Paratesticular fibrous pseudotumor (PFP) is a rare benign tumor that is not a neoplasm but a reactive fibrous inflammatory hyperplasia. Paratesticular fibrous pseudotumor occurs from intrascrotal tissues, such as tunica vaginalis, epididymis, or spermatic cord. Definitive diagnosis requires pathological examination. Radical orchiectomy should be avoided when possible, and local excision should be performed due to the lack of obvious evidence of potential malignancy.
Case reportA 61 years old patient was referred to our clinic with complaints of right scrotal mass. Doppler ultrasonography is observed for the right epididymis in the neighborhood of 30×26×21mm hypoechoic mass. Tumor markers were negative. Frozen came as negative. Testicular mass was excised with testis preventive approach. Pathology report revealed that paratesticular fibrous pseudotumor.
ConclusionAccording to this article frozen section should be done in paratesticular masses to avoid unnecessary radical orchiectomy.
El seudotumor fibroso paratesticular es un tumor benigno raro que no es una neoplasia sino una hiperplasia o proceso reactivo inflamatorio no tumoral. El seudotumor fibroso paratesticular aparece en el tejido intraescrotal, como la túnica vaginal, epidídimo, o el cordón espermático. El diagnóstico definitivo requiere un examen patológico. Debe evitarse la orquiectomía radical en la medida de lo posible. Asimismo, deberían realizarse escisiones locales en caso de no encontrar una evidencia clara de su potencial malignidad.
Informe del casoUn paciente de 61 años dirigido a nuestra clínica con quejas de una masa en el escroto derecho. Se observa una masa hipoecoica de 30×26×21mm en las proximidades del epidídimo derecho durante el examen con ecografía doppler. Los marcadores tumorales fueron negativos. Se realizó biopsia de la masa como procedimiento preventivo testicular. El informe patológico confirmó que se trataba de un seudotumor fibroso paratesticular.
ConclusiónDe acuerdo con este artículo, la biopsia del tejido congelado debería realizarse en masas paratesticulares para evitar orquiectomías radicales innecesarias.
Fibrous pseudotumor is an uncommon benign tumor that originated from the connective tissues of the testicular and paratesticular soft tissues. That accepted as reactive non-neoplastic lesions and the pathogenesis is unknown. The majority of these pseudotumors are found adjacent to the testis, but some are located in the spermatic cord.1 Fibrous pseudotumor is the second most common paratesticular mass after adenomatoid tumor, and accounts for approximately 6% of all paratesticular lesions and tumors.2 Although the peak incidence is in the third decade of life, fibrous pseudotumor has been reported in all age groups.
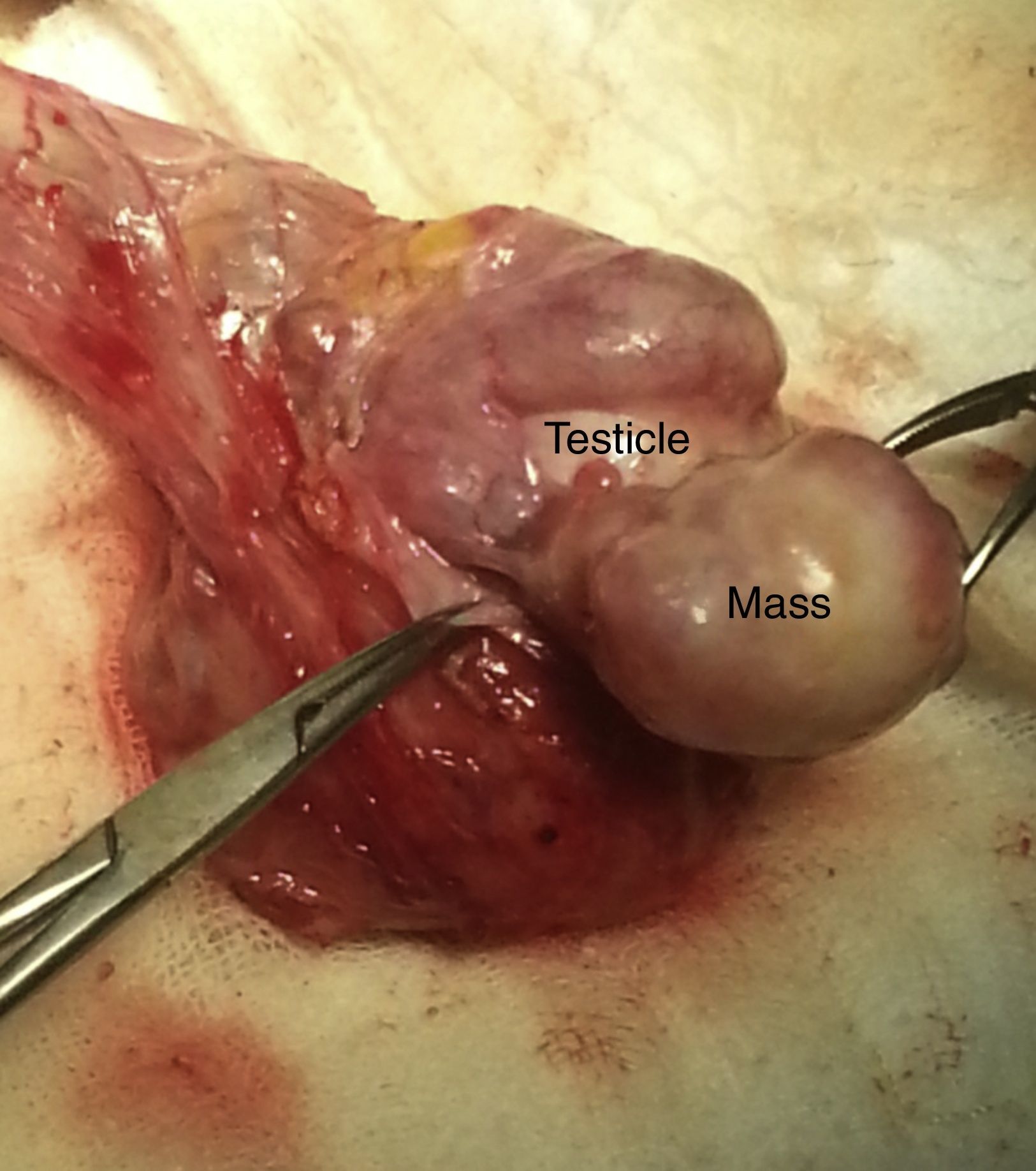
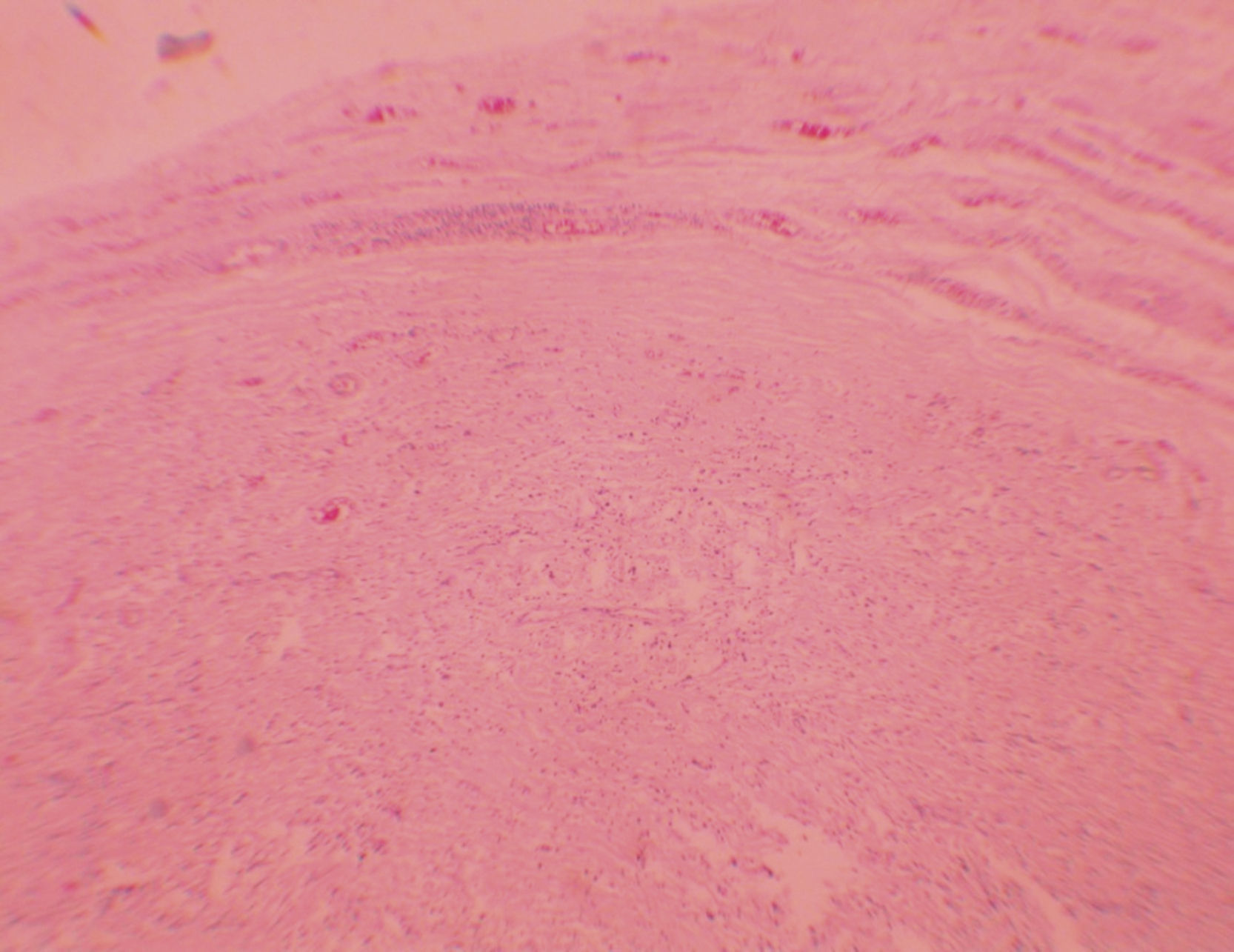
Case reportA 61 years old patient was referred to our clinic with complaints of right scrotal mass. On physical examination, right testis in the neighborhood, about 3cm hard in texture mass was palpated. Laboratory findings were unremarkable. Tumor markers were negative. Tuberculosis and brucellosis were not detected. Doppler ultrasonography of scrotal testes homogeneous internal echoes is observed, and the right epididymis in the neighborhood of 30×26×21mm hypoechoic mass was seen. Peroperative evaluation; testicular parenchyma attached a thin stalks; epididymis neighbor about 3cm in diameter mass lesion was hard and irregular surface (Fig. 1). Frozen came as negative. Testicular mass was excised with testis preventive approach. Pathology report revealed that PFP (Fig. 2). There was no recurrence at 12 months follow patients.
Fibrous pseudotumor typically presents as a painless scrotal mass and discomfort is frequently reported. In approximately a third of cases there is a history of trauma or epididymo-orchitis, and in nearly half of cases there is an associated hydrocele.3 Paratesticular fibrous pseudotumor was first reported by Balloch in 1904. The incidence of fibrous pseudotumor has been reported to comprise approximately 6% of paratesticular lesions and tumors.
In the differential diagnosis of fibrous pseudotumour of the paratesticular region, paratesticular lesions (adenomatoid tumors, cystadenomas, spermatoceles, hydroceles, varicoceles, hernias, scrotal calculi, polyorchidism, solitary fibrous tumor, leiomyoma, neurofibroma, fibroma of the tunics, idiopathic fibromatosis and malignant tumors) and intratesticular lesions (tunica albuginea cysts, testicular simple cysts, epidermoid cysts, cystic ectasia of the rete testis, intratesticular varicocele, adrenal rest tumors, splenogonadal fusion and malignant tumors) should be included. Based on the morphologic appearances of the lesions, the results of radiologic findings, the presence or absence of an infiltrative border, and the results of immunohistochemical studies, distinguishing among these lesions and tumors should be possible in most instances.4–6
No specific laboratory abnormalities are associated with fibrous pseudotumor. Scrotal ultrasound may demonstrate several hypoechoic or hyperechoic lesions adjacent to the testis with normal testicular echotexture. The echogenicity of the lesion depends on the degree of collagenation, calcification or myxoid change.
Testicular/paratesticular fibrous pseudotumors are believed to be reactive lesions resulting from trauma, hydrocele, or infection that can involve the testis, epididymis, spermatic cord, testicular tunics, and paratesticular tissues. These lesions have a number of synonyms including fibromatous periorchitis, nodular fibropseudotumor, nonspecific paratesticular fibrosis, reactive periorchitis, proliferative funiculitis, and many others. Because some lesions lack inflammation and are not nodular, the term fibrous pseudotumor is preferred.7
Fibrous pseudotumor is not a neoplasm but a reactive fibrous inflammatory hyperplasia. Radical orchiectomy should be avoided when possible, and local excision should be performed because of the lack of obvious evidence of potential malignancy.8 Although a benign lesion, fibrous pseudotumors may necessitate a radical orchiectomy in certain situations. As described previously, they clinically can mimic a neoplasm, and viability of the remaining parenchyma may be a concern.9
Paratesticular fibrous pseudotumours may present as nodular or diffuse masses, which may simulate malignancy clinically. The various paratesticular malignant tumors occurring in adults are rhabdomyosarcoma, leiomyosarcoma, liposarcoma, fibrosarcoma, malignant fibrous histiocytoma, and metastatic carcinomas. Since paratesticular fibrous pseudotumors may mimic any of these malignant tumors clinically, surgical management is the treatment of choice for these lesions. In such situations, the role of an intra-operative frozen section may be of paramount importance, and it would help if both the surgeons and pathologists are aware of fibrous pseudotumors in the paratesticular region.10 Frozen section assessment in testicular and paratesticular lesions suspicious for malignancy; its role in preventing unnecessary orchiectomy.11
In a recent study, it has been shown that testis-sparing surgery in small size (<1cm) Leydig cell tumors is safe as well as to all other benign testicular masses.12
Awareness of this entity combined with intra-operative frozen section may prevent performance of an unnecessary radical orchiectomy, especially in younger patients. These results suggest that frozen section assessment is useful for permitting testicular preservation, especially in men with small, nonpalpable, incidentally found masses as well as other benign lesions where a clinical diagnosis of malignancy is in doubt. Because these lesions cannot be distinguished preoperatively, from a malignancy, surgical exploration is usually undertaken, resulting in surgical excision. Orchiectomy is often opted when there is uncertainty regarding malignancy or in cases where the tunics are too diffusely involved to allow preservation of testicular tissue. Intraoperative frozen sections may help obviate radical orchiectomy.
According to this article frozen section should be done in paratesticular masses to avoid unnecessary radical orchiectomy. Fibrous pseudotumor as a rare benign tumor of scrotum should be taken into consideration among the scrotal masses.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interestThe authors declare no conflict of interest.