The insufflation pressure of tracheal tubes is usually determined by the finger-pressure technique has low precision. The minimum leak technique is an alternative to determine whether the cuff is occluding the trachea with safe pressures (20-30cm of H2O). Our group previously described that 43% of intubated patients had excessive cuff pressures (> 30cm of H2O) when the finger-pressure technique was used.
ObjectiveTo compare the finger-pressure and minimum leak techniques to achieve safe intracuff pressures in patients undergoing endotracheal intubation. Data was analyzed with t-student and lineal regression.
MethodsAdult surgical patients requiring intubation were randomized in two groups in which cuff insufflation was checked by either the finger-pressure or minimum leak technique. After insufflation, the intracuff pressure was measured using an aneroid manometer. Data analysis was performed to evaluate variables that may affect performance.
ResultOur study included 286 patients (216 female) with a mean age of 44.6 SE±14.9 years. The mean insufflation pressures differed significantly between groups (finger-pressure, 36.9 SE±1.9cm H2O; minimum leak, 25.3 SE±1.4cm H2O; P<0.0001). Each group had 35% of patients with pressures within safe limits. Using finger-pressure, 46% of patient had excessive pressures (>30cm H2O). Using minimum leak technique, 42% of patients had insufficient pressures (<20cm H2O). We found a consistent association between the intracuff pressure and the body mass index (r2=0.223, P<0.0001).
ConclusionsFinger-pressure insufflation technique gave mean pressures 11cm H2O higher than the minimum leak technique but no replace to aneroid manometer.
La presión de insuflación usualmente se determina por la técnica de digitopresión. Una alternativa es la técnica de escape mínimo que consiste en insuflar el neumotaponamiento hasta escuchar sobre la laringe una fuga mínima de aire. Esta presión se mide objetivamente con un manómetro especial diseñado solo para esta función. Es importante determinar si la técnica de escape mínimo ofrece ventajas sobre la otra cuando no contamos con manómetro y mantener así la presión de insuflación en rangos de sguridad (20–30cm de H2O).
ObjetivoMedir la presión de insuflación con un manómetro en pacientes intubados, comparando la técnica de escape mínimo contra la de digitopresión en pacientes sometidos a intubación.
Material y métodosPacientes quirúrgicos adultos sometidos a intubación fueron aleatorizados en dos grupos. Se compararon las medias de presión de insuflación del neumotaponador mediante el manómetro anaéroide y las complicaciones en pacientes intubados con las técnicas de digitopresión o escape mínimo, el análisis estadístico se realizó con estadística descriptiva, t de Student y regresión lineal. Resultados: Se incluyeron 286 pacientes, 216 femeninos (75.5%), media de la edad 44.6 EE±14.9 años, 48.6% en el grupo de escape mímo y 51.4% en el de digitopresión. La media de la presión de insuflación en cm de H2O fue mayor en la técnica de digitopresión (36.9 EE±1.9) con respecto a la de escape mínimo (25.34 EE±1.4) (p<0.001). La presión de insuflación estuvo en límites seguros en el 35% de los casos. Encontramos una correlación consistente entre la presión del manguito y el IMC (r2=.0223 p<0.0001).
ConclusionesLa técnica de digitopresión da en promedio 11cm de H2O mas que la técnica de escape mínimo pero no sustituye al manómetro.
Endotracheal intubation is a common procedure in anesthesiology and intensive care departments. Two principal functions of endotracheal tubes are to keep the airway secured and to administer inhalational anesthetic gases.1–3 It is therefore necessary to achieve an adequate seal of airway with the endotracheal cuff.4,5 Excessive cuff pressure has been reported as a complication of endotracheal intubation leading to ischemia, necrosis, stenosis, paralysis of the recurrent laryngeal nerve, and tracheoesophageal fistula.6–11
A linear correlation has been observed between pressures higher than 30cm H2O and decrement tracheal irrigation. Additionally, clinical trials and animal models have demonstrated the disappearance of capillary perfusion with pressures of 50cm H2O or higher.12–15
In 2008, we conducted a transversal study with 158 surgical patients who underwent endotracheal intubation. The results showed that only 28.4% of the patients had cuff pressures in safe ranges.16
Usually, cuff pressure is assessed by a low precision finger-pressure technique in which the pilot balloon of the tracheal tube is palpated between the index finger and thumb. An alternative method to assess cuff pressure is the minimal leak technique which determines when the tracheal diameter is totally occluded during insufflation by listening through a stethoscope over the sternal notch.3–5 A more precise way to measure cuff pressure is by using a manometer designed specifically for this purpose (Cuff Pressure Gauge VBM CE 0123). However, this tool is not available in many medical centers, and it is not a frequent practice in operating rooms or intensive care units.
The main objective of this study was to compare the finger-pressure and minimum leak techniques to achieve safe intracuff pressures in surgical patients undergoing endotracheal intubation.
We performed a randomized, doble blind clinical trial approved by Ethical and Research Committees of Mexico General Hospital. The study population was comprised of all patients undergoing elective or emergency surgery in the Central Department of Surgery. Inclusion criteria allowed male and female patients with age ≥18 years with an indication of abdominal, chest, head, neck or orthopedic surgery. Exclusion criteria were ≥2 endotracheal intubation attempts or some other technical problem that would prevent this procedure. Patients were randomly assigned to perform either the finger-pressure or minimal leak technique.
A specific anesthesiologist conducted cuff pressure measurements within 10minutes after endotracheal intubation using a manometer (Cuff Pressure Gauge VBM CE 0123). In cases with the pressure out of a safe range, the pressure was immediately adjusted to 25cm H2O. ASA score, volume of air insufflated, type of surgical procedure, and anesthetic time were recorded. Side effects due to intubation were recorded during the first 24 postoperative hours. All data were stored and analyzed with Statistical Package for Social Science (SPSS V17.0). Difference in media cuff-pressure was assessed by Student t-test two tails. Difference in frequency of side effects was evaluated by Chi Square. Correlation between cuff-pressure and BMI was assessed by Pearson test.
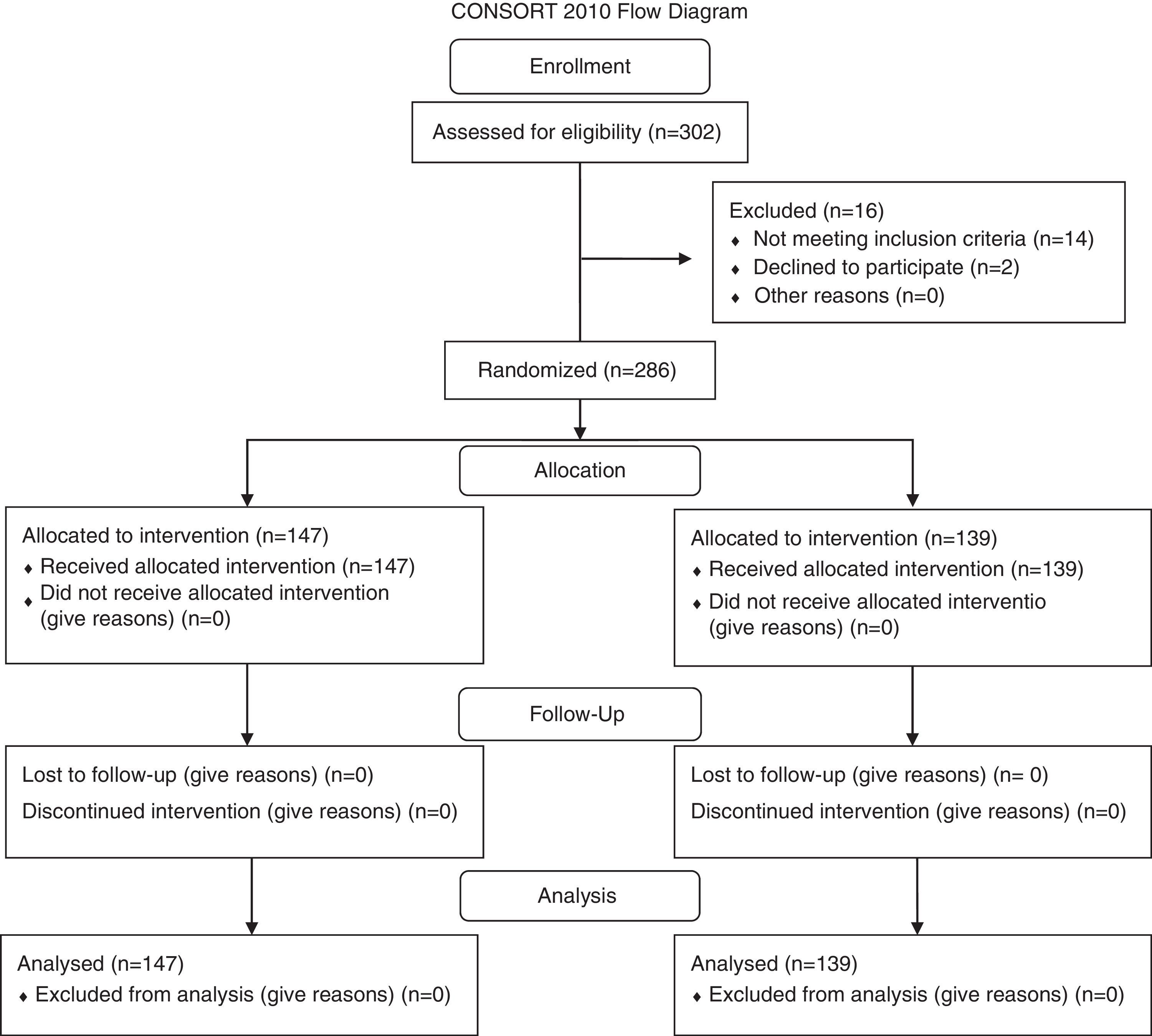
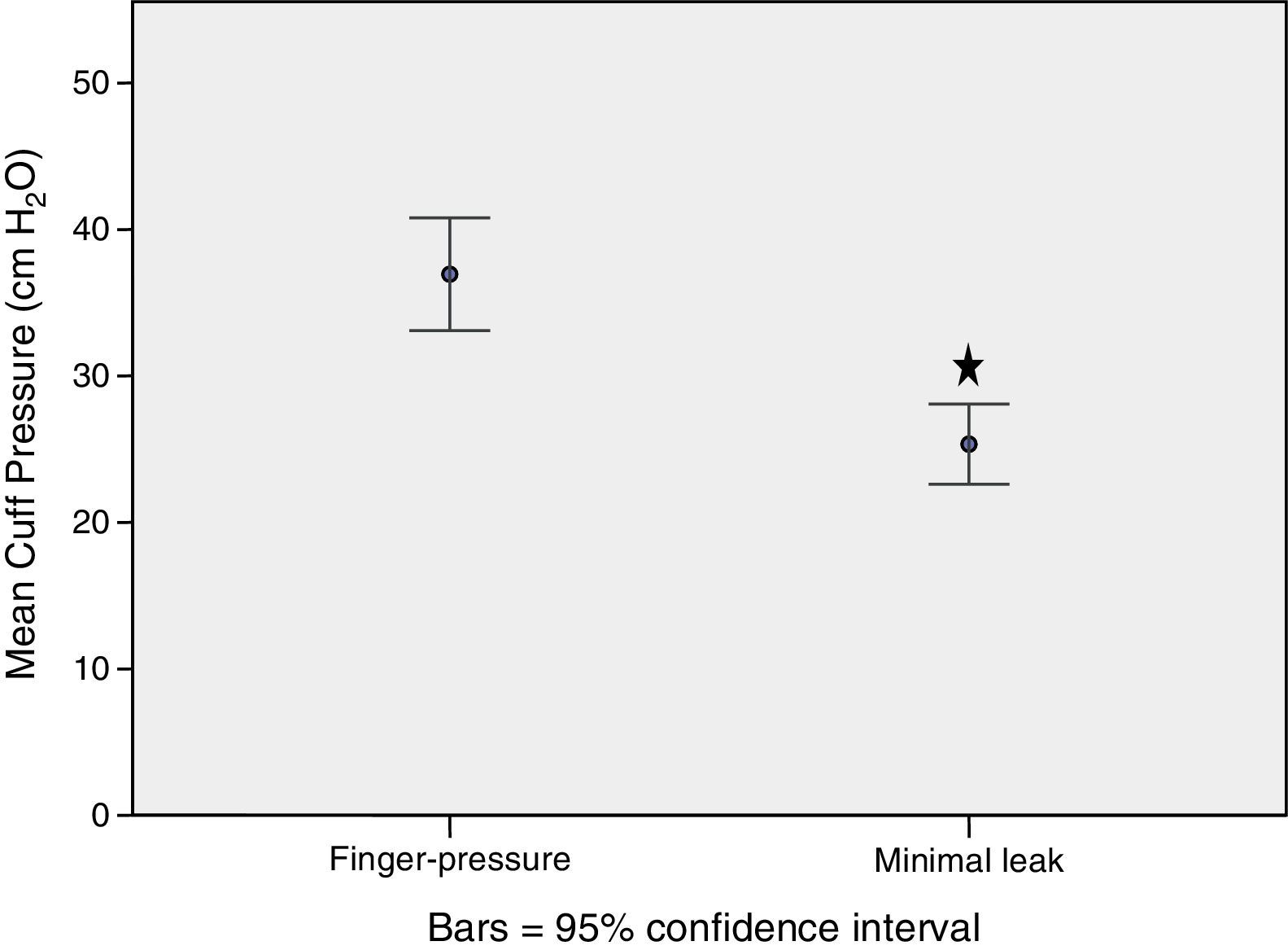
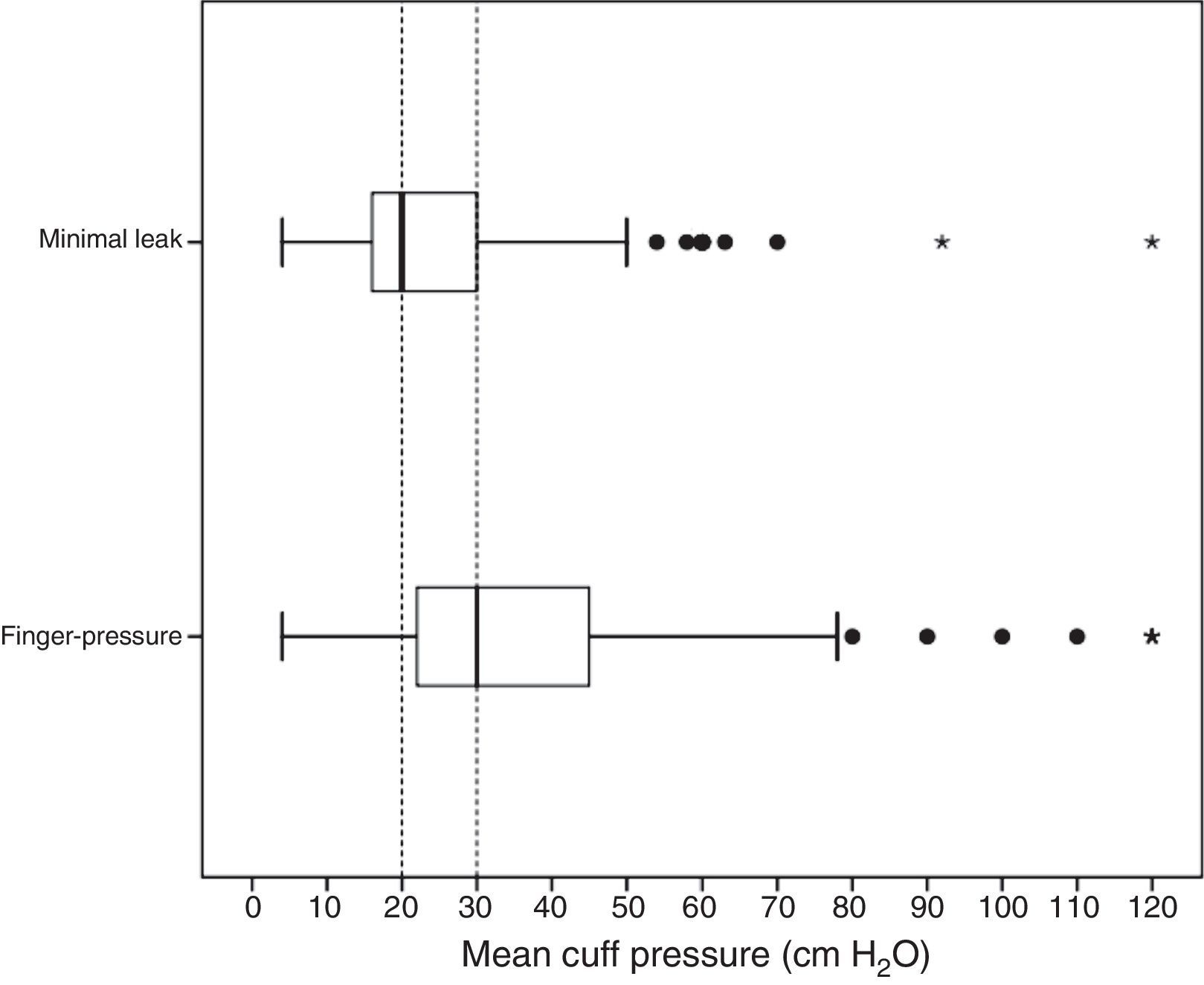
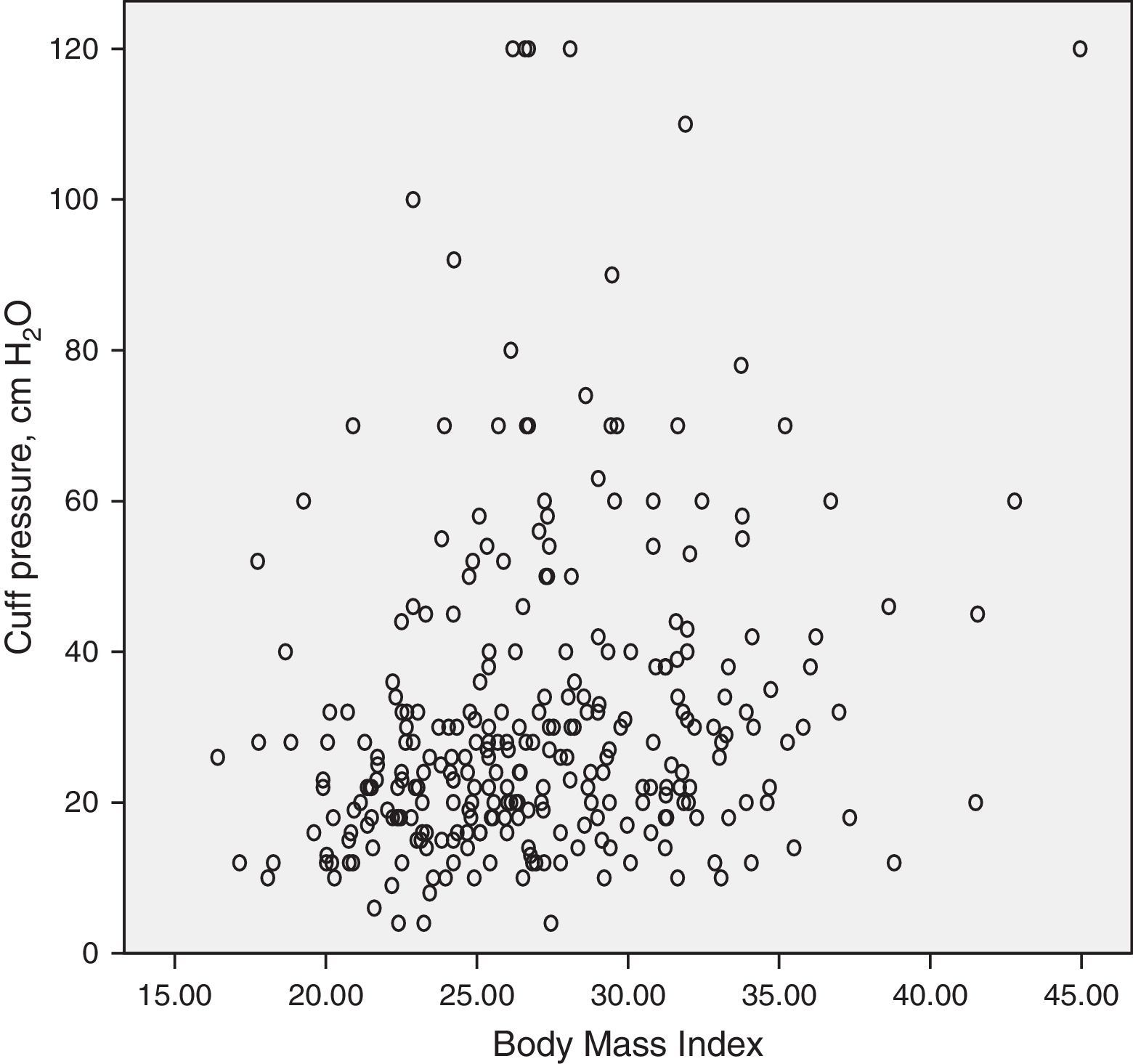
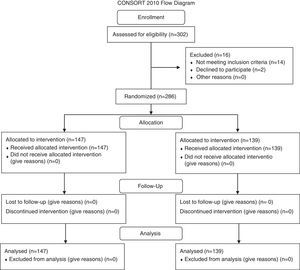
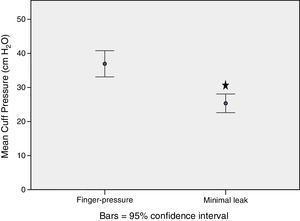
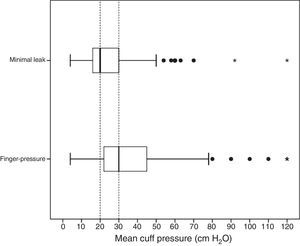
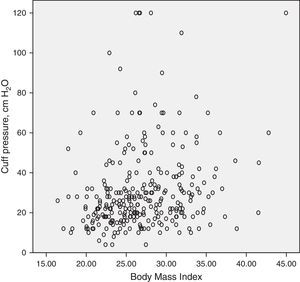
ResultsThe initial number of patients assessed for eligibility was 302; our study included 286 patients, of who 216 were female (Figure 1 shows Distribution of patients according CONSORT guidelines) (sample size was 143 patients for each group calculated by media difference with Z¿= 1.96 and Z¿= 0.84 and minimal difference between both techniques of 10cm H2O). Table 1 shows demographic data. Mean Body Mass Index (BMI) was 27.0kg/m2 (CI 95% 26.5-27.5). Stratifying by ASA score, 46.2% patients were Stage I, 44.1% were Stage II, and 9.8% were Stage III/IV. Figure 2 shows the difference between means of cuff pressure for finger-pressure (36.9cm H2O SE±1.9) versus minimal leak techniques (25.3cm H2O SE±1.4) (Non-statistical difference in distribution by Kolmogorov-Smirnov test). A significance difference was observed (Student t test two tails P<0.0001) with a difference of 11.6cm H2O (CI 95% 6.9-16.3) between groups. The proportions of patient with cuff pressures in a safe range (20-30cm H2O) were 35.4% for finger-pressure and 35.3% for minimal leak technique (Table 2). Therefore, 65% of patients did not have optimal cuff pressures. No significance correlations were found between cuff pressures and ASA stage, type of surgery, anesthesiologist or anesthetic time, but BMI showed a directly proportional relationship with cuff pressure, which was significant Figure 3 (Figure 4). Collateral effects were<10% for the total sample where are included respectively for finger-pressure or minimal leak cough (3.4% and 4.3%), dysphonia (18.4% and 2.9%) and odynophagia (13.6% and 2.9%).
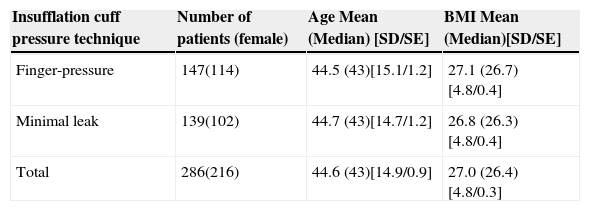
Demographic features. Age in years, BMI=Body Mass Index, SD=Standard deviation, SE=Standard error.
| Insufflation cuff pressure technique | Number of patients (female) | Age Mean (Median) [SD/SE] | BMI Mean (Median)[SD/SE] |
|---|---|---|---|
| Finger-pressure | 147(114) | 44.5 (43)[15.1/1.2] | 27.1 (26.7)[4.8/0.4] |
| Minimal leak | 139(102) | 44.7 (43)[14.7/1.2] | 26.8 (26.3)[4.8/0.4] |
| Total | 286(216) | 44.6 (43)[14.9/0.9] | 27.0 (26.4)[4.8/0.3] |
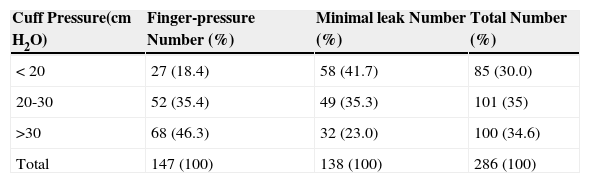
Thirty percent of patients had cuff pressures below 20cm H2O, and 34.6% had cuff pressures greater than 30cm H2O. ¿2=24.50, P<0.0001.
| Cuff Pressure(cm H2O) | Finger-pressure Number (%) | Minimal leak Number (%) | Total Number (%) |
|---|---|---|---|
| < 20 | 27 (18.4) | 58 (41.7) | 85 (30.0) |
| 20-30 | 52 (35.4) | 49 (35.3) | 101 (35) |
| >30 | 68 (46.3) | 32 (23.0) | 100 (34.6) |
| Total | 147 (100) | 138 (100) | 286 (100) |
Box plot graphic shows inter-quartile distribution for minimal leak and finger-pressure. Median for finger-pressure=30cm H2O. Median for minimal leak=20cm H2O.=Internal out layers. *=External out layers. When external out layers were eliminated for specific analysis statistical significance was similarly significant.
The main objective of this study was to assess insufflation cuff pressures by two different techniques and to determine if one technique could be recommended over the other for maintaining cuff pressures from 20 to 30cm H2O.
This study showed a substantial and significant difference between cuff pressures resulting from the finger-pressure (36.9cm H2O±23.6) versus the minimal leak technique (25.3cm H2O±16.3) (delta=11.6cm H2O, P<0.0001). Based on these results, the minimal leak technique could be better to achieve the correct pressure at beginning of surgery. However, only 35.3% of patients in the minimal leak group had pressures within the optimal safe range, while 41.7% of minimal leak group had cuff pressures less than 20cm H2O and 23% had cuff pressures higher than 30cm H2O.
We also found that confounding factors, such as ASA stage, type of surgery, anesthesiologist or anesthetic time, did not correlate with the measured pressures. However, BMI was a factor that directly correlated with higher cuff pressures (P<0.0001), and BMI is not usually taken into account. So, the linear correlation showed a r2=0.223 P<0.0001 (n=286). This finding could be a predictor factor of complications in intubated patients. A significant r2=0.223 cold be explained by partial reduction of air ways in patients with overweight.
Several authors have reported that cuff pressures higher than 30cm H2O can induce paralysis of the tracheal epithelial cilia and lead to tissue ischemia. Additional pathological states could be caused, such as edema, ulceration and even infectious processes. Infection is promoted by the leakage of secretions through the damaged tissue.17–20 Fibrosis and tracheal stenosis have been reported as late complications.21–28 Even with the high frequency of complications that result when cuff pressures are out of optimal range, the frequency is probably underestimated because anti-inflammatory and antibiotics, which may mask these disorders, are usually administered during the anesthetic procedure.29–33 When endotracheal intubation is prolonged for days or weeks, such as for patients in intensive care units, complications from the intubation are even more likely.14,22,24,25
The diagnosis of tracheal stenosis is often delayed because only 70% of tracheal obstructions become symptomatic.26 High cuff pressure can also damage pressure receptors within the tracheal mucosa, but the clinical implications of this damage on chronic cough and other long-term pulmonary disorders needs further study.34
Recurrent laryngeal nerve damage is actually less frequent now compared to the 1970s when low volume-high pressure cuffs were used and exerted irregular pressure on the tracheal wall and compressed the nerve.24
On the other hand, insufficient cuff pressure allows retrograde leakage during positive pressure ventilation which leads to inadequate ventilation of the patient, increased consumption of anesthetic gases, and environmental contamination. Also, improperly inflated cuffs increase the risk of aspiration of secretions to the bronchial tree.17–20
Even though several reports have shown that only manometry with a cuff pressure gauge effectively achieves optimal cuff pressures, these devices are not being used enough in clinical practice. This circumstance is probably due to insufficient availability of manometers and excess of physician confidence in usual insufflation techniques.35–39
Recently, automated controllers have been designed to monitor and keep the cuff pressures within the optimal range.40,41 Particularly in developing countries, access to manometers or controllers is more difficult. So without manometers being readily available, it is important to assess which alternatives are best to keep cuff pressures in the optimal range. Nevertheless, the main conclusion is to realize the need to more widely use manometers or better automated controllers during routine anesthetic procedures.