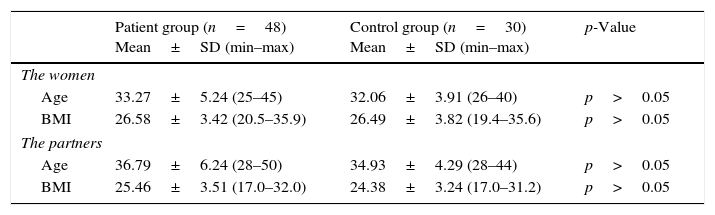
ResultsThe mean ages of the patient and control group were 33.27±5.24 years and 32.06±3.91 years (range: 25–45 years), respectively. The mean age and body mass index (BMI) of two groups were statistically similar (p>0.05). Table 1 shows the mean age and BMI of the women and their partners in the patient and control group.
The mean age and BMI of the women and their partners in the study groups.
| Patient group (n=48) Mean±SD (min–max) | Control group (n=30) Mean±SD (min–max) | p-Value | |
|---|---|---|---|
| The women | |||
| Age | 33.27±5.24 (25–45) | 32.06±3.91 (26–40) | p>0.05 |
| BMI | 26.58±3.42 (20.5–35.9) | 26.49±3.82 (19.4–35.6) | p>0.05 |
| The partners | |||
| Age | 36.79±6.24 (28–50) | 34.93±4.29 (28–44) | p>0.05 |
| BMI | 25.46±3.51 (17.0–32.0) | 24.38±3.24 (17.0–31.2) | p>0.05 |
BMI: Body mass index.
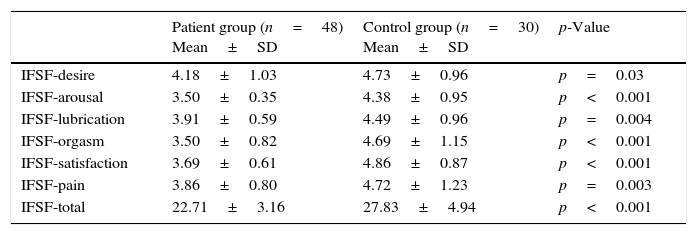
The IFSF scores were assessed as 22.71±3.16 in the patient group and 27.83±4.94 in the control group (p<0.001). Also, all the subscales of the IFSF were significantly lower in the patient group than the control group. Table 2 shows the mean of all the scores of the IFSF in the patient and control group.
The mean of the IFSF scores of the women in the study.
| Patient group (n=48) Mean±SD | Control group (n=30) Mean±SD | p-Value | |
|---|---|---|---|
| IFSF-desire | 4.18±1.03 | 4.73±0.96 | p=0.03 |
| IFSF-arousal | 3.50±0.35 | 4.38±0.95 | p<0.001 |
| IFSF-lubrication | 3.91±0.59 | 4.49±0.96 | p=0.004 |
| IFSF-orgasm | 3.50±0.82 | 4.69±1.15 | p<0.001 |
| IFSF-satisfaction | 3.69±0.61 | 4.86±0.87 | p<0.001 |
| IFSF-pain | 3.86±0.80 | 4.72±1.23 | p=0.003 |
| IFSF-total | 22.71±3.16 | 27.83±4.94 | p<0.001 |
IFSF: Index of female sexual function.
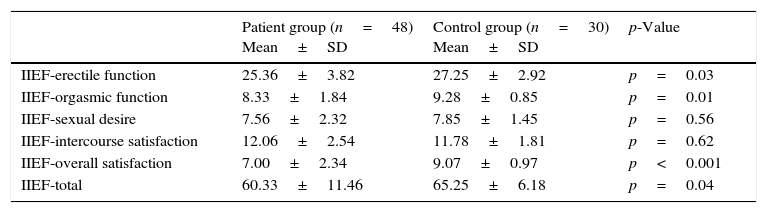
The sexual functions of the patients’ and controls’ partners were quantified with IIEF. The mean of the total IIEF scores in the patient group was significantly lower than the control group (p=0.04). Table 3 shows the mean of all the scores of the IIEF in the patient and control group.
The mean of the IIEF scores of the partners in the study.
| Patient group (n=48) Mean±SD | Control group (n=30) Mean±SD | p-Value | |
|---|---|---|---|
| IIEF-erectile function | 25.36±3.82 | 27.25±2.92 | p=0.03 |
| IIEF-orgasmic function | 8.33±1.84 | 9.28±0.85 | p=0.01 |
| IIEF-sexual desire | 7.56±2.32 | 7.85±1.45 | p=0.56 |
| IIEF-intercourse satisfaction | 12.06±2.54 | 11.78±1.81 | p=0.62 |
| IIEF-overall satisfaction | 7.00±2.34 | 9.07±0.97 | p<0.001 |
| IIEF-total | 60.33±11.46 | 65.25±6.18 | p=0.04 |
IIEF: International index of erectile function.
The present study was aimed at evaluating the sexual function of macromastia patients and their partners. Overall, the sexual function values for the women in the patient group were significantly lower than that of the control group, and this finding suggested that breast hypertrophy brings about an impairment in sexual function in women. The total IFSF scores of the women in the patient and control group were 22.71±3.16 and 27.83±4.94, respectively. Wiegel et al.11 found an IFSF total score of 26.55 to be the optimal cut score for differentiating women with and without sexual dysfunction. In the present study, when we assessed the IFSF scores of the patients with macromastia according to this cut off score, we found that 85% of the patients had sexual dysfunction. Also, all the IFSF subscales mean scores (desire, arousal, lubrication, orgasm, satisfaction, and pain) were significantly lower in the study group than in the control group.
So far, there have been two studies which investigated the sexual function of patients who had been operated for breast hypertrophy before.12,13 In both these previous studies, the authors used IFSF questionnaire to evaluate the sexual function of the patients. However, they did not make any assessment in patients with macromastia who had not been operated yet. So there was no information about the IFSF scores of the patients before the surgery. Romeo et al.12 compared sexual function in women who had undergone reduction mammoplasty and healthy controls and found that there is not any statistically significant difference in terms of sexual function between women who had undergone breast reduction and control group (normal, healthy women). Cerovac et al.13 also assessed the macromastia patients postoperatively and found that sexual function was reported as good in 53%, moderate in 19%, and poor in 28% of patients. However, they did not include healthy controls in their study. Therefore, these previous studies did not supply enough information about whether women with macromastia have impaired sexual function in comparison to healthy controls. Distinctively in the present study we recorded the IFSF scores of patients who had not undergone breast reduction yet. Therefore, our study is the first one, to our knowledge, evaluating the sexual function of women with macromastia who had not undergone breast reduction and of their partners in literature.
In the present study, the sexual functions of the patients’ partners were also quantified using IIEF form. The erectile function values for the patients’ partners were significantly lower than that of the controls (p=0.03). However, the means of the IIEF-erectile function scores in both the groups were normal for sexual function.14 All of the sub-group scores except sexual desire and intercourse satisfaction in the patient's partner group were significantly lower than the control group (Table 3). Overall, findings suggested that although the sexual functions of the men were adversely affected by the existence of breast hypertrophy of their partners, this effect did not cause sexual dysfunction.
This study had two limitations. The first limitation is the absence of the participants’ sex hormone profiles since sex hormone values may affect both female and male sexual function. The other limitation is that there was no post-therapy data of the women with macromastia. Further investigation comparing patient's values prior to and following surgery will put in evidence of a stronger relationship between mammary hypertrophy and sexual function.
ConclusionOur study indicates that most of the women with macromastia have sexual dysfunction and the sexual function of their partners is affected slightly. We suggest that women with macromastia should be questioned about their sexual function by using IFSF. Further studies may evaluate sexual improvement in women with macromastia and in their partners after reduction mammoplasty.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors declare no conflict of interest.