Persistent scrotal pain after varicocelectomy is stressful for both surgeon and patient. The number of researches focusing on which patient will benefit more from the operation is increasing in the literature. In this prospective study, we aimed to investigate whether the patient's physical activity levels and occupations affect the success of varicocelectomy in terms of pain relief.
Materials and methodsThe data of 176 patients who underwent subinguinal microscopic varicocelectomy were analyzed according to BMI, age, varicocele grade, laterality, duration of pain, testicular volume difference, quality of pain, level of physical activity, and profession. The International Physical Activity Questionnaire was used to evaluate the level of physical activity. Patients were grouped as inactive, moderately active, and active according to this scale. Visual analog scale (VAS) scores of the patients were recorded before and after the procedure.
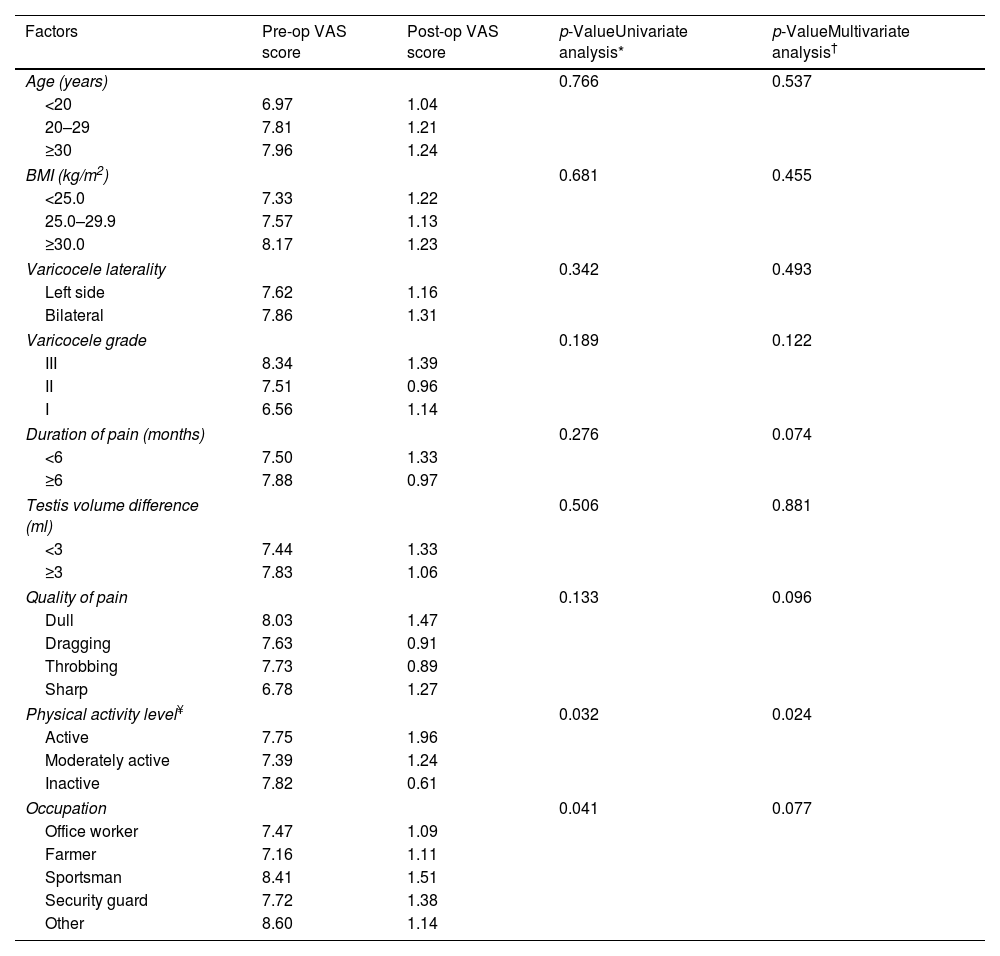
Results135 patients (76.7%) reported complete resolution of their pain. Partial resolution of pain was observed in 34 patients (19.3%). Seven patients (4%) complained of the same pain level. Univariate analysis showed that patient occupations and physical activity levels significantly affected the pain level (p=0.041, p=0.032, respectively). In the multivariate analysis, only physical activity levels of the patients were statistically significant in predicting the resolution of pain (p=0.024).
ConclusionsPatients with low physical activity levels who underwent microscopic varicocelectomy surgery are less likely to have postoperative pain.
El dolor escrotal persistente después de la varicocelectomía es una situación estresante tanto para el cirujano como para el paciente. En este estudio prospectivo, nuestro objetivo fue investigar si los niveles de actividad física y las ocupaciones del paciente afectan el éxito de la varicocelectomía en términos de alivio del dolor.
Materiales y métodosSe analizaron los datos de 176 pacientes que se sometieron a varicocelectomía microscópica subinguinal según IMC, edad, grado de varicocele, lateralidad, duración del dolor, diferencia de volumen testicular, calidad del dolor, nivel de actividad física y profesión. Se utilizó el Cuestionario Internacional de Actividad Física para evaluar el nivel de actividad física. Los pacientes se agruparon en inactivos, moderadamente activos y activos según esta escala. Las puntuaciones de la escala visual analógica visual de los pacientes se registraron antes y después del procedimiento.
ResultadosCiento treinta y cinco pacientes (76,7%) informaron resolución completa de su dolor. Se observó resolución parcial del dolor en 34 pacientes (19,3%). Siete pacientes (4%) todavía se quejaban del mismo nivel de dolor. El análisis univariado mostró que las ocupaciones de los pacientes y los niveles de actividad física afectaron significativamente el nivel de dolor (p=0,041; p=0,032, respectivamente). En el análisis multivariado, solo los niveles de actividad física de los pacientes fueron estadísticamente significativos para predecir la resolución del dolor (p=0,024).
ConclusionesLos pacientes con bajo nivel de actividad física que serán operados de varicocelectomía microscópica tienen menor probabilidad de presentar dolor postoperatorio.
Varicocele is the unusual enlargement of the pampiniform plexus and testicular veins. Varicocele can cause persistent scrotal pain, testicular hypotrophy, impaired spermatogenesis, and infertility. Chronic scrotal pain is detected in 10% of varicocele patients.1 The mechanism of varicocele-related pain has not been fully explained. In the case of scrotal pain, differential diagnoses should be excluded. Varicocele patients with scrotal pain should be treated conservatively on the first attempt. Varicocelectomy may be offered as an alternative treatment method when conservative management fails.2
The symptom relief rate of varicocelectomy has been reported in the range of 48% and 90%.2–6 The choice of treatment is a dilemma for the surgeon because of the variability of these success rates. In order to guide urologists’ decision-making process, specific parameters that may be effective in the operation's success have been investigated. Age, body mass index (BMI), surgical technique, duration of pain, character of pain, and varicocele grade were evaluated in the previous studies.7–10 In our clinical observation, we think the pain may be related to the patient's physical activity level. We aimed to investigate whether the patient's physical activity levels and occupations affect the success of varicocelectomy in terms of pain relief. To the best of our knowledge, this is the first study using a validated questionnaire to determine physical activity (Fig. 1).
Materials and methodsPatients with chronic scrotal pain (with or without infertility) who applied to the urology clinic between May 2021 and May 2022 were evaluated prospectively. The study protocol was approved by the Ethics Committee. All steps of the study were completed in accordance with the Declaration of Helsinki.
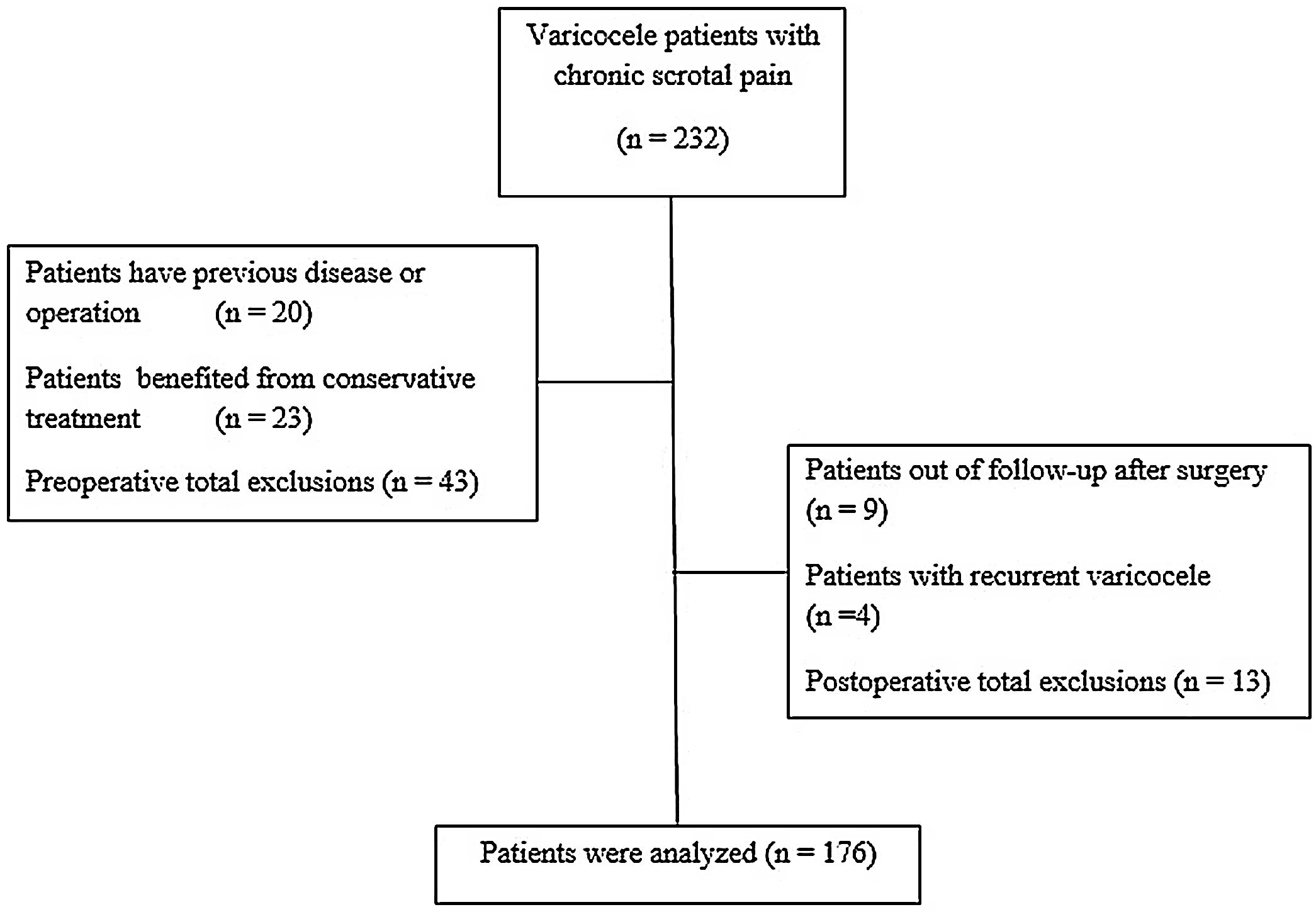
A total of 232 patients diagnosed with varicocele were investigated. All patients were confirmed to have varicocele as a result of doppler ultrasonography. Twenty patients with a previous history of sexually transmitted disease, stone disease, male accessory gland infection, epididymitis, orchitis, acute or chronic prostatitis, spermatocele, hydrocele, scrotal surgery, trauma, inguinal hernia, and testicular torsion were excluded. All patients were treated with conservative management for an average of 4 weeks in the preoperative period. Restricting physical activities, scrotal elevation, and non-steroidal anti-inflammatory drugs were recommended as conservative treatment.7 Twenty-three patients who benefited from the treatment were excluded.
Varicocele localization, varicocele grade, duration of pain, quality of pain, BMI, testicular hypotrophy, and physical activity status of all patients were recorded. Visual analog scale (VAS) scores were recorded before the procedure. Varicocele grade was evaluated as; Grade I palpable only with the Valsalva maneuver, Grade II easily palpable but not visible, and Grade III easily visible.11 Testicular volume was calculated by ultrasonographic measurement (Fig. 2).
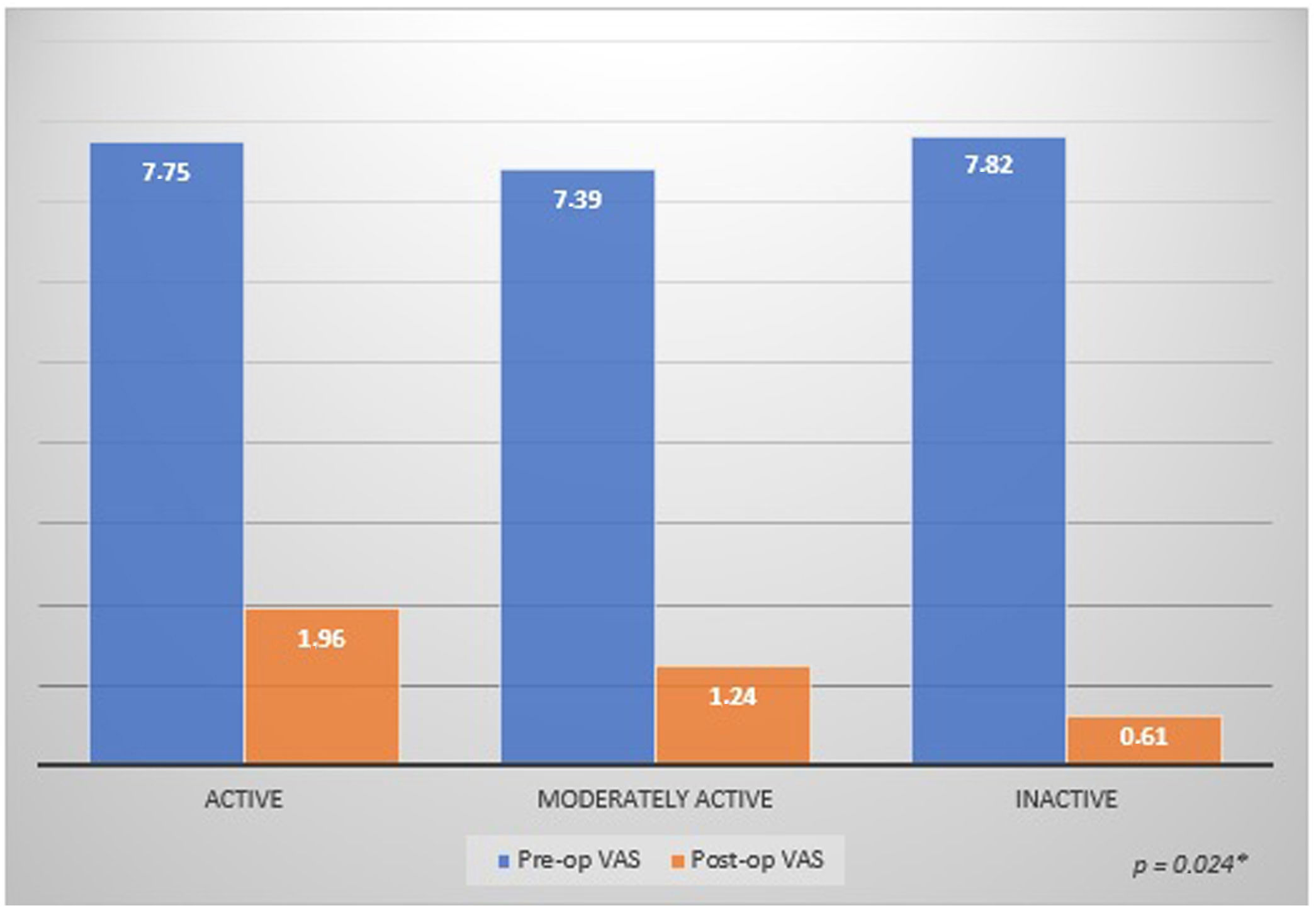
VAS (visual analogue scale) scores based on physical activity level†.
*Multivariate linear regression analysis.
†International Physical Activity Questionnaire. Craig et al.12
Subinguinal microscopic varicocelectomy was performed in both centers by two experienced surgeons. The postoperative 3rd-month examination of the patients was carried out by two different urologists for a more objective evaluation. The patients’ pain status and VAS scores were re-evaluated in the postoperative 3rd month. Patients with unresolved pain were re-examined to exclude differential diagnoses. Doppler ultrasound was used to demonstrate recurrent varicocele. Preoperative and postoperative VAS scores of the patients were recorded according to BMI, age, varicocele grade, laterality, duration of pain, testicular volume difference, quality of pain, level of physical activity, and occupation.
The “International Physical Activity Questionnaire” (IPAQ) was used to evaluate the level of physical activity. This questionnaire was developed by the International Consensus Group and created with the support of the World Health Organization and the Center for Disease Control. The validity and reliability study of the IPAQ scale was conducted by Craig et al. in 12 countries.12 In 2010, this scale was adapted to Turkish by Saglam et al., and its validity and reliability study was conducted.13 The metabolic equivalent threshold (MET) score on this scale is obtained by calculating the sedentary, low, moderate, and intense activity times in a day. Patients are evaluated in 3 categories according to their physical activity levels as inactive, moderately active, and active.
Statistical analysisThe Statistical Package for the Social Sciences version 20 (SPSS IBM Corp.; Armonk, NY) program was used for statistical analysis. Data were evaluated by univariate analysis of the general linear model and multivariate linear regression analysis. Data were analyzed at a 95% confidence interval (CI), considered significant when p value was <0.05. A normal distribution of the quantitative data was checked using the Kolmogorov–Smirnov test.
ResultsThere were no complications during the operation. Postoperative complications consisted of one hydrocele and one hematoma. No patient required additional surgery. There was no patient with testicular atrophy. A total of 13 patients, including nine out of follow-up after surgery and four patients with recurrent varicocele, were excluded from the study. Doppler ultrasound was used to demonstrate recurrent varicocele.
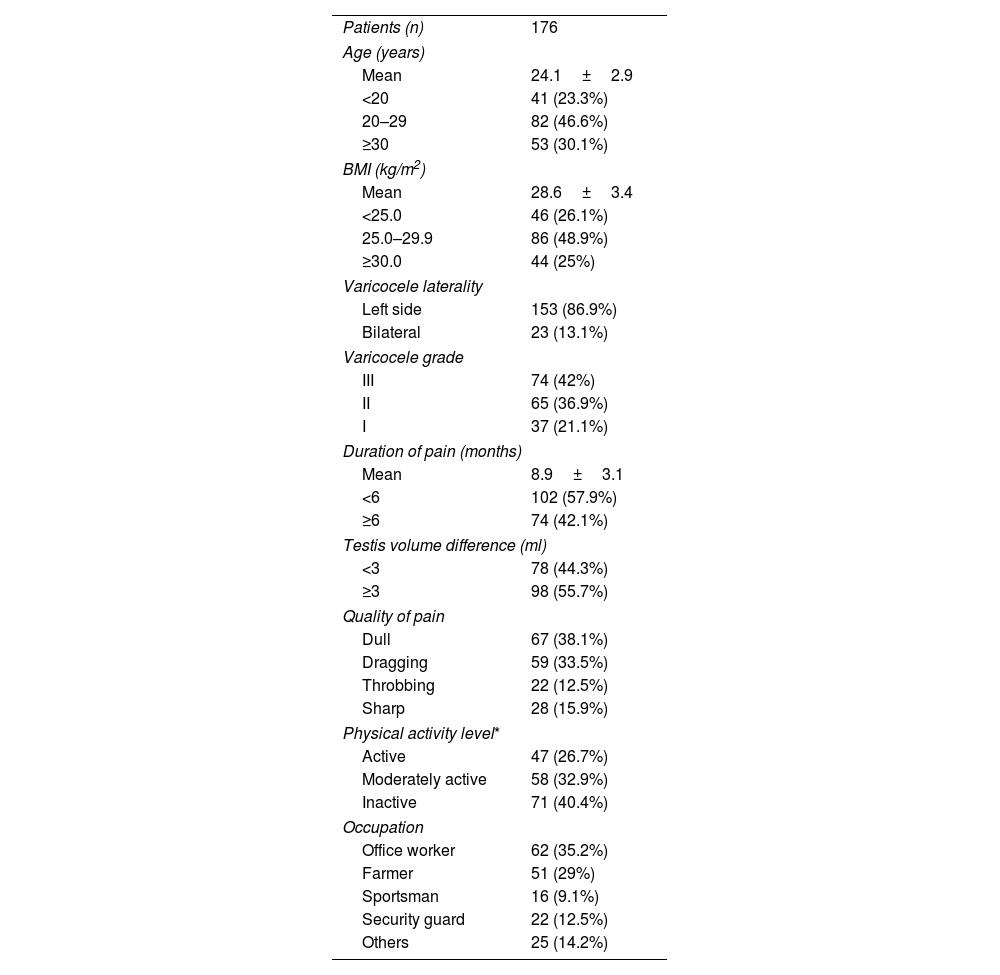
Data from 176 patients were analyzed. The mean age was 24.1±2.9 (range, 16– 44) years. The mean BMI was 28.6±3.4 (range, 18.7–41.3) kg/m2. Left-sided varicocele was recorded in 153 patients (86.9%), and 74 patients (42%) had grade III varicocele. The mean duration of pain was 8.9±3.1 (range, 1–47) months. There were 78 patients (44.3%) with fewer than 3ml testicular volume differences. Regarding pain characteristics, 38.1% of the patients had dull pain, and 33.5% had dragging pain. In the review of the physical activity levels, forty-seven patients (26.7%) were in the active group, fifty-eight (32.9%) were in the moderately active group, and seventy-one (40.4%) were in the inactive group. Among the patients’ occupations, the most common ones were 35.2% office workers and 29% farmers. Preoperative demographic data are given in Table 1, and the patient's physical activity levels within their occupations are detailed in Table 2.
Patient characteristics.
| Patients (n) | 176 |
| Age (years) | |
| Mean | 24.1±2.9 |
| <20 | 41 (23.3%) |
| 20–29 | 82 (46.6%) |
| ≥30 | 53 (30.1%) |
| BMI (kg/m2) | |
| Mean | 28.6±3.4 |
| <25.0 | 46 (26.1%) |
| 25.0–29.9 | 86 (48.9%) |
| ≥30.0 | 44 (25%) |
| Varicocele laterality | |
| Left side | 153 (86.9%) |
| Bilateral | 23 (13.1%) |
| Varicocele grade | |
| III | 74 (42%) |
| II | 65 (36.9%) |
| I | 37 (21.1%) |
| Duration of pain (months) | |
| Mean | 8.9±3.1 |
| <6 | 102 (57.9%) |
| ≥6 | 74 (42.1%) |
| Testis volume difference (ml) | |
| <3 | 78 (44.3%) |
| ≥3 | 98 (55.7%) |
| Quality of pain | |
| Dull | 67 (38.1%) |
| Dragging | 59 (33.5%) |
| Throbbing | 22 (12.5%) |
| Sharp | 28 (15.9%) |
| Physical activity level* | |
| Active | 47 (26.7%) |
| Moderately active | 58 (32.9%) |
| Inactive | 71 (40.4%) |
| Occupation | |
| Office worker | 62 (35.2%) |
| Farmer | 51 (29%) |
| Sportsman | 16 (9.1%) |
| Security guard | 22 (12.5%) |
| Others | 25 (14.2%) |
BMI: body mass index.
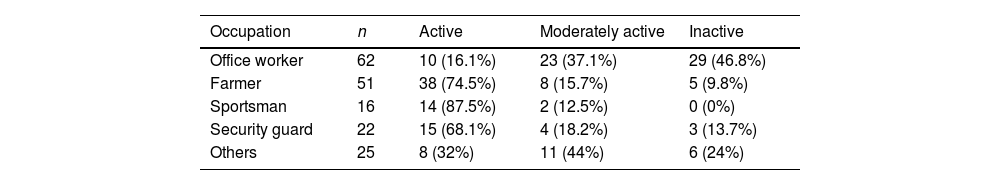
Activity level* evaluations of occupations.
| Occupation | n | Active | Moderately active | Inactive |
|---|---|---|---|---|
| Office worker | 62 | 10 (16.1%) | 23 (37.1%) | 29 (46.8%) |
| Farmer | 51 | 38 (74.5%) | 8 (15.7%) | 5 (9.8%) |
| Sportsman | 16 | 14 (87.5%) | 2 (12.5%) | 0 (0%) |
| Security guard | 22 | 15 (68.1%) | 4 (18.2%) | 3 (13.7%) |
| Others | 25 | 8 (32%) | 11 (44%) | 6 (24%) |
The activity distributions of occupations were given as a percentage.
The mean VAS score of all patients was calculated pre-operatively and post-operatively as 7.66 and 1.18, respectively. After the operation, 135 patients (76.7%) reported complete resolution of their pain (VAS score 0). Partial resolution of pain was observed in 34 patients (19.3%). Seven patients (4%) complained of the same pain level. There was no worsening of symptoms in any patient.
Univariate and multivariate analysis of age, BMI, varicocele laterality, varicocele grade, duration of pain, testicular volume difference, and quality of pain did not significantly affect the success of pain relief of varicocelectomy (p>0.05). Univariate analysis showed that patient occupations and physical activity levels significantly affected the pain level (p=0.041, p=0.032, respectively). In the multivariate analysis, it was evaluated that the physical activity levels of the patients, not their occupation, were significant in predicting the resolution of pain (p=0.077, p=0.024, respectively). The mean postoperative VAS score of physical activity levels was 1.96 in the active group, 1.24 in the moderately active group, and 0.61 in the inactive group. Only physical activity level significantly affects the success of pain relief of varicocelectomy in multivariate analysis. Detailed postoperative data are shown in Table 3.
Post-operative data.
| Factors | Pre-op VAS score | Post-op VAS score | p-ValueUnivariate analysis* | p-ValueMultivariate analysis† |
|---|---|---|---|---|
| Age (years) | 0.766 | 0.537 | ||
| <20 | 6.97 | 1.04 | ||
| 20–29 | 7.81 | 1.21 | ||
| ≥30 | 7.96 | 1.24 | ||
| BMI (kg/m2) | 0.681 | 0.455 | ||
| <25.0 | 7.33 | 1.22 | ||
| 25.0–29.9 | 7.57 | 1.13 | ||
| ≥30.0 | 8.17 | 1.23 | ||
| Varicocele laterality | 0.342 | 0.493 | ||
| Left side | 7.62 | 1.16 | ||
| Bilateral | 7.86 | 1.31 | ||
| Varicocele grade | 0.189 | 0.122 | ||
| III | 8.34 | 1.39 | ||
| II | 7.51 | 0.96 | ||
| I | 6.56 | 1.14 | ||
| Duration of pain (months) | 0.276 | 0.074 | ||
| <6 | 7.50 | 1.33 | ||
| ≥6 | 7.88 | 0.97 | ||
| Testis volume difference (ml) | 0.506 | 0.881 | ||
| <3 | 7.44 | 1.33 | ||
| ≥3 | 7.83 | 1.06 | ||
| Quality of pain | 0.133 | 0.096 | ||
| Dull | 8.03 | 1.47 | ||
| Dragging | 7.63 | 0.91 | ||
| Throbbing | 7.73 | 0.89 | ||
| Sharp | 6.78 | 1.27 | ||
| Physical activity level¥ | 0.032 | 0.024 | ||
| Active | 7.75 | 1.96 | ||
| Moderately active | 7.39 | 1.24 | ||
| Inactive | 7.82 | 0.61 | ||
| Occupation | 0.041 | 0.077 | ||
| Office worker | 7.47 | 1.09 | ||
| Farmer | 7.16 | 1.11 | ||
| Sportsman | 8.41 | 1.51 | ||
| Security guard | 7.72 | 1.38 | ||
| Other | 8.60 | 1.14 | ||
VAS: visual analog scale; BMI: body mass index.
Varicocele is one of the most common causes of scrotal pain. Although varicocele is a treatable cause of infertility and research focuses on this issue, varicocele-related scrotal pain may negatively affect patients’ quality of life and should not be underestimated. Albeit there is no consensus for the surgical treatment of varicocele-related scrotal pain in current guidelines, varicocelectomy may be considered when conservative management fails.14 Various surgical success rates for treating painful varicocele have been reported in the literature.3–5 This variability makes it challenging to decide on surgery. Few studies have investigated which patients would benefit most from the surgery. The parameters of age, BMI, laterality, location, grade, etc., were evaluated. To our knowledge patient's physical activity status has been assessed as a cause of varicocele, but its effect on persistent postoperative pain has not yet been investigated. Patients state that their pain increases with standing and physical activity and decreases with lying down.15 The cause of varicocele-related pain is not well established. Compression of the surrounding neural fibers by enlarged venous vessels could be one of the explanations.9,16,17 Valsalva, increased by physical activity, may increase pressure on venous structures. This may be effective in the formation of pain and the non-resolution of postoperative pain. We believe that evaluating the individual's physical activity level can guide clinicians in the treatment decision of varicocelectomy.
There is no consensus on the effectiveness of BMI levels in treating varicocele-related pain. Some of the researchers reported that low BMI increased the incidence of varicocele.18 Park et al. found that all patients with unsuccessful results after surgery had a BMI >22kg/m2.7 Chen et al. found higher BMI in patients who did not respond to surgical treatment, even though the results did not show statistical significance.19 Our study evaluated patients in 3 different groups according to their BMI levels. The effect of BMI level on treatment success was not statistically significant (p=0.455). We interpreted that the conflicting results in the literature may be due to the fact that factors other than BMI also influence the success of treatment.
In a meta-analysis of varicocele grade, no significant relationship was found between preoperative varicocele grade and postoperative pain resolution.8 In another meta-analysis by Han et al., there was no significant relationship between pain resolution rate and varicocele grade, but it was found to be higher in grade III varicocele.20 We found that patients with grade III varicocele had a higher preoperative mean VAS score (Table 2). However, it did not significantly affect the postoperative pain resolution rate (p=0.122).
Some studies have reported that a longer duration of pain before surgery is associated with more successful outcomes. Kim et al. compared patients who benefited from surgery and who did not. The success of the surgery was found to be higher in those with longer periods of pain (13.7 months and 4.2 months, respectively).21 It may be explained by the fact that some patients who are evaluated as scrotal pain in patients with shorter duration pain have muscle or tendon origin pain. Different cut-off values were determined in studies such as 3.6 and 9 months for pain duration.3,4,7 This complicates the evaluation and standardization of studies. We used six months as the cut-off value, determined as the chronic pain threshold in other organ diseases. In our study, the post-op mean VAS score was lower in patients with pain duration >6 months than in patients with <6 months. (0.97, 1.33 respectively). There is a trend toward statistical significance (p=0.074). Studies with larger numbers of patients are needed.
In their study on the character of varicocele-related pain, Peterson et al. reported that 63% of the patients described dull or throbbing pain and found it statistically significant.1 Kim et al. have shown that the character of pain is an independent predictor of success.21 In their study, the highest success rate was 100% (24/24) in patients who described dull pain. Patients describing dragging pain had a 96.2% success rate (51/53). None of the patients described sharp pain. However, this relationship was not found statistically significant in other studies.3,22 In our study, most patients described dull and dragging pain (71.6%). Throbbing pain and sharp pain were described less frequently. There was no statistically significant difference between treatment successes regarding pain characteristics (p=0.096). We noticed that while the pain characteristics of the patients were questioned in detail, some had difficulty distinguishing the type. This situation may have affected the result of our study on this topic.
The relationship between physical activity and varicocele has been investigated in different aspects, except for the point of view in our article. In a prospective study, healthy male volunteers and volunteers affected by varicocele are grouped as athletes and non-athletes. As a result, testicular volume loss and sperm parameters were significantly lower in the athletes in the varicocele group. It has been concluded that physical activity may have an aggravating effect on spermatogenesis in patients with varicocele.23 There is no data on pain assessment in this study. Ebiloglu et al. compared VAS scores before and after physical activity in the preoperative period.24 It was found that physical activity significantly increased pain (p=0.001). The success of the surgical techniques was compared with the VAS score in the post-op period. Subinguinal microscopic varicocelectomy was found to be the most successful method. The pain-increasing effect of physical activity was evaluated only for the pre-op period. In addition, patients were operated on with three different surgical techniques. Patients were not separated into groups according to their physical activity level. In our study, the patients were divided into three groups according to their physical activity levels and operated on with the same surgical technique. We evaluated the VAS score results both pre-operatively and post-operatively. Post op complete pain resolution rate was 90% in the inactive group and 72% in the active group (p=0.02). Four out of 7 patients whose pain remained unchanged were in the active group. An inverse correlation was found between physical activity level and operation success. We can speculate that high physical activity levels may lead to continued pressure in the neurons surrounding the veins due to continuous Valsalva, even if the testicular veins are ligated. It can be explained to patients who will undergo varicocelectomy that surgery's success in pain may be relatively lower in those with high physical activity levels.
Data on the occupations of the patients were divided into five different groups. The groups were formed by considering their physical activity intensities. Postoperative VAS scores were higher in sportsmen and security workers (1.51 and 1.38, respectively). However, no significant relationship was found in multivariate analysis (p=0.077). We explained this situation because the physical activities of patients from the same profession may not be at the same level (Table 2). We may consider that the level of physical activity is a more objective criterion than occupation.
Microscopic subinguinal varicocelectomy is currently the most preferred surgical method with high success and low complication rates.25 One of the limitations of our study is that two different surgeons performed the operations. In order to overcome this limitation, all the patients were operated by two sufficient experienced surgeons with the same technique. The number of patients with persistent pain in our study may not be considered enough to support our results, so we know that further studies with more patients are needed. Another limitation is that the hormone profile of our patients was not examined. High physical activity can affect the hormonal status of patients. We did not routinely examine the hormone profile because it would not change our follow-up and treatment plan. This issue could be addressed in future studies.
In conclusion, microscopic varicocelectomy is an effective treatment method in patients with painful varicocele who do not respond to conservative management. Occupation alone is not a determining factor in predicting the operation's success. It seems there is a significant correlation between low physical activity and the resolution of varicocele pain. The possibility of persistence of pain after the operation may be discussed with patients according to their physical activity level.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Ethical approvalThe study protocol was approved by the Ethics Committee of Karamanoglu Mehmetbey University Faculty of Medicine (date: 25.05.2021; Decision No: 03-2021/07).
FundingNone declared.
Conflict of interestThe authors declare they have no conflicts of interest.
We thank Metin Savun (Basaksehir Cam and Sakura City Hospital, Clinic of Urology) and Guven Erbay (Karamanoglu Mehmetbey University, Faculty of Medicine, Department of Urology) for re-examination of the patients and their valuable contributions to our study.