A 28-year-old man diagnosed with primary adrenal insufficiency (Addison's disease) in 2002. Following diagnosis, replacement therapy with hydrocortisone and fludrocortisone was indicated. Hydrocortisone replacement therapy was unsuccessful, and increased ACTH levels as high as 996pg/dl were observed on outpatient follow-up. A pituitary MRI revealed a pituitary microadenoma. These findings raised three possibilities: (1) treatment is insufficient; (2) there is no relationship between Addison's disease and pituitary microadenoma; and (3) the microadenoma is similar to Nelson's syndrome. This latter is the most satisfactory explanation of this patient's clinical picture.
Un varón de 28 años fue diagnosticado de insuficiencia suprarrenal primaria autoinmune (enfermedad de Addison) en el año 2002. Tras ello, se indica tratamiento sustitutivo con hidrocortisona y fludrocortisona. En el seguimiento ambulatorio se objetiva un aumento de los niveles de ACTH, llegando a 996 pg/dl, con tratamiento sustitutivo con hidrocortisona que no logra suprimir la ACTH. Por ello se realiza RNM de hipófisis donde se objetiva un microadenoma hipofisario. Ante estos hallazgos se plantearon tres posibilidades: 1.- El tratamiento es insuficiente; 2.- No existe relación entre la enfermedad de Addison y el microadenoma hipofisoario; 3.- El microadenoma se considera una situación clínica similar al síndrome de Nelson. Esta última respuesta es la que da una explicación más satisfactoria al cuadro clínico de este paciente.
Addison's disease is characterised by failure of the adrenal glands to produce sufficient steroid hormones, the most common aetiology being autoimmune adrenalitis and tuberculosis. This causes the classic signs of suprarrenal insufficiency, along with the melanoderma typical of increased adrenocorticotropic hormone (ACTH) secretion.1,2 ACTH overproduction in response to decreased cortisol levels can also be caused by an autonomously functioning pituitary adenoma, as seen in Nelson's syndrome.3,4 The ACTH increase seen in Addison's disease could also be due to primary pituitary ACTH hypersecretion unrelated to cortisolemia,5 or to both of the foregoing cases. We present the case of a pituitary microadenoma in a patient with Addison's disease that could be interpreted as either Nelson's syndrome or primary pituitary ACTH hypersecretion coexisting with Addison's disease. The gradual increase in ACTH levels despite appropriate replacement therapy with hydrocortisone would seem to bear out the latter hypothesis. This clinical situation could also be explained by ACTH hypersecretion secondary to adrenal dysfunction that eventually becomes autonomous, as in tertiary hyperparathyroidism in kidney failure.6
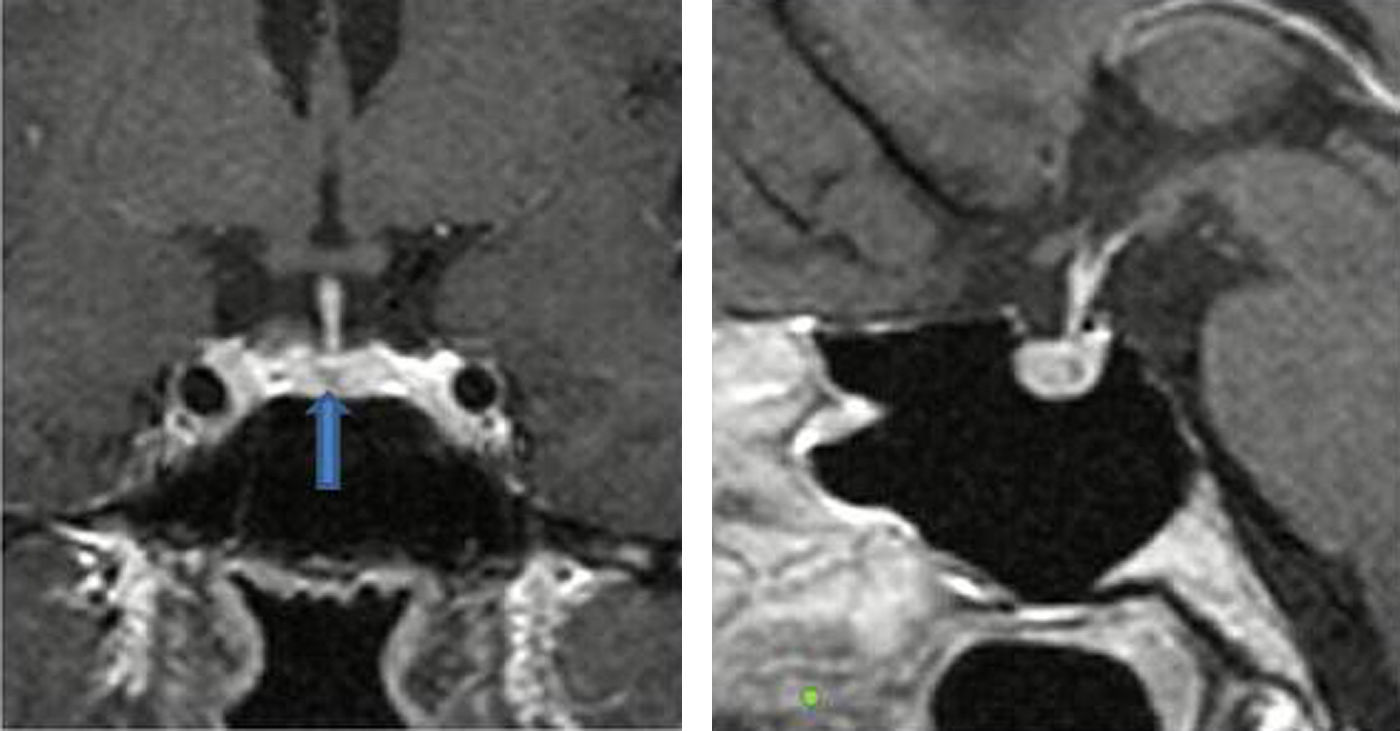
Case studyA 28-year-old man was admitted to our hospital in 2002 for periodic paralysis, anorexia, weight loss of 8kg in the previous 12 months, vomiting and general malaise. On physical examination, he presented hyperpigmentation of the palms of the hands, oral mucosa, and axillary and inguinal folds. Arterial pressure was 90/60mmHg, heart rate was 96bpm, axillary temperature was 37°C, weight 62kg and height 1.69cm. Emergency laboratory tests showed hyponatraemia (128mEq/l) and mild hyperpotassaemia (6.1mEq/l), slightly elevated BUN and normal creatinine. Once ionic changes had been normalised, we measured basal cortisol (less than 1mcg/dl) and ACTH levels (336pg/ml, normal levels up to 50pg/ml). This was followed by a prolonged ACTH stimulation test, with no elevation of cortisolaemia. We started replacement treatment with 30mg hydrocortisone and 0.1mg fludrocortisone daily, with outpatient follow-up. Antiadrenal antibody levels were >1/20 (normal, absent). On follow-up, ACTH levels remained elevated and did not respond to replacement therapy, so this was increased to 40mg hydrocortisone daily. ACTH was measured every 2 years between 2004 and 2014, showing levels of 405, 438, 710, 782, 489 and 996pg/ml. Prolactin, FSH-LH, TSH and HGH levels were normal. Over the prolonged follow-up period, the patient has adhered strictly to the therapeutic regimen (Morisky Green test), and has had no intercurrent disease or need for hospitalisation. On the basis of ACTH levels, we decided to perform a targeted MRI examination of the pituitary region, which revealed a cold lesion measuring 2.5mm, compatible with a pituitary microadenoma (Fig. 1). The long clinical evolution, with normal findings on serial campimetry and imaging studies (chest X-ray and abdominal ultrasound), all but rules out the coexistence of ectopic ACTH secretion.
DiscussionOur patient meets the criteria for ACTH-secreting pituitary adenoma, with no clinical signs of a space-occupying lesion. As the most characteristic sign of increased ACTH is melanodermia, we decided to perform periodic follow-up of ACTH levels with laboratory tests and MRI of the pituitary gland. However, other non-specific signs associated with this case could benefit from some strategies reported in the literature.7
Nelson's syndrome, the enlargement of an autonomous ACTH-secreting pituitary adenoma, is a typical clinical presentation following bilateral adrenalectomy for Cushing's syndrome, and would explain the clinical picture following autoimmune adrenalitis in this case.8 The extended time lapse between onset of symptoms and diagnosis of Addison's disease in this patient could have caused Nelson's syndrome, as during this period ACTH secretion continued unchecked due to low cortisol levels.9,10 Although many authors suggest that this is not such a rare occurrence, a Medline search retrieved only 1 article specifically analysing this problem. For this reason, we have decided to adopt a wait-and-see, symptom-guided approach complemented by follow-up campimetry tests and imaging studies.4
Another, albeit unlikely, hypothesis put forward to explain these symptoms is non-adrenal function-related pituitary ACTH hypersecretion, in which both processes would have developed independently.
Treatment strategies, in the absence of evidence of any other hormonal dysfunction other than ACTH, and no neurological symptoms, remain unclear.6 However, ACTH hypersecretion could improve with replacement therapies aimed at improving adrenal hormone homeostasis.11 This approach is similar to that taken in diabetes, where insulin is replaced by a basal-bolus regimen.
ConclusionsWe present a case of Addison's disease treated with replacement therapy that actually increased, rather than reduced, ACTH levels. Observing rising levels over time, we decided to perform MRI of the pituitary gland, which showed the presence of a microadenoma. Various hypotheses have been put forward to explain this phenomenon:
- 1.
Conventional treatment is ineffective in inhibiting ACTH production.
- 2.
The pituitary microadenoma is unrelated to Addison's disease or any suprarenal dysfunction.
- 3.
The microadenoma is caused by an autoimmune adrenalitis, and symptomatology is similar to Nelson's syndrome.