Cecal appendagitis or cecal epiploic appendicitis is produced by torsion or thrombosis of a vascular pedicle of an epiploic appendix; it presents itself as pain in the right iliac fossa, simulating an acute appendicitis; having a self-limiting course with spontaneous resolution within 2 weeks. It does not require surgery, but only treatment with painkillers.
We report the case of a male patient who came to the emergency room with pain in the right iliac fossa; without improvement of symptoms, he underwent surgery resulting with cecal appendagitis, his treatment and subsequent evolution.
La apendagitis cecal o apendicitis epiploica cecal se produce por la torsión o trombosis del pedículo vascular de un apéndice epiploico. Se presenta como dolor en fosa iliaca derecha, simulando un cuadro de apendicitis y tiene un curso autolimitado con resolución espontánea en 2 semanas. El tratamiento es a base de analgésicos sin requerir cirugía.
Se presenta el caso de un paciente masculino con dolor persistente en fosa iliaca derecha, intervenido quirúrgicamente y con reporte histopatológico de apendicitis epiploica cecal.
The epiploic appendages were described anatomically by Vesalius in 1543, Virchow in 1843 describes surgical involvement, Lynn in 1956 first used the term cecal appendicitis and until 1986, when Danielson describes the radiological characteristics.1,2
The epiploic appendages are adipose structures that rise in the serosal surface of the colon and project into the abdominal cavity. They develop in the second trimester of fetal life and grow during adulthood, reaching a length of 0.5cm to 15cm and 2cm thick, located along the sigmoid colon 57%, ileocecal 26%, ascending colon 9%, transverse colon 6% and descending colon 2%.3,4 Correspond to between 50 and 100 pedunculated structures, practically nonexistent in the rectum, aligned in two separate rows, a medial to the taeniae and other lateral to the taeniae. Pedicle of each epiploic appendix contains one or two small end arteries, branches of the vasa recta and a small draining vein.
Limited blood flow of the epiploic appendages, excessive mobility and pediculated morphology make them susceptible to torsion with hemorrhagic or ischemic. Obesity and overweight are also risk factors because they increase the epiploic appendages both in number and measure; large meals, the same way, predispose to thrombosis draining vein due to splanchnic venous ectasia.4,5
Clinical caseThe case is a 50 years old male, without any pathologic background in his medical records. His clinical picture begins 18h before with pain localized at right iliac fossa level, like a colic, mild intensity, intermittent, accompanied by nausea, without vomiting, denies fever, denies urinary symptoms and diarrheal evacuations. Physical exploration: blood pressure 110/80mmHg, heart rate 85 per minutes, breathing frequency 18 per minutes and temperature 36.5. Abdomen with decreased peristalsis, tympanic to percussion, with discreet resistance at right iliac fossa level, signs Mcburney and Rosving negative, without plastrons were noted. Laboratory results revealed leukocytes 18.29/mm3, neutrophils 72.7%, red cells 14.98g/dl, platelets 233/mm3, PT 11.4, PTT 31.5, Na 137, Cl 100, K 4.0, glucose 78mg/dl, urea 25mg/dl, and creatinine 0.5mg/dl. Images are reporting lack of acute appendicitis (Figs. 1 and 2).
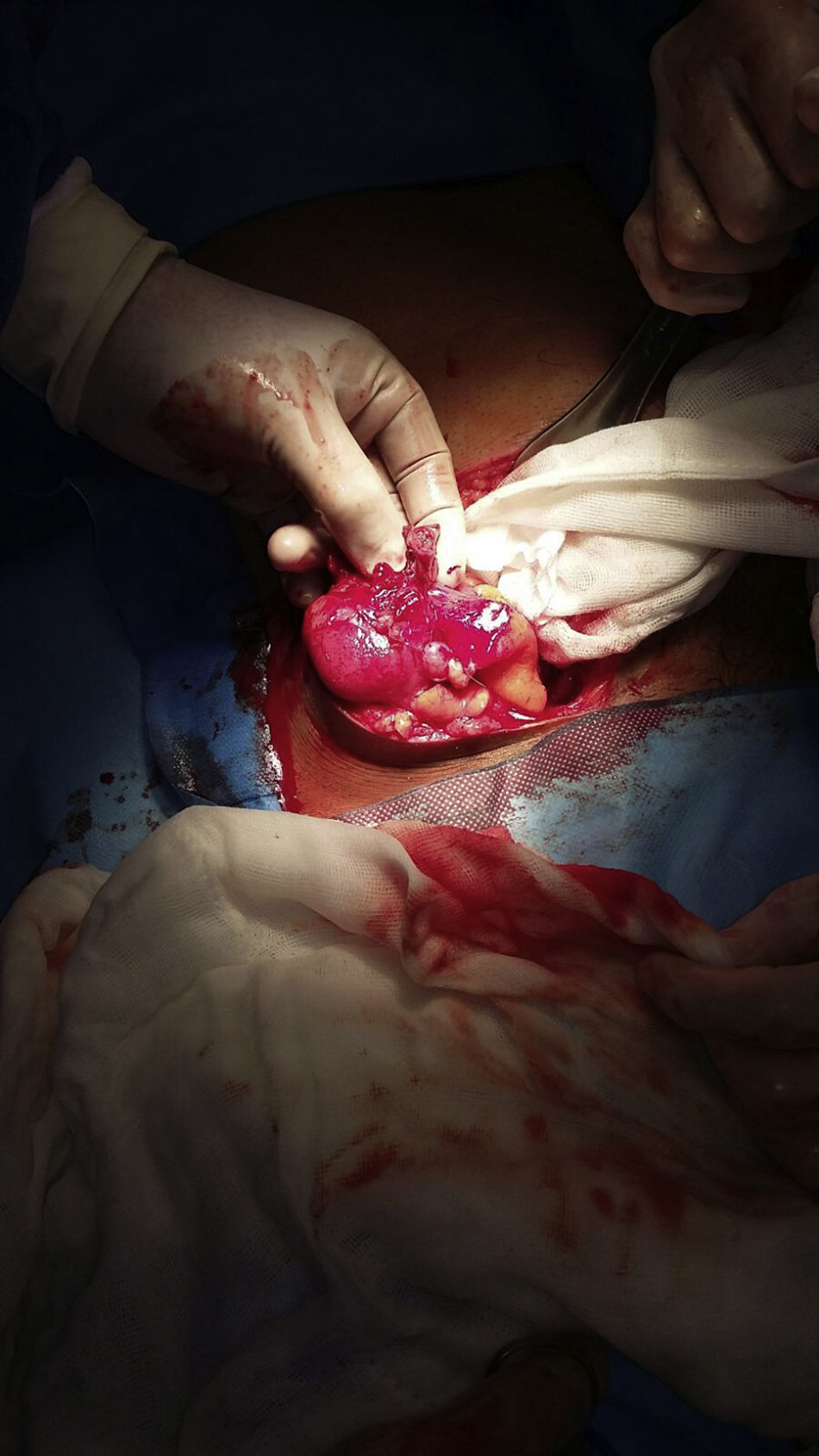
Following the patient evolution, it is decided to treat surgically, a type of McBurney incision was being performed, and were followed the dissection planes to abdominal cavity identifying low reaction liquid, cecal appendix without compromise, with healthy basis, and finding in the antimesenteric region an epipploic appendix twisted and gangrenous (Fig. 3). It is performed right hemicolectomy, with ileocolic terminolateral anastomosis. It faces by planes. 5 days after the surgical event, the patient presents tolerance to oral route, with normal evacuations; he was discharged with medical service. Histopathology report confirmed cecal appendagitis.
DiscussionAppendagitis is a relatively rare condition, and it occurs in 1.1% of patients with acute abdominal pain. It manifests as pain in the left iliac fossa in 80% of cases, to the right of the abdominal cavity in 14% and diffusely 6%.5 The incidence is noted in 3–7% in patients with suspected acute diverticulitis and 1% in patients with pain in the right iliac fossa; and according to the experience of Macari et al., it is a condition that occurs very rarely in the blind.7
The diagnosis of appendagitis, based on clinical signs and symptoms of the disease is not specific, which affects only 2.5% of the preoperative diagnoses are correct.8 Suspecting this diagnosis in patients with clinical signs and symptoms of acute appendicitis, which occurs with an incidence of 9.3 per 10,0009; or history of appendectomy, in which case it must be considered as differential diagnosis, recurrent appendicitis, which occurs in 1 in 50,000.10
Motta-Ramirez, in his studio in Mexico City, reported appendagitis 62% in male gender, between the second and fifth decade of life5; Rashid et al. in their study observed that it is very rare in patients less than 19 years old.11 It usually occurs without pain migration or peritoneal reaction. The presence of nausea, vomiting and diarrhea is uncommon. 10–30% of patients have a palpable mass and 25% have fever and leukocytosis.2–4,12
Differential diagnoses besides the cecal appendicitis, Meckel diverticulitis and omental infarction. While the cecal appendicitis and Meckel diverticulitis require surgical treatment; cecal appendagitis and omental infarction are self-limiting processes, which can be resolved with medical treatment and observation.6,13
Under normal conditions, epiploic appendages are not displayed, but are only displayed if they are swollen or ascites, hemoperitoneum or later in the intra-abdominal injection of contrast.5 On ultrasonography, it appears as a hyperechoic mass oval, lobed, incompressible, surrounded by a hypoechoic peripheral ring in 60% of cases, with increased echogenicity of the surrounding fat and no flow central.4 The CT scan is the gold standard to identify appendagitis.1 On CT, the infarcted epiploic appendix is presented as a focal area, oval, 1–4cm small, pericolonic, with fat density −40 to −120units Hounsfield, usually surrounded by a thin, fine dense ring, which represents the visceral peritoneum lining the eppiploic appendix. Less commonly, it can be identified within the lesion, one dense, ill-defined, rounded or linear area corresponding to the central thrombosed vessels or areas of hemorrhage or fibrosis.1 Magnetic resonance reveals data of focal lesions with hypointense images corresponding to fat, shown as a ring. This is an excellent method, but is limited by its cost and limited availability in Mexico.14 These radiographic changes may take up to six months to disappear.15
Surgeons and radiologists should be aware of this rare self-limiting disease and considered in the differential diagnosis of pain in the right iliac fossa, and should not ignore it, because there have been cases of confirmed appendicitis by the US and CT resulting in appendagitis.3,16 At the same time can be considered sometimes a disease underdiagnosed due to selective use, and no systematic imaging tests that make many patients remain labeled with nonspecific abdominal pain prior to surgery or medical treatment.2
With the use of laparoscopy, the diagnosis of cecal appendagitis is more likely. There have been reported cases of acute appendicitis a week after the laparoscopic treatment of a twisted appendagitis. Both pathologies were histologically confirmed.17,18
The treatment was initially surgical; it was until the year 1968 when conservative treatment was proposed by Epstein and Lempke.2 Currently the treatment is ambulatory with anti-inflammatory drugs, and there is no difference in evolution between those who receive or not antibiotic therapy.4,15 Spontaneous resolution of the symptoms occurs in 1–2 weeks. However, it has been reported persistent pain up to 40%.2,3
The wrong diagnosis can lead to surgery, medical treatment and hospitalization unjustified. Complications are rare: adherence to other viscera causing obstruction or abscess formation.4,15
Earlier, few cases of cecal appendagitis or cecal epiploic appendicitis have been published. The low frequency explains that rarely suspected this entity, so that his diagnosis is usually done during a surgical intervention. It is not uncommon for the clinician think in acute appendicitis in cases of cecal appendagitis.4,14
Even though the appendagitis is an infrequent cause of abdominal pain, we conclude that it is a relevant knowledge for the physician to avoid diagnostic and therapeutic errors that could increase unnecessary forms of morbidity, or the inadequate use of antibiotics and of hospitable resources.4
Ethical disclosureProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors declare that they have no conflict of interests.