Millium colloid is a rare cutaneous deposition disorder of unknown aetiology on light-exposed skin. It presents as flesh-coloured or yellow papules. A skin biopsy and light microscopy study is required for diagnosis, with findings of fissured eosinophilic colloid masses in the papillary dermis, with solar elastosis that is separated from the epidermis by a Grenz zone containing normal collagen. There is no single effective treatment. We present a case report of a 42-year-old man with papular lesions on the dorsum of both hands and a history of prolonged sun exposure.
El millium coloide es una enfermedad de depósito, presente en áreas fotoexpuesta y de etiología desconocida. Clínicamente se identifica como lesiones de aspecto papular de color rosa o amarillo. Para su diagnóstico es necesario realizar una biopsia de piel para microscopía de luz, donde se observan masas eosinofílicas fisuradas en la dermis papilar en presencia de elastosis solar y una zona de Grenz de fibras elásticas que separa la lesión del resto de la epidermis. Hasta el momento no existe un tratamiento de elección. Se presenta el reporte de un caso de un paciente masculino de 42 años con lesiones de aspecto papular en dorso de manos, con el antecedente de exposición crónica a la luz solar.
Colloid milium is a cutaneous deposit disease of unknown pathogenesis that usually presents on areas of the skin exposed to sunlight. Clinically, it is characterised by yellow or flesh-coloured papules. It can only be diagnosed by a skin biopsy, and evolution is chronic and asymptomatic.
A case reportWe present the case of a 42-year-old unmarried businessman presenting with a 4-year history of diffuse dermatitis involving the dorsum of both hands. The lesions involved the metacarpophalangeal and interphalangeal joints, and consisted of skin-coloured or pink papules measuring 0.5cm in diameter, with well-defined borders and a rough surface (Figs. 1–3). Onset was marked by pain in the joints of both hands, particularly in the morning, with no stiffness or other symptoms. The patient was referred to the Rheumatology department, and later to our service for diagnosis.
The patient's medical history was unremarkable, he did not smoke, drink or take drugs, and was not taking any medication. He had been driving a “mototaxi” for 4 years.
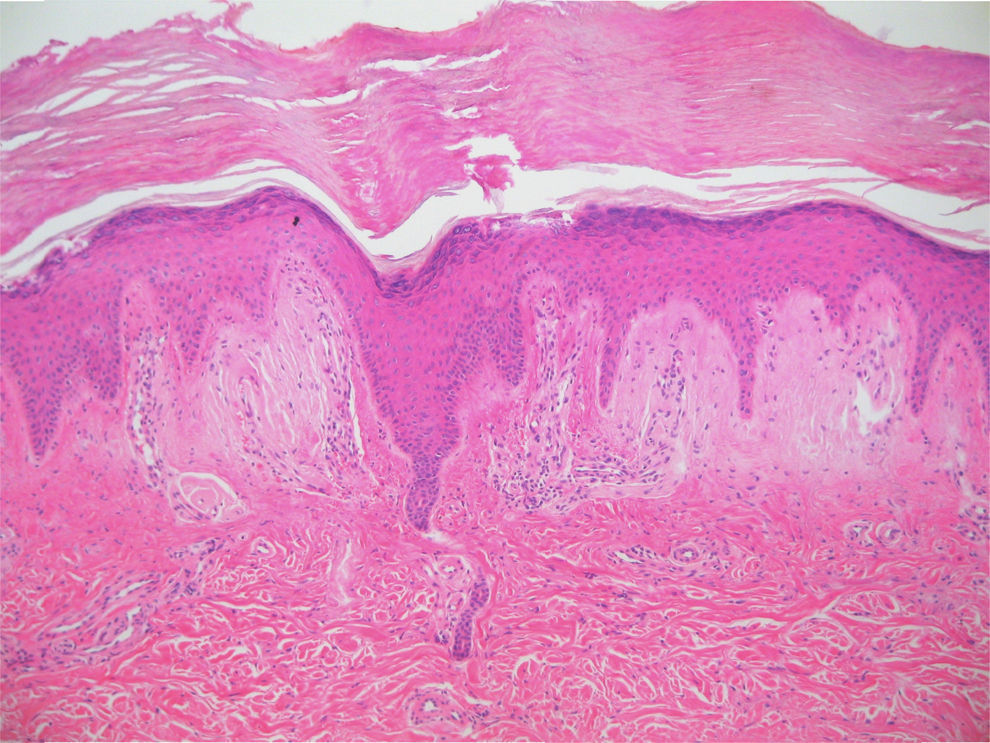
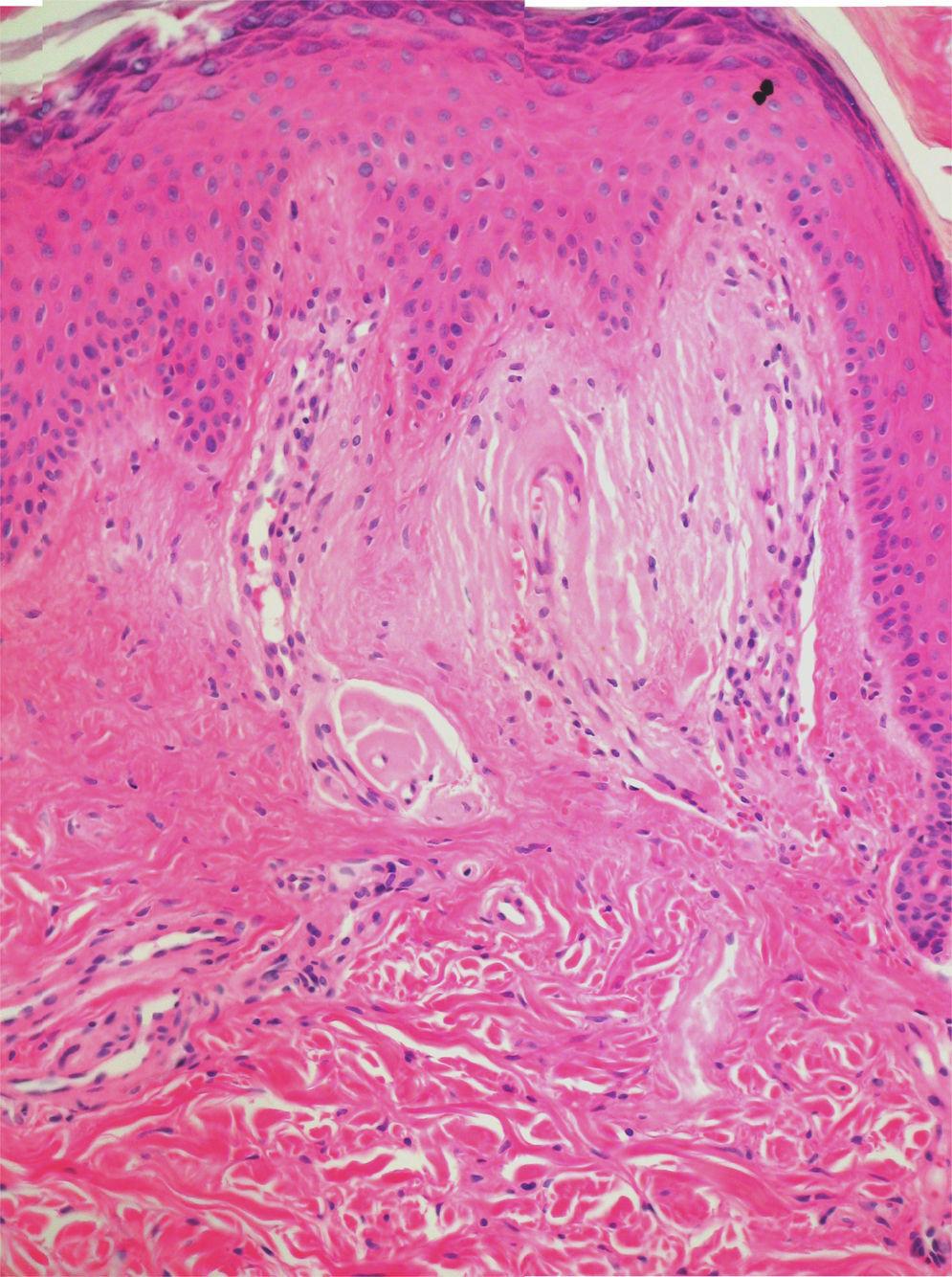
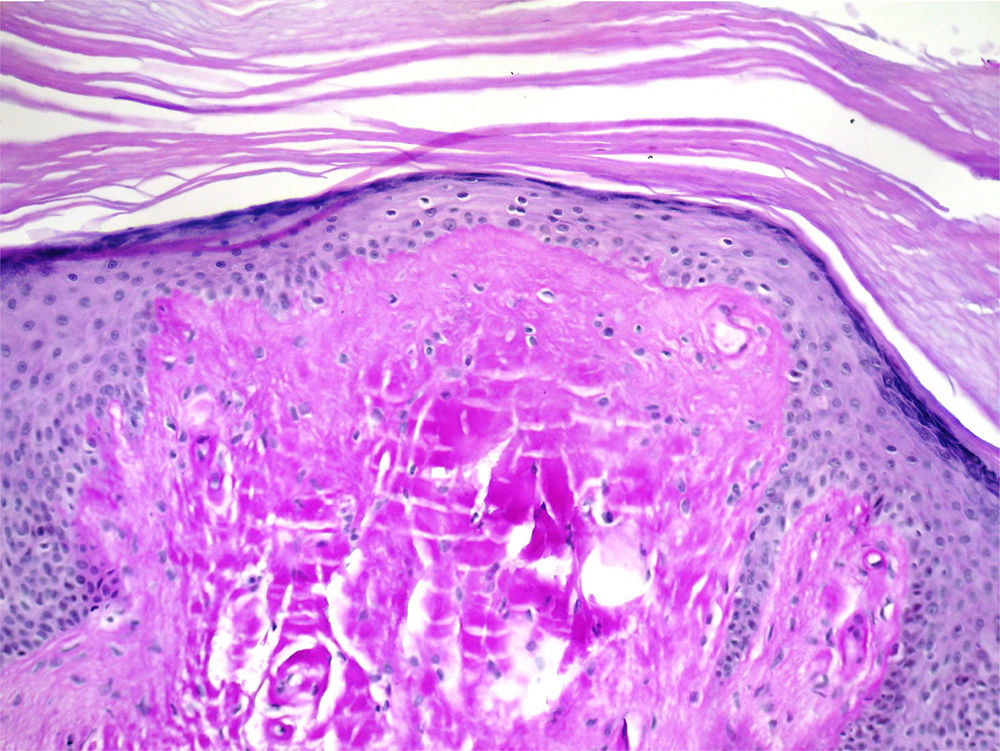
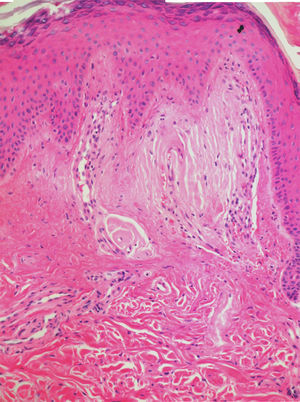
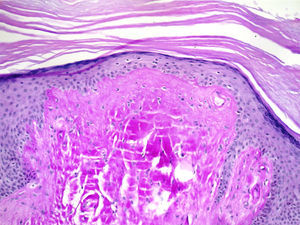
The clinical impression suggested Gottron's papules, and after ruling out cutaneous mucinosis, we performed a skin biopsy using a 4.0mm biopsy punch, which was sent for histopathology. Light microscopy findings were abundant compact hyperkeratosis with patches of parakeratosis, moderate, irregular epidermal acanthosis with areas of elongation and thickening of interpapillary ridges. Deposits of pale, eosinophilic, amorphous, compact material substituting collagen fibres were observed in the superficial, mid and deep layers of the dermis, compressing the adnexa and capillaries. The material was PAS positive and marginally positive for Congo red and crystal violet, and was identified as colloid. Mild lymphohistiocytic infiltrate, oedema, and areas of erythrocyte extravasation were also observed. On the basis of these findings, colloid milium was diagnosed (Figs. 4–6).
Colloid milium is a rare cutaneous deposit disease. The pathogenesis of this condition remains unclear, although several suggestions have been put forward, including the notion that it is secondary to rupture of collagen or elastin fibres resulting in accumulation of serum proteins or fibroblasts products. Exposure to sunlight is thought to be a pivotal factor and could be responsible for the structural damage caused to the elastin, thereby preventing elastin synthesis in fibroblasts. It has also been suggested that sunlight could contribute to the degradation of proteins such as elastin, and lead to the destruction of elastin fibres.1–4
Colloid milium has been classified into four types: adult, juvenile, nodular, and an adult-onset variety associated with the use of hydroquinone and ochronosis, giving rise to the pigmented subtype.1–3 The most common form of the disease is the adult form, which affects men and women in a ratio of 4:1.4
It usually presents as firm, amber, pink or yellow papules that vary in size from 0.5 to 5mm and contain a yellow, mucoid material that is expressed when pressure is applied. The papules form on hyperpigmented and hypertrophic skin. The lesions are usually asymptomatic, and evolve over a period of 3 years. They are usually limited to areas of exposed skin, such as the face, dorsa of the hands, either side of the neck and on the outer ear. However, some studies have reported cases of colloid milium appearing on areas of skin that are not exposed to ultraviolet light.1,2
Diagnosis is based on light microscopy study of a skin sample, which shows fissured eosinophilic colloid masses in the papillary dermis, with solar elastosis and a Grenz zone of elastin fibres that separates the lesion from the rest of the epidermis.4 Some fibroblasts can be observed in cleft formations, together with some lymphocytes, mast cells and enlarged veins, with preservation of adnexa. Amyloid stains are negative or equivocal. Immunohistochemistry study with anti-keratin antibodies is positive for colloid. Under electronic microscopy, remnants of desmosomes together with binding and nuclear proteins have been found in the colloid deposits.5,6
Juvenile colloid milium is a rare form with onset before puberty. It can be familial, and is thought to follow an autosomal dominant pattern of inheritance. Patients with colloid milium are predisposed to degeneration of basal keratinocytes caused by exposure to sunlight. The disease usually involves the face, and often resolves in adulthood.5,6 The lesions are both clinically and histologically similar to the adult form, with absence of the Grenz zone.4 Only one familial case has so far been reported in the literature.7
The nodular variety has also been classified as a type of amyloidosis and usually presents as an isolated nodule measuring approximately 5cm in diameter on the fact, trunk or scalp. Most lesions are located on the trunk, and have been associated with multiple myeloma. Histological findings include a flat epidermis with subepidermal colloid masses.
Differential diagnosis is with calcinosis cutis, millia cysts, multiple syringoma and amyloidosis.8
There is no consensus on the treatment of choice, and various strategies have been used, including dermabrasion, curettage, cryotherapy, erbium laser resurfacing, retinoic acid, etc.,9 although results have been inconclusive. Gomes et al.10 report two cases in which they used photodynamic therapy with methyl-aminolevulinate cream as photosensitizer prior to curettage, with no recurrence at the 1-year follow-up visit. Li et al.11 used a fractionated CO2 laser, obtaining adequate results over a 3-month follow-up.
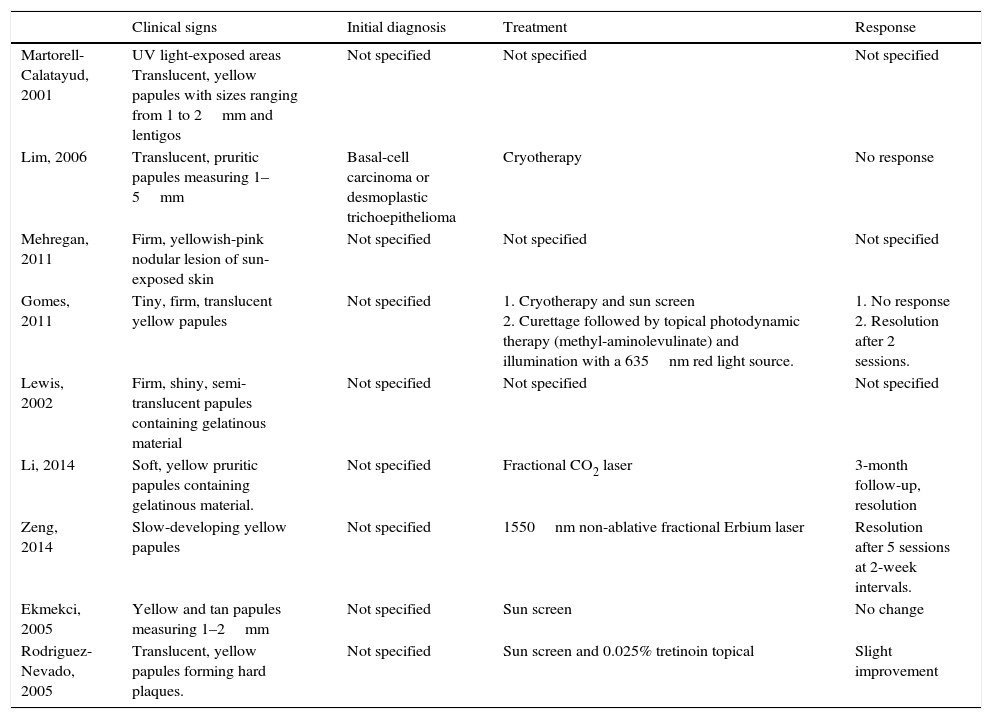
In the case reported here, the condition was evidently triggered by chronic exposure to sunlight while the patient was riding his motorcycle. Response to topical corticosteroids was poor, and with no improvement the patient decided to suspend treatment. At 6-month follow-up, the dermatitis was asymptomatic and showed no signs of change; however, the patient is now willing to try a new approach. Table 1 shows a summary of cases of colloid milium reported in the literature.
Comparison of clinical factors and treatment in cases of colloid milium reported in the literature.
| Clinical signs | Initial diagnosis | Treatment | Response | |
|---|---|---|---|---|
| Martorell-Calatayud, 2001 | UV light-exposed areas Translucent, yellow papules with sizes ranging from 1 to 2mm and lentigos | Not specified | Not specified | Not specified |
| Lim, 2006 | Translucent, pruritic papules measuring 1–5mm | Basal-cell carcinoma or desmoplastic trichoepithelioma | Cryotherapy | No response |
| Mehregan, 2011 | Firm, yellowish-pink nodular lesion of sun-exposed skin | Not specified | Not specified | Not specified |
| Gomes, 2011 | Tiny, firm, translucent yellow papules | Not specified | 1. Cryotherapy and sun screen 2. Curettage followed by topical photodynamic therapy (methyl-aminolevulinate) and illumination with a 635nm red light source. | 1. No response 2. Resolution after 2 sessions. |
| Lewis, 2002 | Firm, shiny, semi-translucent papules containing gelatinous material | Not specified | Not specified | Not specified |
| Li, 2014 | Soft, yellow pruritic papules containing gelatinous material. | Not specified | Fractional CO2 laser | 3-month follow-up, resolution |
| Zeng, 2014 | Slow-developing yellow papules | Not specified | 1550nm non-ablative fractional Erbium laser | Resolution after 5 sessions at 2-week intervals. |
| Ekmekci, 2005 | Yellow and tan papules measuring 1–2mm | Not specified | Sun screen | No change |
| Rodriguez-Nevado, 2005 | Translucent, yellow papules forming hard plaques. | Not specified | Sun screen and 0.025% tretinoin topical | Slight improvement |
The authors declare that they have no conflict of interests.