Awake craniotomy for neurostimulation can be managed with different anaesthetic techniques, ranging from local anaesthesia or local anaesthesia with sedation to intermittent general anaesthesia.
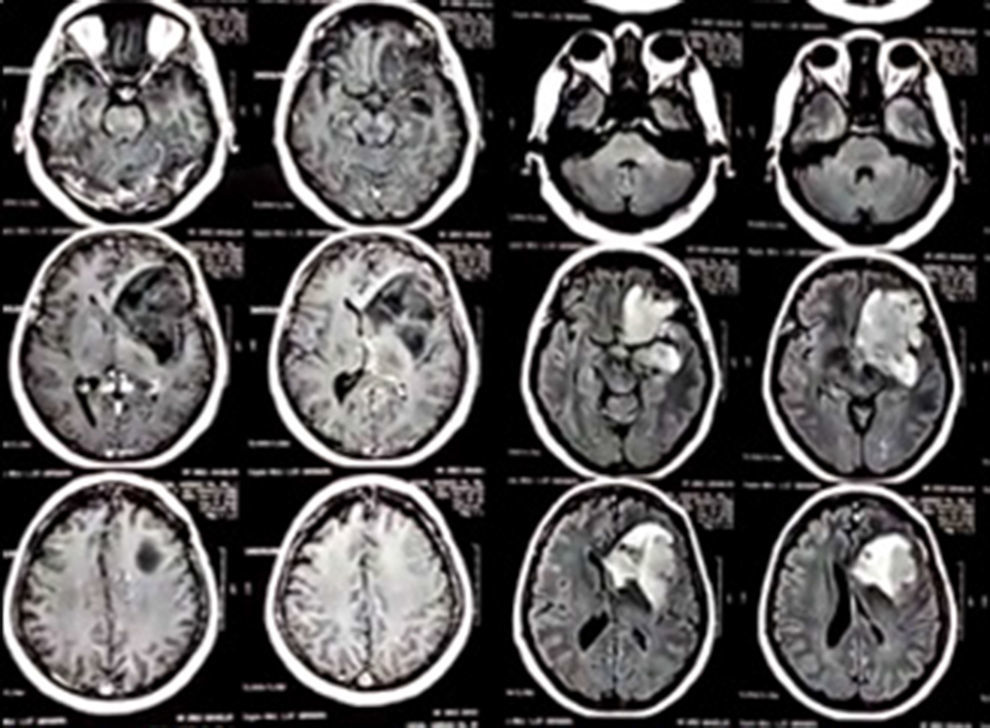
Materials and methodsWe present the case of a 56-year-old female who was diagnosed with a frontal astrocytoma which required surgical resection. Her magnetic resonance imaging study showed a space-occupying lesion in her left frontotemporal region, which was exerting a mass effect on the midline structures. Anatomically, the tumour involved the language area and motor tracts. It was therefore decided to perform craniotomy with the patient awake during the procedure, to allow intraoperative cortical mapping in order to preserve the language and motor functions.
ResultsThis case was managed with a scalp nerve block as local anaesthesia plus intravenous sedation without airway instrumentation. We reviewed the literature about patient management during awake craniotomy.
La craneotomía con paciente despierto en el momento de la neuroestimulación se puede manejar con diferentes técnicas anestésicas, las cuales van desde anestesia local, anestesia local más sedación y anestesia general intermitente.
Material y métodosSe presenta el caso clínico de una mujer de 56 años de edad en quien se realizó diagnóstico de astrocitoma frontal el cual requirió resección quirúrgica. En su estudio de imagen por resonancia magnética se evidenció un proceso ocupante en región fronto temporal izquierda, el cual presentó efecto de masa sobre estructuras de la línea media. La tumoración involucra anatómicamente área de lenguaje así como tractos motores por lo que se decidió realizar craneotomía con paciente despierta para llevar a cabo mapeo cortical intraoperatorio con el objetivo de preservar las funciones de lenguaje y motoras.
ResultadosEste caso fue manejado con un bloqueo de escalpe como anestesia local, más sedación intravenosa sin instrumentación de la vía aérea. Se hace una revisión de la literatura sobre el manejo del paciente para craneotomía despierto.
Brain surgery with the patient awake was practised long before the introduction of anaesthesia. It was in the 1920s, however, with the work of W. Penfield, when craniotomy using techniques under conscious sedation began to be performed for location of epilepsy foci and surgical management. There is a report dating from 1929 about one awake craniotomy under local anaesthetic for resection of a large brain tumour by Dr Harvey Williams Cushing. In 1950, H. Olivecrona perfected these techniques and used the procedure especially for the treatment of brain tumours.1,2
Awake craniotomy has become a common procedure for tumour surgery.3 It is now widely used for the resection of lesions close to or within eloquent areas.1,4
Anatomically, there are defined eloquent areas. However, the location and prognosis of function using classic anatomical criteria is insufficient, due to the variability in the organisation of the cortex, distortion of cerebral topography resulting from the mass effect of the tumour and functional reorganisation due to the plasticity of the neurons.5,6
Awake craniotomy for mapping of motor and language functions has increased both efficacy and safety in the resection of primary and metastatic tumours.7
For anaesthetic care to be successful in an awake patient, provision of adequate analgesia and sedation that still allow the patient to be conscious and cooperative during monitoring is essential, as this will make it easier for the patient to tolerate the procedure and at the same time facilitate accurate neurological monitoring.4
Case reportThis was a 56-year-old female patient brought into surgery for tumour resection under an asleep–awake–asleep anaesthetic technique for craniotomy with cortical mapping. Her previous history included smoking, removal of giant cell tumour from the first phalanx of the middle finger of her left hand 21 years earlier, caesarean section without anaesthetic or surgical complications, systemic hypertension diagnosed 3 years earlier and managed with enalapril, metoprolol and acetylsalicylic acid and absence seizures managed with clonazepam and levetiracetam. She wore glasses and was right handed and bilingual. This report was approved by the hospital bioethics committee and informed consent was granted by the patient, subject to the rules on confidentiality and personal data protection.
Following onset 2 years earlier of migraine-type headaches and difficult to control hypertension, she was admitted to hospital, where they made the incidental finding of brain cancer in the frontal region.
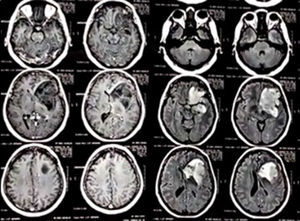
Astrocytoma was diagnosed from biopsy and managed conservatively. Twelve months later, she began to have absence seizures, which were managed and effectively controlled pharmacologically with clonazepam and levetiracetam. Three months prior to the surgical intervention, the patient had a magnetic resonance imaging (MRI) scan, which showed the tumour (see Image 1).
In view of the fact that anatomically, the tumour involved the language area and motor tracts, it was decided to perform awake craniotomy in order to carry out intraoperative monitoring, with the aim of preserving the language and motor functions while resecting the tumour.
On physical examination, the patient was found to be obese at 85kg and 1.57m in height, in good general condition, with normal pulses and regular heart sounds with no murmurs or adventitious sounds. Airway Mallampati grade II, short neck, wearing removable dentures. Had a neuropsychological assessment from 2 weeks prior to the intervention where it was reported that the patient had no language difficulties of any kind except during the ictal period. Cardiology assessment concluded that the patient was a grade I risk for anaesthetic and surgery and so did not require any special perioperative considerations.
Anaesthetic techniqueAs she was undergoing a surgical procedure, two peripheral lines were inserted and ondansetron 8mg, parecoxib 40mg and omeprazole 40mg were administered intravenously 40min beforehand. The patient was taken into the operating theatre and positioned comfortably in supine position on a thermal mattress, 2mg of midazolam was administered IV and she was attached to a 5-lead ECG monitor, pulse oximetry, skin temperature, non-invasive blood pressure and bispectral index (BIS). Reservoir mask in place at 10l/min with capnography line. After sedation, Foley catheter inserted to monitor urine output. Parameters on admission: blood pressure (BP) 105/70mmHg; temperature 36°C; heart rate (HR) 62bpm; BIS 85; maintaining spontaneous ventilation.
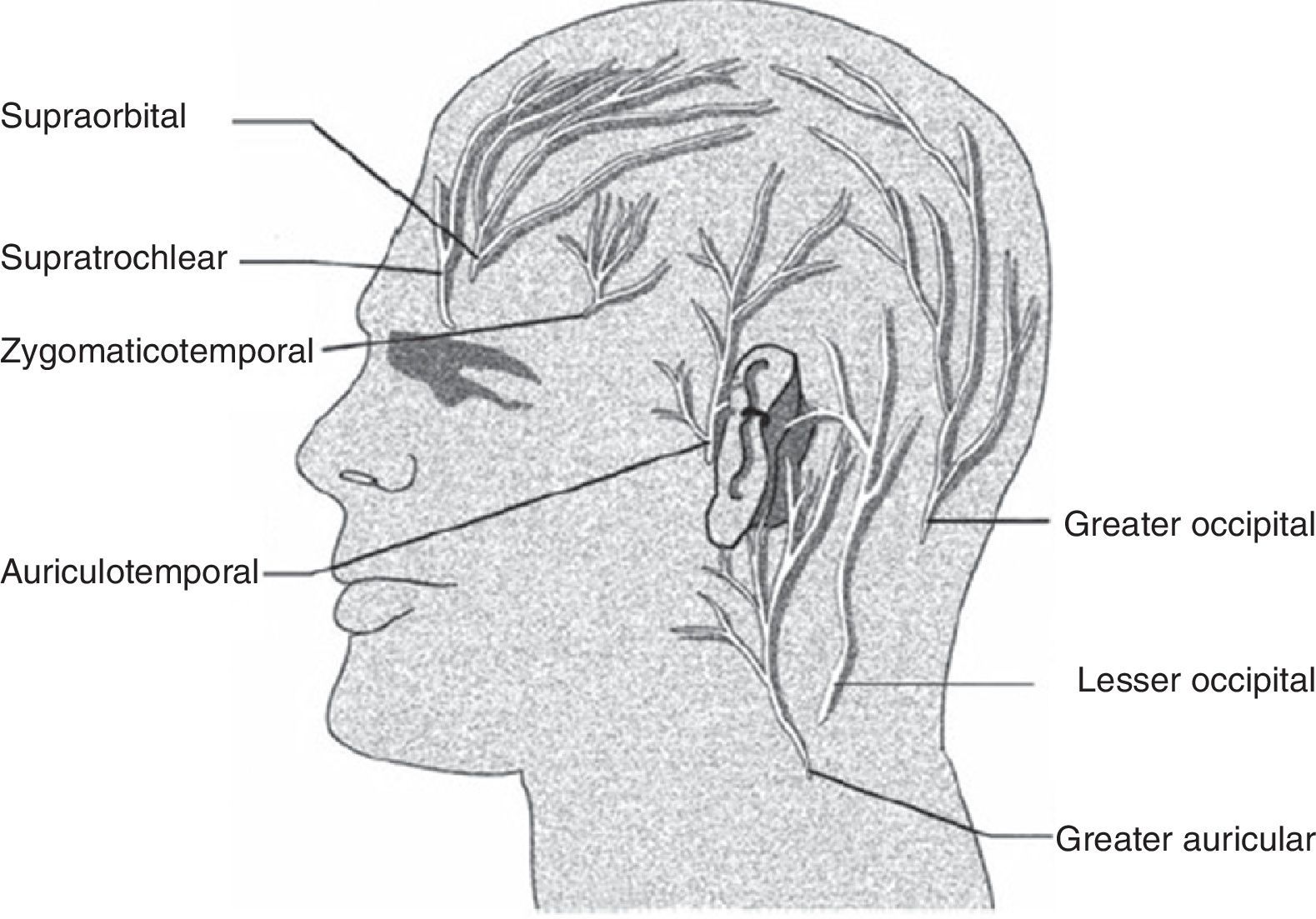
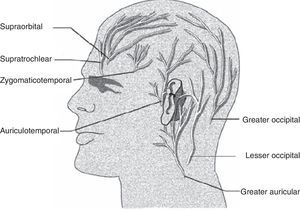
It was decided to perform bilateral regional scalp block with ropivacaine 0.75%, injecting 1.5ml into each of the points: supraorbital, supratrochlear, zygomaticotemporal and auriculotemporal; the greater and lesser occipital nerves; and 1.5ml of the same anaesthetic as reinforcement for the puncture sites where the spikes were placed to secure the Mayfield head holder. Dexmedetomidine infusion was started at 0.3μg/kg/h; 15min later, propofol and sufentanil infusions were started at target plasma concentrations of 1μg/ml and 0.0002mg/ml respectively. Ketorolac 60mg and ceftriaxone 1g were injected intravenously. At 90min, the surgeon injected the surgical incision site with 5ml of lidocaine/epinephrine 20mg/0.005mg/ml and 10min later, the surgical procedure was begun. At that point, the dexmedetomidine 0.3μg/kg/h infusion continued and the target plasma concentrations of propofol and sufentanil remained at 1.3μg/ml and 0.0002μg/ml respectively, with no significant changes in haemodynamic variables and maintaining a BIS ranging from 64 to 54.
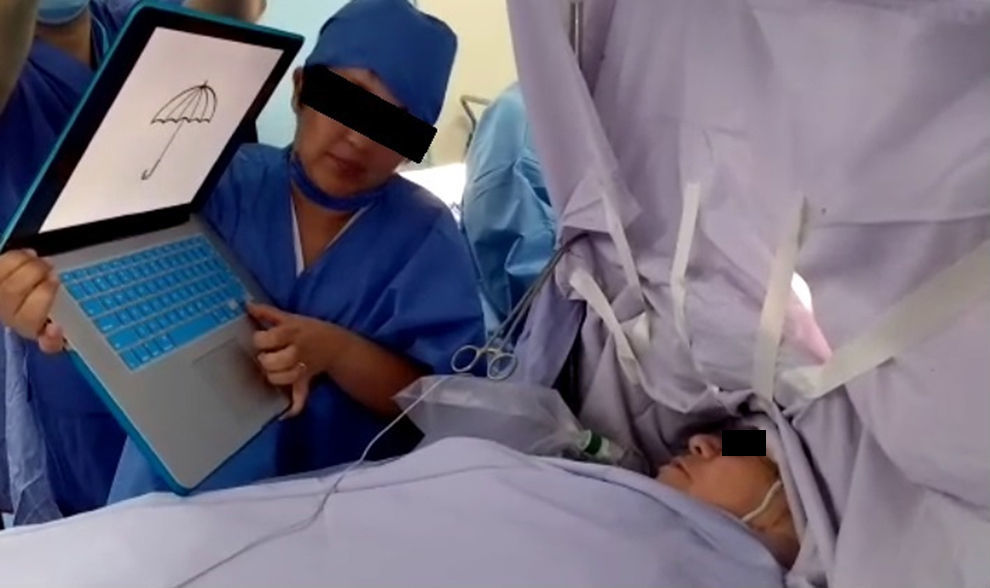
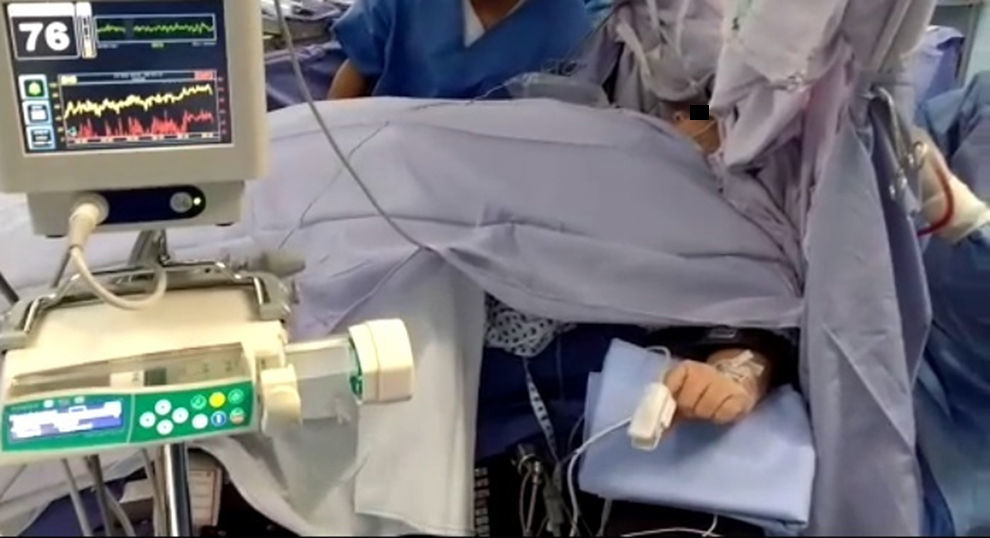
Prior to opening the dura mater, the surgeon decided to inject 100mg simple lidocaine at the base of the middle meningeal artery. At 120min, the three infusions were discontinued and gradually, over the following 15min, BIS was observed to return to values ranging from 89 to 74 (see Image 2); 20min after stopping the infusions, the patient was calm, cooperative and suitably understanding instructions, so the surgeon proceeded to perform cortical stimulation in areas adjacent to the tumour while the neuropsychologist conducted several tests of language with the patient; instances of dysarthria, paraphasia, counting errors, speech arrest or involuntary movements were discussed with the neurosurgeon (see Images 3 and 4). Once the language area had been identified, the neurosurgeon resected the tumour and carried out haemostasis. The patient remained awake for 50min. She had no intra-anaesthetic complications and did not develop any neurological deficits following the resection. The surgical pathology report stated intermediate-stage astrocytoma (WHO grade II).
DiscussionAll anaesthetic techniques for managing awake craniotomy are designed to allow resection and/or neurological functional mapping with greater protection of areas of the brain that control both motor function and speech.4,8 The techniques published in the literature vary from local anaesthetic with or without intravenous sedation to intermittent general anaesthesia with or without instrumentation of the airway, known as awake–awake–awake, asleep–awake–awake and asleep–awake–asleep craniotomy.9–11 In our case, we opted for local anaesthetic and intermittent intravenous sedation for an asleep–awake–asleep approach.
The challenge for the anaesthetist is to provide sedation, anxiolysis and optimal analgesia during preparation and brain exposure, and immobility, comfort and a maximum level of alertness for mapping and tumour resection, while also keeping hypoxaemia, hypercapnia, nausea, vomiting, seizures and haemodynamic instability to a minimum.4,9,12 As with any other craniotomy, optimum operative conditions are required in terms of surgical exposure and relaxation of the brain mass.13
Costello states that evaluation by a neurophysiologist is the gold standard for assessing patient responses during brain mapping.8 In our case, a neuropsychologist was present throughout the procedure and was responsible for conducting all the tests with the awake patient.
Scalp block is key in awake-patient techniques as it blocks sensory branches of the trigeminal nerve and occipital nerves (see Image 5).14–16 The anaesthetics most commonly used for this purpose are ropivacaine, lidocaine and bupivacaine, supplemented or not with epinephrine.15 The scalp block provides adequate postoperative analgesia and reduces opioid consumption, in addition to being prophylactic in the event of peripheral stimulation of the trigeminal cardiac reflex.9,14,17 In our case, we used ropivacaine for its prolonged effect and residual analgesia and lidocaine to reinforce some areas, taking advantage of its rapid onset of action with excellent results.
Numerous drug regimens have been described in different protocols, with the most used being propofol, remifentanil, dexmedetomidine and midazolam.18 Both dexmedetomidine and propofol allow early wake-up once the infusion is stopped because they have a short half-life, and this makes them the preferred drugs for performing awake craniotomy.19
The use of dexmedetomidine in craniotomy is widespread when intraoperative neurophysiological monitoring is required, in addition to being an attractive option because it does not cause respiratory depression.1,4,13,19 However, there are still unknowns in the field of cerebral haemodynamics in terms of the drug's bradycardia, hypotension and hypertension effects described extensively in the literature that directly affect cerebral blood flow, intracranial pressure, cerebral perfusion pressure and metabolic oxygen consumption.20 With our patient in particular, we can confirm the efficacy of dexmedetomidine, and we experienced no alterations to heart rate or blood pressure that might affect cerebral haemodynamics.
The bispectral index as part of monitoring for awake craniotomy has shown some utility for predicting full return to consciousness when preparing to perform brain mapping. Conte et al. conducted a prospective observational study on 27 patients which showed that the return to BIS equal to the pre-induction values seemed to indicate full return to consciousness.21 Our patient's BIS did return to baseline values and it was possible to perform cortical mapping with an appropriate level of consciousness. Nevertheless, further studies are necessary.
Awake craniotomy is now the preferred and most widely used method for functional neurosurgery.16 Intraoperative mapping with direct cortical stimulation is the gold standard for resection of brain lesions near eloquent areas and the motor cortex.15,22
Relative contraindications include an uncooperative patient, anxiety, deterioration in neurological status, psychiatric disorders, difficulty following orders, inability to concentrate, emotional instability, anticipated difficult airway, chronic obstructive pulmonary disease, obstructive sleep apnoea, obesity, gastro-oesophageal reflux and large brain tumours with midline shift. Contraindications inherent to the surgical procedure include estimated times of over 5h, the need to conduct multiple neurological tests and lateral and prone positioning.7,23 However, reports in the literature demonstrate the effectiveness of awake craniotomy managed with scalp block and dexmedetomidine in patients with contraindications such as obesity and tumours causing midline shift.7 The case we report here met the last two of the above relative criteria that contraindicate this technique, but the experience and skill of the surgeon allowed resection to be carried out without complications, with adequate cortical mapping and no new postoperative neurological deficits; similar cases have also been reported by Garavaglia et al.7
The main benefits of awake craniotomy are shorter hospital stay, reductions in hospital costs and perioperative morbidity, and improvement in postoperative functional status.1,24 Worth noting is the importance of a short hospital stay also in limiting nosocomial infections and thromboembolism.5
It has been shown that the incidence of permanent neurological deficits is lower among patients managed with awake craniotomy (4.6%) compared to general anaesthesia (16%), along with an improvement in both quality of life and survival, and decreased incidence of neurological deficits.5,9,24
The greater the extent of tumour resection, the lower the risk of tumour recurrence and the longer overall survival. Total resection has been reported in up to 78% of patients treated by awake craniotomy and neurophysiological monitoring.18
The main complications are late awakening, seizures, airway obstruction, hypoxia post-extubation, acute and chronic pain, nausea and vomiting.3 However the choice of anaesthetic technique also has an influence on the incidence of complications, as they are three times more common in patients managed with general anaesthesia.4 In our case, the patient did not suffer any complications.
ConclusionAwake craniotomy is a procedure widely used under different anaesthetic techniques.1,4,9,11 Scalp block is essential for adequate analgesia and different local anaesthetics can be used.14–16
A wide range of intravenous agents is reported in the literature, but the most commonly used are dexmedetomidine, propofol and ultra-short-acting opioids.18,19
The main indication for awake craniotomy is the need for neurophysiological monitoring for location of the tumour and resection of lesions in or near eloquent areas. Intraoperative evaluation in the awake patient is the gold standard for adequate assessment.4,8,16
There are few contraindications to awake craniotomy and the potential complications are those inherent to the craniotomy itself. The main benefits are for the patient, as it makes increased tumour resection possible, with better neurological outcome, in addition to lower costs for the patient and the institution.1,5,7,23
This article provides specialists with a report on a successfully managed case of awake craniotomy, as well as information that may aid decision-making in other similar cases.
Ethical disclosureProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
FundingNo funding was received for this study.
Conflict of interestThe authors declare that there are no potential conflicts of interest in relation to the article.
To Dr María Cristina Navarro Meza and Dr Rodrigo Ramos Zúñiga for their critical review of the text and technical comments on this article, and for their contributions to the manuscript. And especially to Dr José Lepe Mancilla, both for his encouragement and for being able to count on his support for carrying out this project.