To evaluate the clinic efficacy and safety of the disposable circumcision suture device (DCSD) and Shang ring circumcision (SRC) in the treatment of redundant prepuce or phimosis with a meta-analysis.
Material and methodsElectronic databases including PubMed, Embase, Wan Fang, VIP, CNKI and CBM database were researched from inception to August 30, 2016 for relevant RCTs and prospective studies, the reference lists of the included studies were also searched manually. The risk ratios (RR) or mean difference (MD) with 95% confidence intervals (CI) as the effect sizes were calculated by the Revman 5.3 and stata12.0 software.
ResultsTwelve RCTs or prospective studies were included with 3345 patients among which 1661 cases received DCSD treatment and 1684 SRC. Compared to the Shang ring circumcision treatment, the disposable circumcision suture device provided a significantly shorter operation time [MD=−0.94, 95%CI (−1.76, −0.12), P=0.02], lower pain scores [MD=−1.89, 95%CI (−2.72, −1.07), P<0.001], no stitch removal pain, better postoperative penile appearance [RR=1.10, 95%CI (1.04, 1.17), P=0.001], fewer complications [RR=0.42, 95%CI (0.32, 0.56), P<0.001] and shorter wound healing time [MD=−8.92, 95%CI (−10.79, −7.05), P<0.001]. Meanwhile, there is more intraoperative blood loss [MD=0.12, 95%CI (0.02, 0.22), P=0.02], and more treatment cost [MD=877.57, 95%CI (737.94, 1017.20); P<0.001].
ConclusionsBased on the results of our meta-analysis, DCSD is more effective and safer than SRC. Thus, it has the advantages of shorter operation time, lower pain scores, better postoperative penile appearance, fewer complication and shorter wound healing time. However, the results need additional high-quality multicenter RCTs to evaluate in the future.
Evaluar la eficacia clínica y la seguridad en el tratamiento del prepucio redundante o fimosis con los dispositivos de sutura de circuncisión desechable (DCSD) y la circuncisión del anillo Shang (SRC).
Material y métodosSe investigaron las bases de datos en línea, como PubMed, Embase, Wan Fang, VIP, CNKI y CBM desde el inicio hasta el 30 de agosto de 2016 para ensayos controlados aleatorios y estudios prospectivos relevantes, así como las listas de referencias de los estudios incluidos. Las relaciones de riesgo (RR) o la diferencia de medias (MD) con intervalos de confianza (IC) del 95% (IC 95%) así como los tamaños del efecto se calcularon con el software Revman 5.3 y stata 12.0.
ResultadosSe incluyeron 12 ECA o estudios prospectivos con 3.345 pacientes, de los cuales 1.661 fueron tratados con el DCSD y 1.684 con SRC. En comparación con el tratamiento con SRC, el DCSD proporcionó un tiempo de operación más corto (MD=−0,94; IC 95% [−1,76, −0,12], p=0,02), sin dolor al extraer las puntadas (MD=−1.89; IC 95% [−2,72, −1,07], p<0,001), y mejor recuperación después de la cirugía (RR=1,10; IC 95% [1,04; 1,17], p=0,001), menos complicaciones (RR=0,42; IC 95% [0,32; 0,56], p<0,001)] y menor tiempo de cicatrización (MD=−8,92; IC 95% (−10,79, −7,05), p<0,001]. Mientras tanto, hay más pérdidas sanguíneas intraoperatorias (MD=0,12; IC 95% [0,02; 0,22]; p=0,02) y más costo de tratamiento (MD=877,57, IC 95% [737,94; 1.017.20]; p<0,001).
ConclusiónEl DCSD es más eficaz y más seguro que SRC según el resultado del metaanálisis. Por lo tanto, tiene las ventajas de un menor tiempo de operación, menores puntuaciones de dolor, mejor aspecto postoperatorio del pene, menor complicación y menor tiempo de cicatrización de la herida. Se necesitan ECA multicéntricos adicionales de mejor calidad en la evaluación debido a los límites de esta revisión sistemática.
Male circumcision (MC), dated back to more than 5000 years ago, represented an effective treatment for the penile malformations, has been performed with a prevalence of approximately 70% in the USA and 38.7% worldwide.1–3 There are large volumes of published trials describing the benefits of MC, including easier urination, improved penile topical hygiene, increased sexual pleasure and prevented urinary tract infections.4,5 Additionally, it has been demonstrated that it could reduce sexually transmitted diseases (STDs) passed by their female partners, penile cancer and cervical cancer associated with harboring human papilloma virus.6,7
There have been multiple methods of MC, such as sleeve circumcision, dorsal slit (DS), DCSD, SRC and the suture less circumcision using tissue glue. The most common forms are the conventional circumcision (CC) including World Health Organization (WHO) recommending forceps guided, dorsal slit, and sleeve resection methods.8 In these traditional forms, they have the disadvantages of adverse complications, inevitably suturing the incision, and cumbersome and time-consuming of the surgical procedure.8,9 Moreover, those methods require superior surgical technique to avoid the imperfect postoperative appearance, such as irregular hematoma.10,11 In contrast, DCSD and SRC, as two novel types of disposable circumcision devices, have substantial advantages which could simplify surgical process, shorten operative time, reduce adverse events, achieve a satisfying appearance, and seem to be more effective and safer than CC.12,13 However, it is still controversial which MC practices are more clinically acceptable between DCSD and SRC.
Recently, plenty researches compared DCSD and SRC in redundant prepuce and phimosis therapies, but obtained various outcomes due to the differences in research design, recruitment criteria and measurement methods. Therefore, we collected high-quality RCTs and clinical prospective studies to conduct an overall meta-analysis, comprehensively evaluating the clinical efficacy and safety of DCSD and SRC.
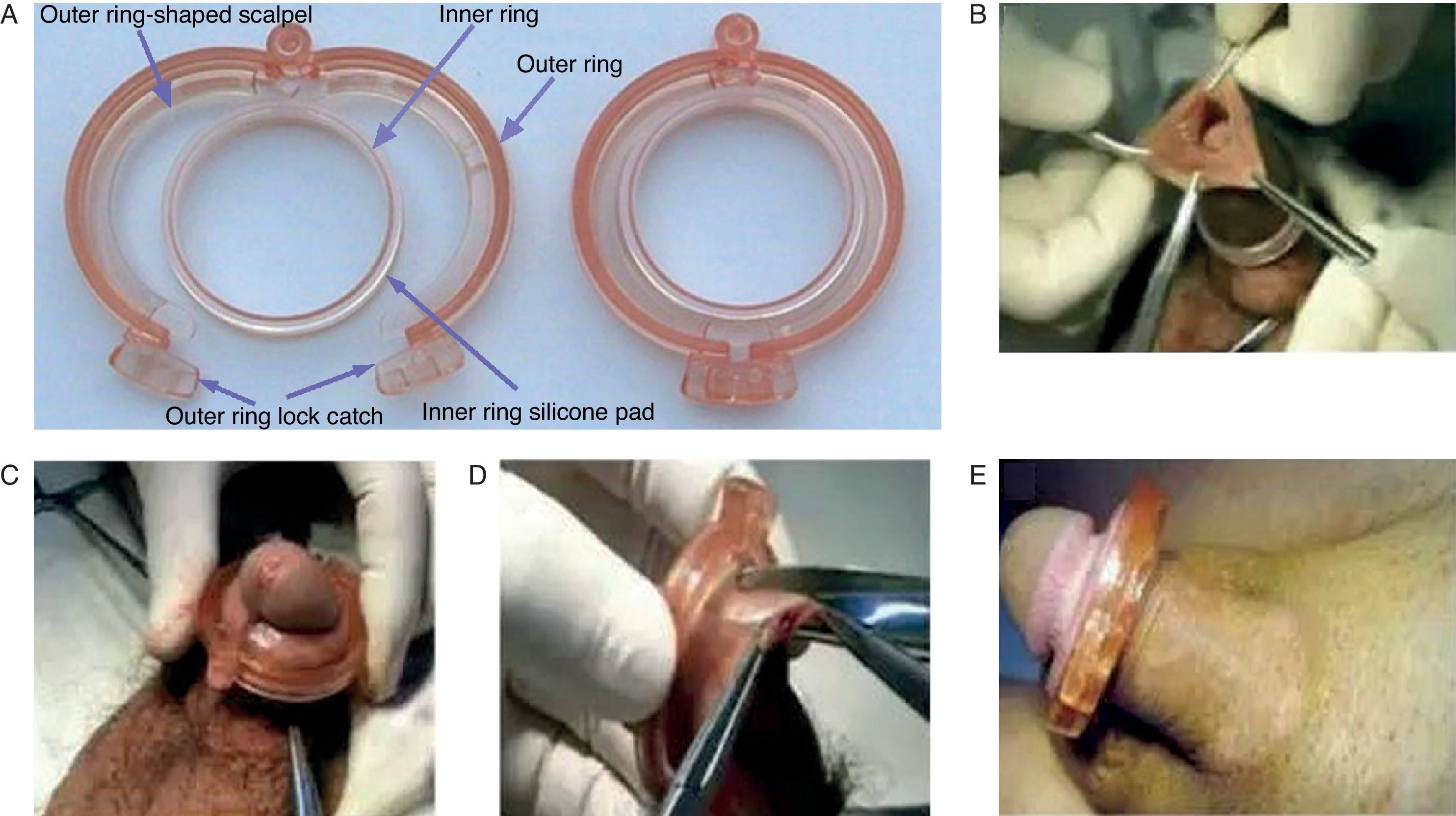
Materials and methodsThe devices and the proceduresThe SRC includes two rings, the inner ring as the supporting frame, and the outer one with two linked scalpels, which could lock itself and thus can make an anastomosis to that inner ring. The size of SRC, ranging from 13 to 40mm, was chosen according to the measurement of penis at the level of the coronal sulcus with a particular tape (Fig. 1A). The SRC was used first introduced by Peng31 in 2008. The inner ring was placed on foreskin which was over the glans. And thus, the edge of foreskin was clamped with the blood vessel forceps. After that, flipping over the ring, the coronal sulcus would be exposed. In addition, the device would be removed by the surgeon after 7 days (Fig. 1).
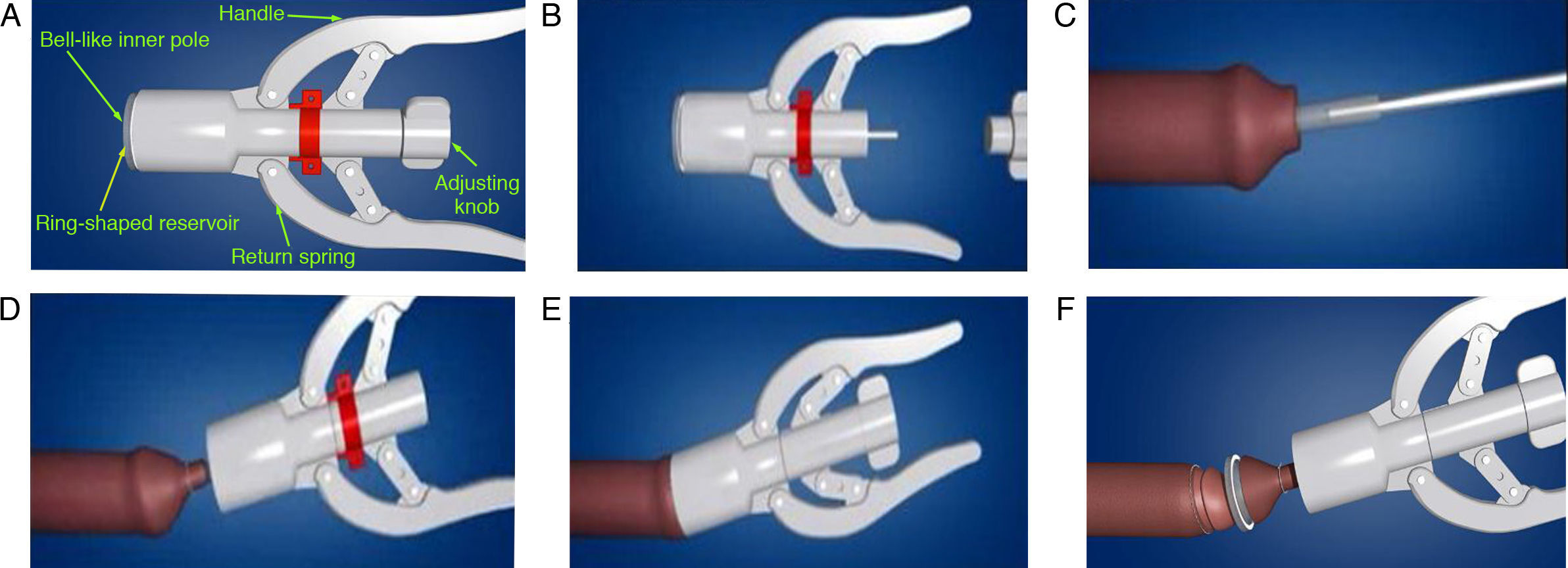
The DCSD consists of an inner rod and an outer pole, including the following items: (1) bell-like inner pole; (2) ring-stapled reservoir; (3) ring-stapled scalpel; (4) return spring; (5) handle; and (6) adjusting knob (Fig. 2A). A control handle is fixed on the outside of the outer pole and a connecting interface links with the inner rod from the inside. The disposable ring-shaped scalpel and staples are assembled in the outer pole. The DCSD was introduced by Wang et al.35 in 2014. Briefly, the inner rod was placed on glans penis and lifted the foreskin with vascular clamps. The outer pole was used to fix the foreskin, and then the knob was control to insert the proper position between the outer pole and inner rod, adjusted the control knobs and outer pole, the redundant foreskin was removed (Fig. 2).
Retrieval strategyThe systematic literature was preformed according to the guidelines for preferred reporting items for systematic reviews and meta-analyses.14 We searched the electronic databases including PubMed, Embase, Wan Fang database, VIP database, Chinese National Knowledge Infrastructure (CNKI) and China Biology Medicine (CBM) database from their inception to August 30, 2016, collecting the eligible studies of DCSD and SRC treating redundant prepuce or phimosis without language limitation. The keywords or MeSH search headings were used as followed: “redundant prepuce,” “excess foreskin,” “phimosis,” “disposable circumcision suture device,” “circumcision stapler,” “DCSD,” “novel device,” “Shang Ring,” “ring device,” “Shang huan,” “disposable anastomosis device,” and “SRC.” In addition, a manual retrieval from related reviews, meta-analyses and meeting reports was performed for references. The procedure generated disagreements which were defused through discussion with all researchers.
Selection criteriaStudies were eligible for inclusion if they met the following criteria: (a) RCTs or prospective studies; (b) the study included male patients with redundant prepuce or phimosis requiring circumcision; (c) studies involving treatments of DCSD and SRC; (d) full text available.
The following exclusion criteria were used: (a) summary, discuss theory, letters, case reports, comments, meta-analysis, review, and other types of research literature; (b) duplicate publications and data were unavailable to estimate RR or MD; (c) patients with genital malformations, urinary tract infection, coagulopathy, or diabetes.
Data extraction and quality assessmentThe following data were extracted and recorded in predesigned forms from the eligible studies by two reviewers (CG Huang and Y Dai) independently: the first author's name, publication year, study design, numbers of patients in each treatment group, ages of patients, the diagnostic criteria of patients, detail of interventions, follow-up period, and clinical outcome measurements. The outcomes included: (a) operation time; (b) intraoperative blood loss; (c) intraoperative pain score; (d) 24h postoperative pain score; (e) wound healing time; (f) rate of satisfaction with postoperative penile appearance; (g) treatment cost; (h) wound infection; (i) wound dehiscence; (j) wound edema; (k) postoperative bleeding and (l) adverse event rate.
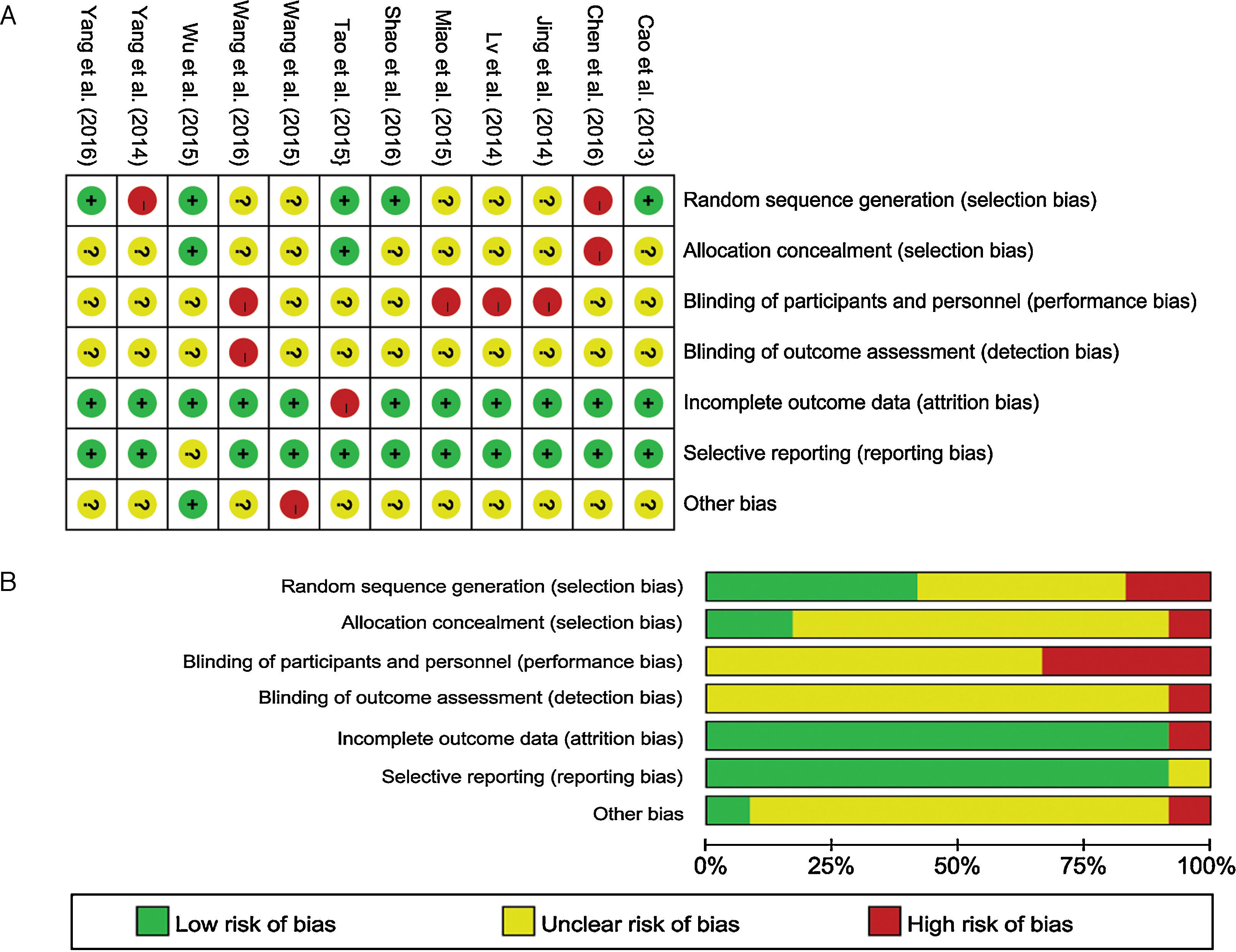
The assessment tool presented by Cochrane Handbook for Systematic Reviews Interventions version 5.1.015 was applied to evaluate the methodological quality of recruited clinical trials. For included trials, the following criteria were evaluated for risk of bias: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting and other bias. Any discrepancies were defused through discussion or the third reviewer.
Statistical analysis and meta-analysisAll statistical analyses were performed with Revman 5.3 provided by the Cochrane Collaboration and Stata statistical software (version 12.0, Stata Corporation, College Station, TX, USA). RR with 95% CI as the effect sizes were calculated for dichotomous outcomes (rate of satisfaction with penile appearance; wound infection; wound dehiscence; wound edema; adverse event rate), whereas statistical analysis of continuous outcomes (operation time; intraoperative blood loss; pain score; wound healing time; treatment cost; postoperative bleeding) was analyzed through MD and 95% CI. The Mantel–Haenszel Chi-square (χ2)16 based test for heterogeneity was performed using Cochran's Q-statistic and I2 statistic.17 The significant I2 valuing >50% was indicated existing heterogeneity, and the meta-analysis should be performed using the random effect model. On the contrary, heterogeneity (I2≤50%) was performing with no significance and the fixed effect model was implemented. When there was a high level of heterogeneity, the sensitivity analysis should be performed testing the reliability of the meta-analysis results. For these outcomes, the statistical significance should be tested using P<0.05.
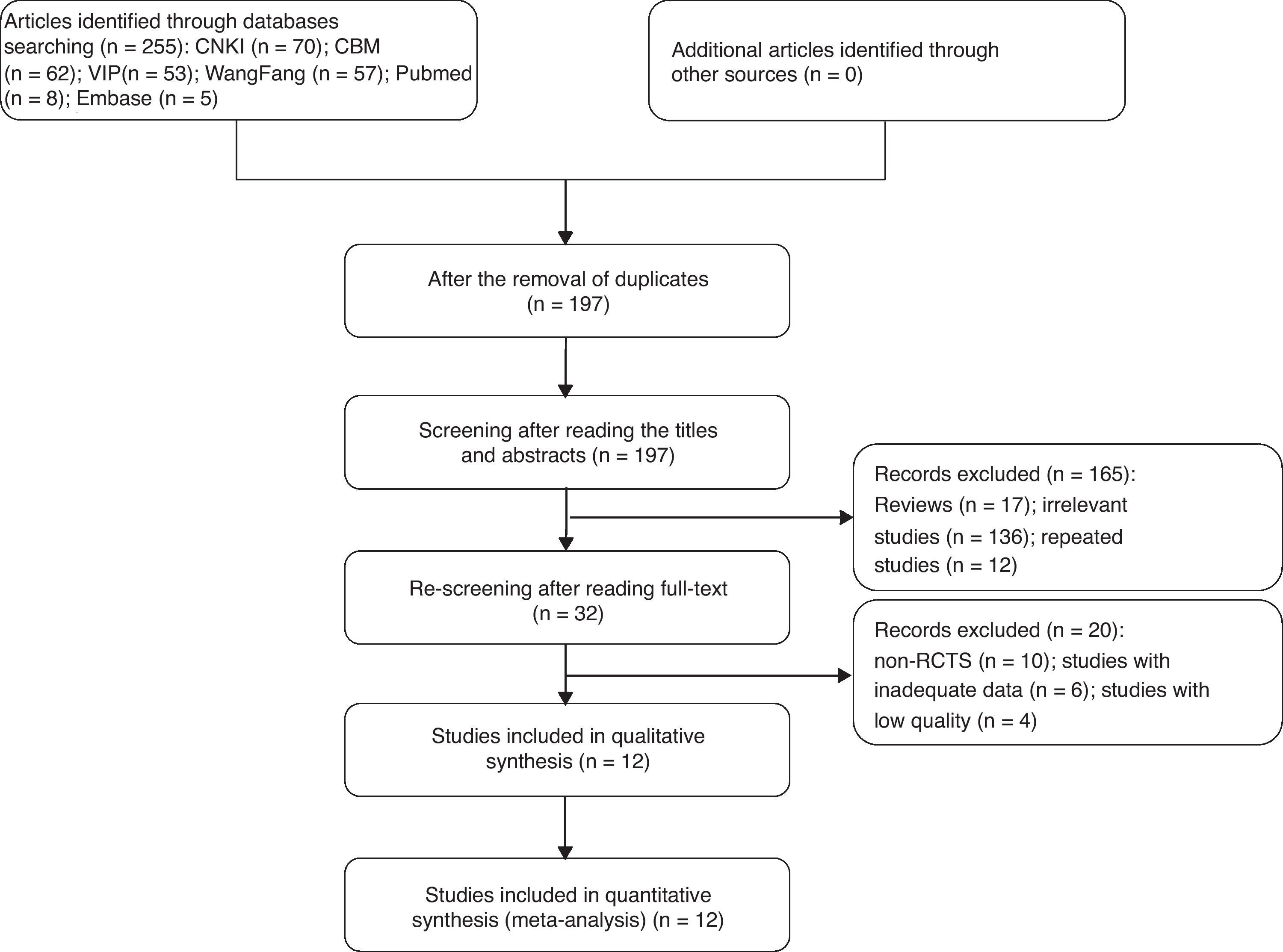
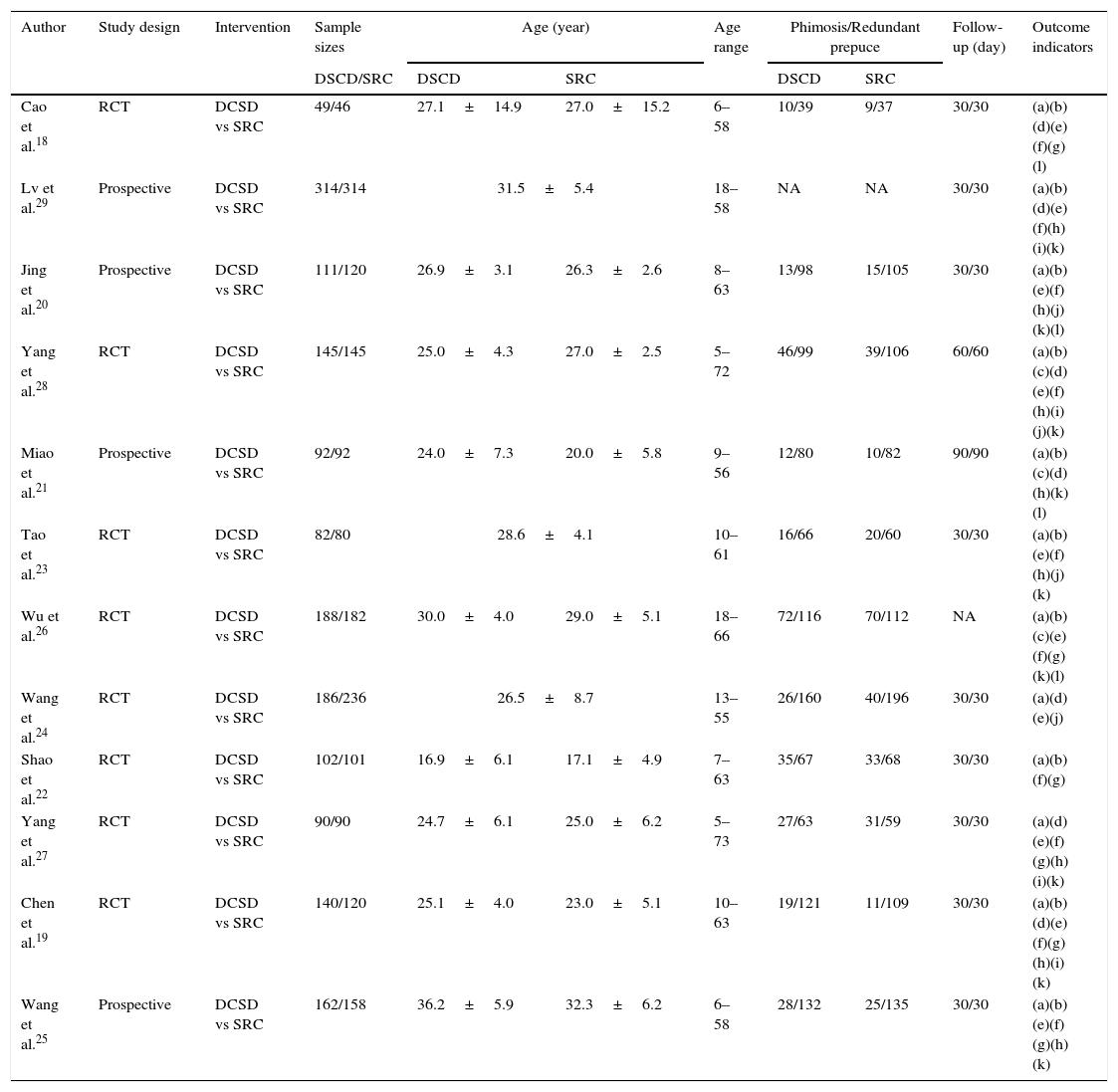
ResultsEligible studies and the risks of bias assessmentA totall of 255 studies were identified by searching through the databases and no additional records were identified through other sources. After screening the duplicates, titles, abstracts and full-text, we removed irrelevant and repeated studies, and there were 32 records appeared potentially relevant. We searched the reference lists of all the identified studies in order to include as many relevant articles as possible. And a total of 12 studies18–29 were eligible and included in the meta-analysis.
A flow chart of records of acquisition was illustrated in Fig. 3. Eight of the reports18,19,22–24,26–28 were RCTs and the other 4 reports20,21,25,29 were prospective studies, with a total of 1661 participants in the DCSD group and 1684 participants in the SRC group. Baseline characteristics of the 12 studies were conducted in Table 1.
General characteristics of the 12 eligible trials involved.
| Author | Study design | Intervention | Sample sizes | Age (year) | Age range | Phimosis/Redundant prepuce | Follow-up (day) | Outcome indicators | ||
|---|---|---|---|---|---|---|---|---|---|---|
| DSCD/SRC | DSCD | SRC | DSCD | SRC | ||||||
| Cao et al.18 | RCT | DCSD vs SRC | 49/46 | 27.1±14.9 | 27.0±15.2 | 6–58 | 10/39 | 9/37 | 30/30 | (a)(b)(d)(e)(f)(g)(l) |
| Lv et al.29 | Prospective | DCSD vs SRC | 314/314 | 31.5±5.4 | 18–58 | NA | NA | 30/30 | (a)(b)(d)(e)(f)(h)(i)(k) | |
| Jing et al.20 | Prospective | DCSD vs SRC | 111/120 | 26.9±3.1 | 26.3±2.6 | 8–63 | 13/98 | 15/105 | 30/30 | (a)(b)(e)(f)(h)(j)(k)(l) |
| Yang et al.28 | RCT | DCSD vs SRC | 145/145 | 25.0±4.3 | 27.0±2.5 | 5–72 | 46/99 | 39/106 | 60/60 | (a)(b)(c)(d)(e)(f)(h)(i)(j)(k) |
| Miao et al.21 | Prospective | DCSD vs SRC | 92/92 | 24.0±7.3 | 20.0±5.8 | 9–56 | 12/80 | 10/82 | 90/90 | (a)(b)(c)(d)(h)(k)(l) |
| Tao et al.23 | RCT | DCSD vs SRC | 82/80 | 28.6±4.1 | 10–61 | 16/66 | 20/60 | 30/30 | (a)(b)(e)(f)(h)(j)(k) | |
| Wu et al.26 | RCT | DCSD vs SRC | 188/182 | 30.0±4.0 | 29.0±5.1 | 18–66 | 72/116 | 70/112 | NA | (a)(b)(c)(e)(f)(g)(k)(l) |
| Wang et al.24 | RCT | DCSD vs SRC | 186/236 | 26.5±8.7 | 13–55 | 26/160 | 40/196 | 30/30 | (a)(d)(e)(j) | |
| Shao et al.22 | RCT | DCSD vs SRC | 102/101 | 16.9±6.1 | 17.1±4.9 | 7–63 | 35/67 | 33/68 | 30/30 | (a)(b)(f)(g) |
| Yang et al.27 | RCT | DCSD vs SRC | 90/90 | 24.7±6.1 | 25.0±6.2 | 5–73 | 27/63 | 31/59 | 30/30 | (a)(d)(e)(f)(g)(h)(i)(k) |
| Chen et al.19 | RCT | DCSD vs SRC | 140/120 | 25.1±4.0 | 23.0±5.1 | 10–63 | 19/121 | 11/109 | 30/30 | (a)(b)(d)(e)(f)(g)(h)(i)(k) |
| Wang et al.25 | Prospective | DCSD vs SRC | 162/158 | 36.2±5.9 | 32.3±6.2 | 6–58 | 28/132 | 25/135 | 30/30 | (a)(b)(e)(f)(g)(h)(k) |
RCT: randomized controlled trial; DCSD: disposable circumcision suture device; SRC: Shang ring circumcision; NA: not available; (a) operation time; (b) intraoperative blood loss; (c) intraoperative pain score; (d) 24h postoperative pain score; (e) wound healing time; (f) rate of satisfaction with postoperative penile appearance; (g) treatment cost; (h) wound infection; (i) wound dehiscence; (j) wound edema; (k) postoperative bleeding; (l) adverse event rate.
In regards to quality assessment, five of the eligible studies have described random sequence generation, there are only two articles reported the allocation concealment. Moreover, none of the researches applied blinding methods, most of the trials had completed data, and only one research reported didn’t have other bias. Two studies did not adopt a randomized groupings or grouped with improper methods. Most of the included trials did not specifically describe allocation concealment and blinding, and four of these trials illustrated unblind or open-lable. One studies had other bias. The assessment for bias risk was summarized quantified or qualitatively in Fig. 4.
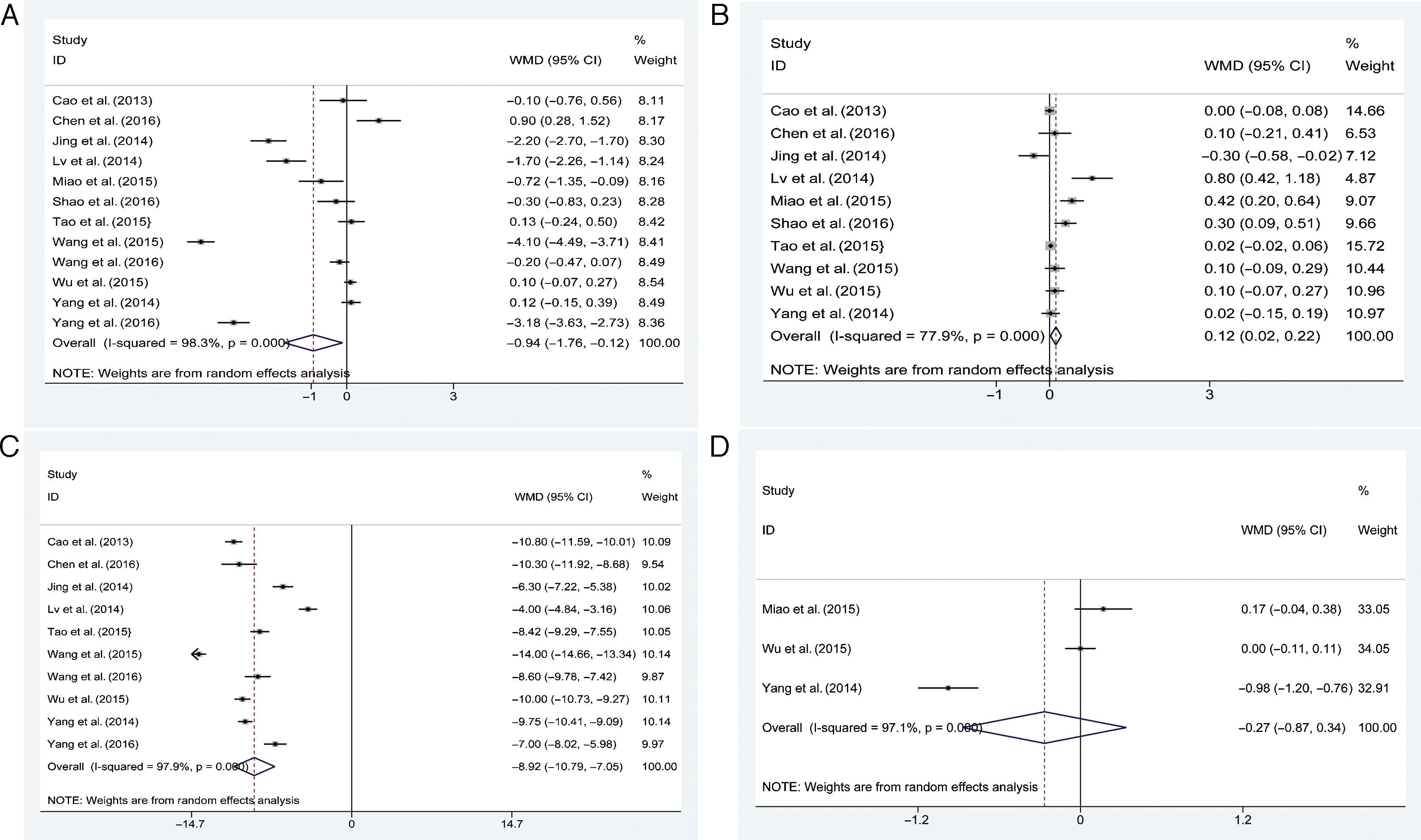
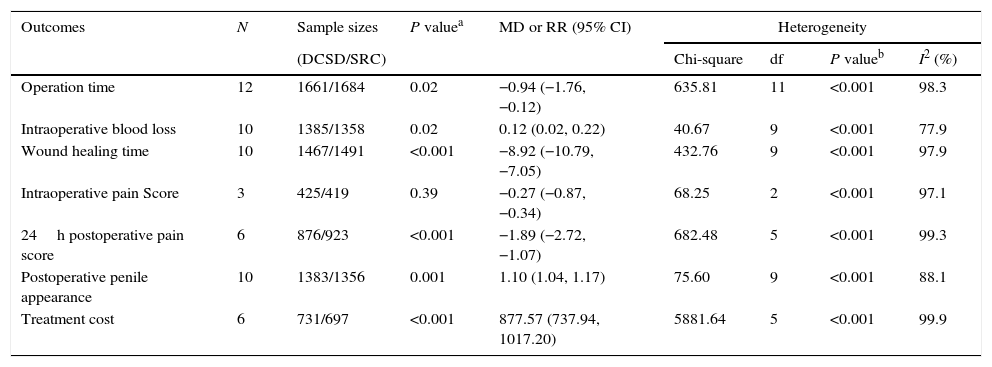
Meta-analysis of the operation timeAll the 12 studies18–29 were included in the meta-analysis of the operation time, with a total of 1661 patients received DCSD group and 1684 patients received SRC group. The random effects model was selected due to the high level of heterogeneity (P<0.001, I2=98.3%). The pooled estimates demonstrated that the operation time in DCSD group was statistically significant shorter than that in the SRC group [MD=−0.94, 95%CI (−1.76, −0.12), P=0.02; Fig. 5A]
Meta-analysis of the intraoperative blood lossIn total of 10 studies18–23,25,26,28,29 were analyzed for the intraoperative blood loss, with 1385 patients in the DCSD treatment and 1358 patients in the SRC treatment. There was the significant heterogeneity (P<0.001, I2=77.9%) existing in the recruited studies and the random effects model was applied. The pooled estimates revealed that DCSD group has the statistically more intraoperative blood loss compared with the SRC group [MD=0.12, 95%CI (0.02, 0.22), P=0.02; Fig. 5B] (Table 2).
The results list of meta-analysis forest plots.
| Outcomes | N | Sample sizes | P valuea | MD or RR (95% CI) | Heterogeneity | |||
|---|---|---|---|---|---|---|---|---|
| (DCSD/SRC) | Chi-square | df | P valueb | I2 (%) | ||||
| Operation time | 12 | 1661/1684 | 0.02 | −0.94 (−1.76, −0.12) | 635.81 | 11 | <0.001 | 98.3 |
| Intraoperative blood loss | 10 | 1385/1358 | 0.02 | 0.12 (0.02, 0.22) | 40.67 | 9 | <0.001 | 77.9 |
| Wound healing time | 10 | 1467/1491 | <0.001 | −8.92 (−10.79, −7.05) | 432.76 | 9 | <0.001 | 97.9 |
| Intraoperative pain Score | 3 | 425/419 | 0.39 | −0.27 (−0.87, −0.34) | 68.25 | 2 | <0.001 | 97.1 |
| 24h postoperative pain score | 6 | 876/923 | <0.001 | −1.89 (−2.72, −1.07) | 682.48 | 5 | <0.001 | 99.3 |
| Postoperative penile appearance | 10 | 1383/1356 | 0.001 | 1.10 (1.04, 1.17) | 75.60 | 9 | <0.001 | 88.1 |
| Treatment cost | 6 | 731/697 | <0.001 | 877.57 (737.94, 1017.20) | 5881.64 | 5 | <0.001 | 99.9 |
N: number of studies; DCSD: disposable circumcision suture device; SRC: Shang ring circumcision; MD: mean difference; RR: risk ratio; CI: confidence interval; df: degree of freedom.
There were 10 literatures18–20,23–29 recruited of 1467 patients in the DCSD treatment and 1491 patients in the SRC treatment. Heterogeneity was indicated (P<0.001, I2=97.9%) and the random effects model was applied to evaluate the pooled estimates. The results merged estimates demonstrated that the patients in the DCSD group reported a markedly shorter wound healing time than SRC group [MD=−8.92, 95%CI (−10.79, −7.05), P<0.001; Fig. 5C].
Meta-analysis of the pain scoreThe intraoperative pain score and 24h postoperative pain score had enough data relevant to two therapeutic measures and thus were included in the meta-analysis. There were only 3 literatures21,26,28 recruited for intraoperative pain score with 425 patients in the DCSD treatment and 419 patients in the SRC treatment. The results indicated the significant heterogeneity (P<0.001, I2=97.1%) was existed between the trials, thus we used the random effects model to evaluate the pooled analysis. The pooled estimates indicated that there was no significant difference in the intraoperative pain score between the DCSD and SRC group [MD=−0.27, 95%CI (−0.87, −0.34), P=0.39; Fig. 5D].
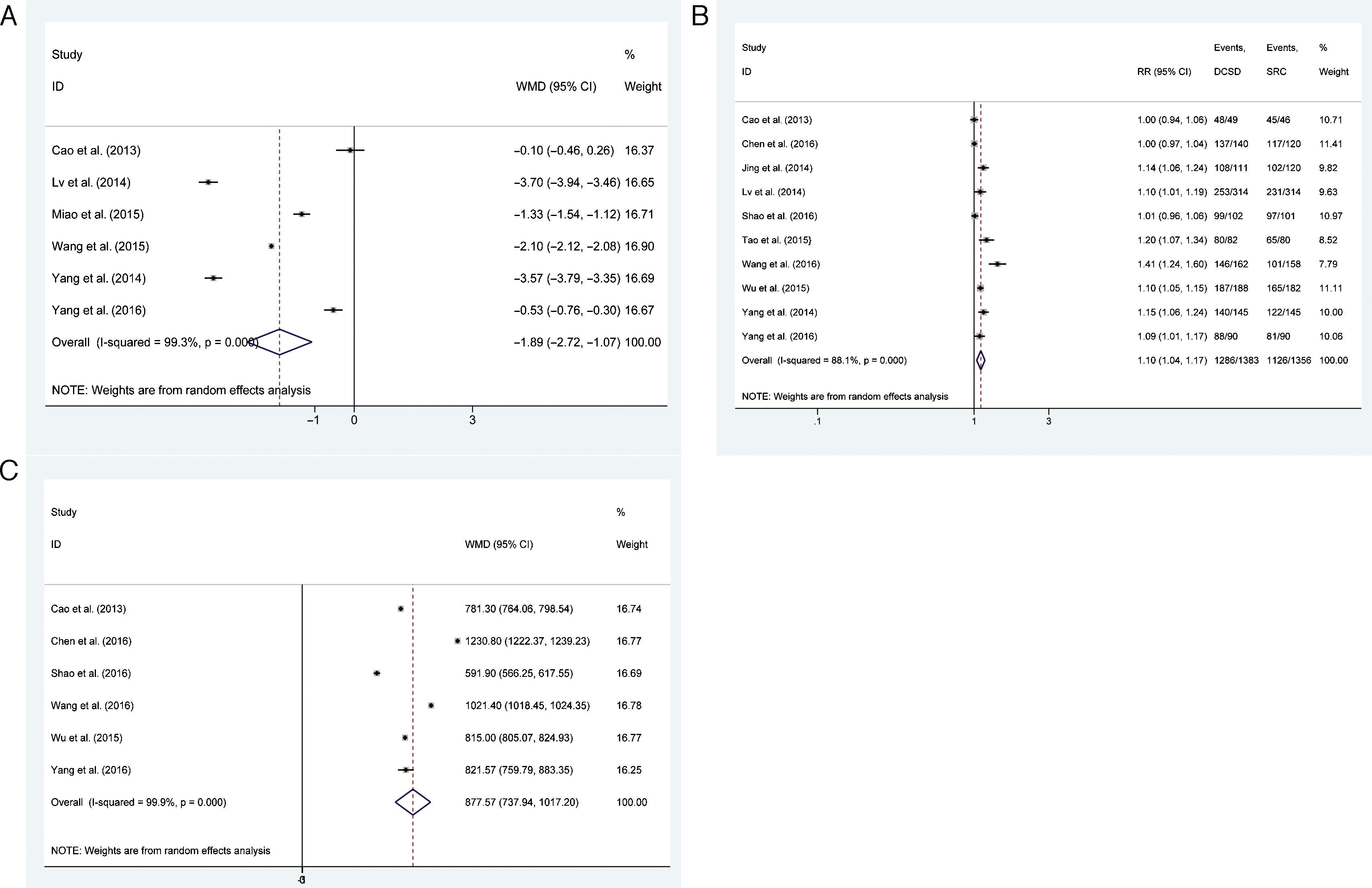
The 24h postoperative pain score was reported in six included studies18,21,24,27–29 with 876 patients in the DCSD group and 923 patients in the SRC group. The random effects model was chosen for the meta-analysis as the significant heterogeneity was existing (P<0.001, I2=99.3%). The total estimates demonstrated that 24h postoperative pain score in DCSD group was lower than SRC group significantly [MD=−1.89, 95%CI (−2.72, −1.07), P<0.001; Fig. 6A].
Meta-analysis of the satisfaction for postoperative penile appearanceThere were a total of 10 literatures18–20,22,23,25–29 studied the participants’ satisfaction for penile appearance after treatment with 1383 patients in DCSD group and 1356 patients in SRC group. The heterogeneity result indicated significant heterogeneity was existed between the trials (P<0.001, I2=88.1%). The random effects model was chosen in this analysis. The pooled estimates described that participants’ satisfaction in DCSD group was significantly higher than SRC group [RR=1.10, 95%CI (1.04, 1.17), P=0.001; Fig. 6B].
Meta-analysis of the treatment costThe treatment cost was recorded in 6 literatures18,19,21,25–27 with 731 patients in DCSD group and 697 patients in SRC group. The results shown significant heterogeneity (P<0.001, I2=99.9%) was existed, thus the random effects model was chosen to evaluate the pooled analysis. The results demonstrated that DCSD had a statistically higher treatment cost compared with SRC [MD=0.88, 95%CI (0.74, 1.02), P<0.001; Fig. 6C].
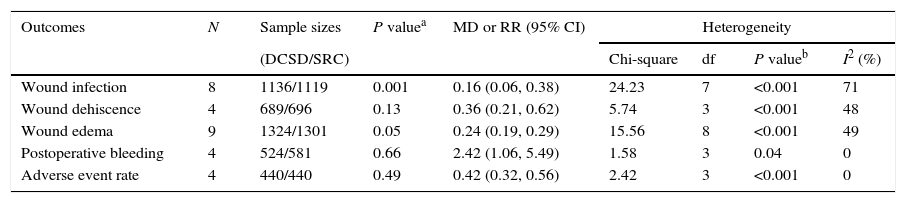
Meta-analysis of the postoperative complicationsThere were 8 literatures19–21,23,25,27–29 studied the rate of wound infection and the pooled estimates indicated that DCSD treatment with wound infection was observed less significantly than SRC treatment [RR=0.16, 95%CI (0.06, 0.38), P<0.001; I2=71%; Table 3]. Four studies19,27–29 reported on wound dehiscence found that the rate of wound dehiscence was lower statistically in the DCSD group than in the SRC group [RR=0.36, 95%CI (0.21,0.62), P<0.001; I2=48%; Table 3]. Nine studies19–21,23,25–29 reported on wound edema showed that the rate of wound edema was lower dramatically in the DCSD group than in the SRC group [RR=0.24, 95%CI (0.19, 0.29), P<0.001; I2=49%; Table 3]. The results of postoperative bleeding studied in 4 literatures20,23,24 showed that The DCSD group had significantly less postoperative bleeding than SRC group [MD=2.42, 95%CI (1.06, 5.49), P=0.04; I2=0%; Table 3]. A lower adverse events rate reported by 4 studies18,20,21,26 was indicated in the DCSD group compared with the SRC group [RR=0.42, 95%CI (0.32, 0.56), P<0.001; I2=0%; Table 3].
The indices for evaluating the postoperative complications.
| Outcomes | N | Sample sizes | P valuea | MD or RR (95% CI) | Heterogeneity | |||
|---|---|---|---|---|---|---|---|---|
| (DCSD/SRC) | Chi-square | df | P valueb | I2 (%) | ||||
| Wound infection | 8 | 1136/1119 | 0.001 | 0.16 (0.06, 0.38) | 24.23 | 7 | <0.001 | 71 |
| Wound dehiscence | 4 | 689/696 | 0.13 | 0.36 (0.21, 0.62) | 5.74 | 3 | <0.001 | 48 |
| Wound edema | 9 | 1324/1301 | 0.05 | 0.24 (0.19, 0.29) | 15.56 | 8 | <0.001 | 49 |
| Postoperative bleeding | 4 | 524/581 | 0.66 | 2.42 (1.06, 5.49) | 1.58 | 3 | 0.04 | 0 |
| Adverse event rate | 4 | 440/440 | 0.49 | 0.42 (0.32, 0.56) | 2.42 | 3 | <0.001 | 0 |
N: number of studies; DCSD: disposable circumcision suture device; SRC: Shang ring circumcision;; MD: mean difference; RR: risk ratio; CI: confidence interval; df: degree of freedom.
Male circumcision is one of the oldest and most commonly performed surgical procedures in the world.1 The earliest record of circumcision stems from Egypt, the image of the procedures of adult circumcision engraved in Ankh-Mahor's tomb at Saqqara, dating back to about 2400–2300 BCE.2 With surgical techniques developing, male practices have been more and more mature.
At present, conventional circumcision (CC) and two novel types of disposable circumcision devices (SRC and DCSD) were suggested to be the most effective surgeries for redundant prepuce or phimosis. Comparing with the novel types, the CC procedures have the disadvantage of longer operation time, inevitably suturing the incision, more adverse complications, and stitch removal pain. SRC was invented by Mr. Shang JZ from China, the principle of SRC was applied by clamping the superficial dorsal veins and vessels between an inner and outer ring-shaped scalpel to the transection of the foreskin, and then allowing foreskin to be removed by natural atrophy or surgically.30,31 By imitating intestinal anastomosis, DCSD was used through cutting the foreskin with annular circumcision, and simultaneously suturing wounds with suture staples.29,32,33 Clinical date demonstrate SRC has advantages over conventional technology due to lower complications rate, shorter operation time, and high satisfaction rate12,31; however, it cause higher postoperative pain scores, secretions around the anastomat, postoperative edema, prolonged ring split time and wound healing time after rings removed.18,24,30 DCSD can make inner and outer plates fit well, is a more effective and safer novel disposable device for patients than CC.29,32 In order to provide evidences for choosing which method is better for patients, we applied this meta-analysis to evaluate the efficacy of DCSD and SRC in treating redundant prepuce or phimosis comprehensively. Eventually, 12 high-quality studies18–29 met the inclusion criteria. To our knowledge, this is the first meta-analysis to compare DCSD with SRC for MC in English.
All included studies had described the operation time, and the pooled analysis indicated that the operation time of DCSD treatment was shorter than SRC treatment, which may be due to the difference of the procedures.
Our pooled analysis demonstrated that DCSD had the disadvantages in control of bleeding. As there was no electric coagulation hemostasis during the operation of DCSD treatment and having a gap between the suture staples and nails, which means there would be the blood loss in the procedures,20,24,25 if necessary, we should sew the ecstatic blood vessels up to prevent it. Conversely, the outer ring in SRC treatment is carried out and clamped shut the foreskin, covering the inner ring before the foreskin is excised and thus hindering blood flow, so that the intraoperative blood loss is reduced.
Our findings in this meta-analysis demonstrated that the wound healing time of the DCSD group was markedly shorter than SRC group. To DCSD treatment, the foreskin was cut with the suture in the same moment. By contrast, the use of SRC treatment had required no sutures, so that the rings would be manually removed several days after surgery, prolonging the time of wound healing. A non-RCT reported by Ma et al.34 showed that wound healing time for DCSD was12.4±3.1 days, compared with18.4±2.7 days for SRC. Our meta-analysis is consistent with the finding.
The intraoperative pain score and 24h postoperative pain score were included in the meta-analysis with enough data relevant to two therapeutic measures. Our findings indicated that there was no statistically difference in the intraoperative pain score between the DCSD group and the SRC group, which may be due to the recruited studies too less in our meta-analysis to evaluate intraoperative pain score. The results of meta-analysis showed that 24h postoperative pain score in DCSD group was lower than SRC group. Cao et al.18 pointed out that the leading reason for a lower 24h postoperative pain score was that SRC treatment had not require the suture, removing the rings with the obvious pain for the participants and even need to use paregorics or local anesthetics during the removing operation; by contrast, the operation of DCSD treatment was cutting with the suture, so that presenting an opportunity for decreasing the pain score. Our analysis was in accordance with the other included studies.
We performed the meta-analysis of the satisfaction for postoperative penile appearance indicated that satisfaction rate of DCSD group was 93%, compared with 83% for SRC. The results may be as follows: (1) DCSD treatment was more safe and effective with suturing than SRC treatment; and (2) DCSD treatment have shorter wound healing time and a lower pain score, comparison of SRC treatment. In respects to the treatment cost, subjects in DCSD treatment were more expensive than SCR treatment.20,23–25
There were wound infection, dehiscence, edema, bleeding, and adverse events rate included in the meta-analysis of postoperative complications between DCSD and SRC. The pooled results showed a significantly lower the rate of wound infection, dehiscence and wound edema with DCSD relative to SRC, which may be due to the patients choosing SRC with waiting for spontaneous ring-removal, who would wear the device for 2–3 weeks after the operation, increasing the risk of local complication rate. Conversely, there was not any difference reached statistical significance in postoperative bleeding. Meanwhile, an obvious drawback of the SRC is markedly higher incidence of edema than DCSD. These may be the results the following factors29,30,32: (1) the SRC procedure couldn’t help the reconstruction of lymphatic vessels and blood vessels in time; (2) there was a relatively narrow gap between the inner ring and the corona, increasing the risk of infection, whereas that infection could aggravate the edema; (3) the inflammation reaction and repeated erection of the penis also could aggravate the edema after procedure. Our present meta-analysis proves the above results.
Nevertheless, our meta-analysis does have certain limitations. Firstly, the sample size of certified eligible studies is small; whether the eligible studies excepted Cao et al.18 applied the blind method and allocation concealment are unknown; and some eligible studies’ characteristics are also unclear. Secondly, the difference of the number of participants among eligible trials was relatively large; and follow-up time of eligible studies differs, which would impact the results. Thirdly, inevitably different judgment standards in study indexes have increased the heterogeneity; and the eligible trials were all from China, which also would enhance the heterogeneity. In addition, we have applied the sensitivity analysis individually to test the reliability of our meta-analysis outcomes and the analysis indicated our meta-analysis conclusion is stable.
ConclusionOur meta-analysis found that the DCSD treatment has the advantages of shorter operation time, lower pain scores, no stitch removal pain, better postoperative penile appearance, fewer complications and shorter wound healing time relative to SRC treatment. Therefore, DCSD as the novel disposable device might be the more efficacious and safer choice for patients. However, our findings need additional and high-quality studies to validate in the future.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors declare no conflict of interest.
Ethical responsibilitiesNone.