Bone marrow aspiration and bone marrow biopsy are invasive procedures in which good technical skill is crucial to obtain samples suitable for processing and diagnostic interpretation. The type and calibre of the needle is one of the main variables of the technique, and is selected on the basis of the age, gender and body mass of the patient. This article provides a practical, step-by-step guide to the technique for both procedures. It also discusses existing techniques for reducing the pain associated with the procedure, an essential aspect for the patient that if poorly handled, can force cancellation of the procedure.
La aspiración y biopsia de médula ósea son procedimientos invasivos en los que una buena técnica determinará la obtención de muestras idóneas para su procesamiento e interpretación diagnóstica. El tipo y calibre de la aguja es una de las principales variables de la técnica, debiendo elegirse en función de la edad, género y masa corporal del paciente. En este artículo se encontrará una guía práctica, paso a paso de la técnica para ambos procedimientos. Se mencionarán además las maniobras existentes para reducir el dolor asociado al procedimiento, aspecto fundamental para el paciente, y que en caso de no ser bien manejado puede obligar a la suspensión del procedimiento.
Trepanning is one of the oldest surgical operations known to man (of 120 prehistoric craniums dating from 6500 BC, 430 showed signs of trepanning). A trephine (from the Latin trypan) or auger is a cylindrical surgical instrument of varying size and shape. Trepans are specially designed to obtain cylindrical fragments of bone for analysis, or to drill through the cranium. The Roman physician Celsus practised trepanation, and recommended it as a remedy for headache. One of the earliest paintings depicting a medical procedure shows the New England physician John Clarke trepanning a cranium (Fig. 1). In the early years of the 20th century, the Italian physician Pianese made the first attempt to obtain a bone marrow sample for diagnosis by perforating the upper part of the epiphysis of the femur, obtaining a cylindrical specimen. The technique he used is very similar to that used today. Seyfarth, in 1922, developed a puncture needle for open biopsy of the sternum at a point between the 3rd and 4th ribs.
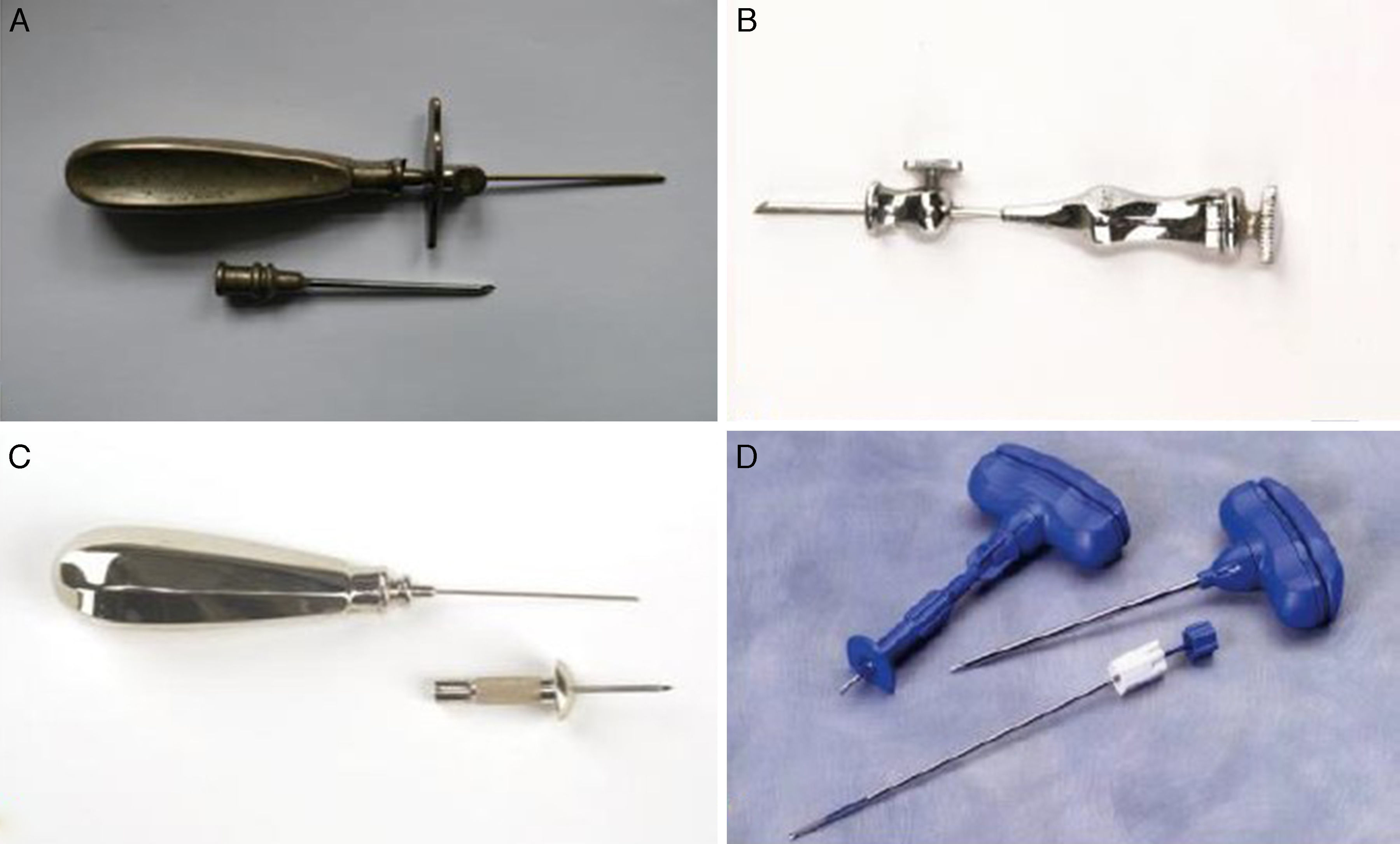
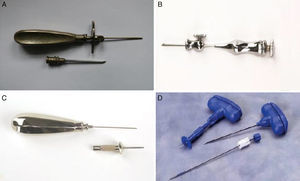
In 1927, Anirkin, a Russian physician, obtained bone marrow from the sternum using a lumbar puncture needle. Anirkin's technique was used not only for the analysis of bone marrow, but also for diagnosis of typhoid and tuberculosis. Arjeff (1931) introduced needles with a guard, and Grunke (1938) used a short lumbar puncture needle for marrow aspiration on the sternum with the help of a wooden mallet. The needles developed by Klima and Rosegger (1935) have guards (Fig. 2A). Henning and Korth (1934) suggested a cannula with a side opening to facilitate irrigation of the marrow cavity. During these early years, many physicians considered administration of local anaesthetic unnecessary. The first deaths following sternal punctures probably occurred between 1943 and 1944. The technique continued to improve throughout the 1940s and into the 1950s, when the pelvis was suggested as the collection site (Rubinstein 1950, Bierman 1952, Sacker and Nordin 1954). In response to a 5% failure rate in obtaining samples, McFarland and Dameshek (1958) described a trephination technique using the Vim-Silverman biopsy needle (Silverman, 1938). These biopsies were performed using local anaesthesia, and several modifications were made to the needle (1959–1963) (Fig. 2B and C). Up to this point, all biopsy procedures were performed in the outpatient setting. In 1971, Iranian haematologist Khosrow Jamshidi redesigned the needle so that the interior diameter of the distal portion was tapered, allowing tissue to freely enter the lumen without fracturing the core (Fig. 2D). Some early attempts at designing electric drills were made between the 1960s and 1980s. However, due to the ease of use, efficacy and low cost of hand-held needles, these electric devices were discontinued. Modern needles are similar in design to those used in the 20th century, and the procedure is carried out under local anaesthetic to minimise patient discomfort.1
Ideal size of bone marrow biopsy needlesBone marrow biopsy complements the study of bone marrow smear specimens obtained by aspiration, thus facilitating the diagnostic process. Diagnosis will depend on the size of the sample obtained. According to Wintrobe, the ideal sample size is 2.0cm.2 Bishop et al. at the Christie Hospital in Manchester, UK, evaluated the quality of 767 bone marrow trephines performed using 2 types of needles (the Jamshidi and the Islam). The average histology sample size was found to be 1.59cm, and 25% of the specimen was fractured and therefore not viable for the purpose of the study. The average, useful length of the biopsy specimen was 1.15cm (0.09cm soft tissue, 0.04cm of cortex, 0.26cm of disrupted marrow, and 0.74cm of interpretable marrow). The largest specimens were usually obtained using the Jamshidi needle.3
Bone marrow aspiration and bone marrow biopsy techniqueBone marrow aspiration has gained momentum due to the possibility of obtaining haematopoietic stem cells. These are useful not only in the treatment of haematological and non-haematological diseases, but also for the purpose of tissue reconstruction.4 The following describes the general technique used in sternal bone marrow aspiration. The technique used in iliac spine sampling is described in connection with bone marrow biopsy.
Sternal puncture- 1.
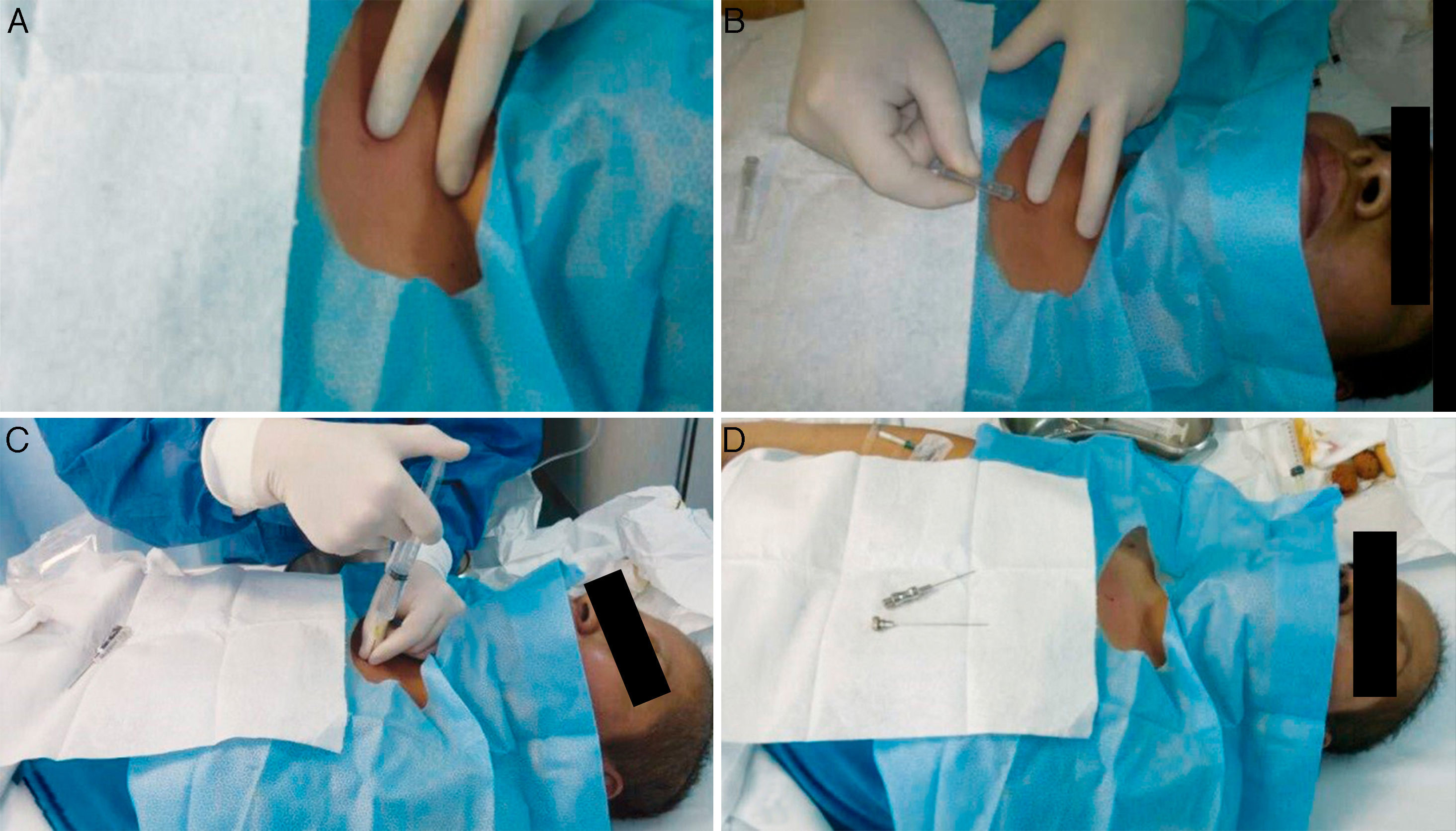
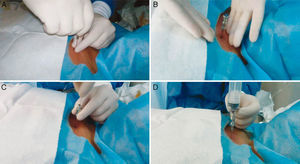
With the patient in the supine position, locate the sternal angle using gentle digital palpation. Use the needle cover to locate the intersection between the sternal angle and the midsternal line (Fig. 3A and B). To facilitate the procedure, ask the patient to extend their neck (Fig. 3C). Disinfect the area and cover it with a surgical aperture drape.
Figure 3.Sternal puncture. (A) Location of the sternal puncture site. The sternal angle, formed by the junction of the manubrium and the body of the sternum, lies 2cm below the sternal notch. (B) Gently mark the puncture site. (C) Inject 10ml lidocaine, initially at the level of the skin, and then in the periosteum. (D). Identify the parts of the Osgood needle before performing aspiration.
(0.5MB). - 2.
Administer local anaesthetic with 1% lidocaine, using 3ml to anaesthetise the skin and subcutaneous tissue. Then, gently inject lidocaine at various points on the cortical bone, administering 1ml anaesthetic with each injection.
- 3.
After a waiting time of between 3 and 5min, start the procedure. First, identify the parts of the bone marrow needle (Fig. 3D). Haematologists usually use size 16 and 18 needles.
- 4.
Insert the needle at the previously marked site, through the skin and subcutaneous tissue until it abuts the bone.
- 5.
Push the needle through the bony cortex, rotating it on its axis until it is fixed in place at the desired depth (Fig. 4A and B).
- 6.
Withdraw the stylet (Fig. 4C), attach a 20ml syringe, and aspirate gently (Fig. 4D).
- 7.
For a smear sample, aspirate only 1ml of fluid.
- 8.
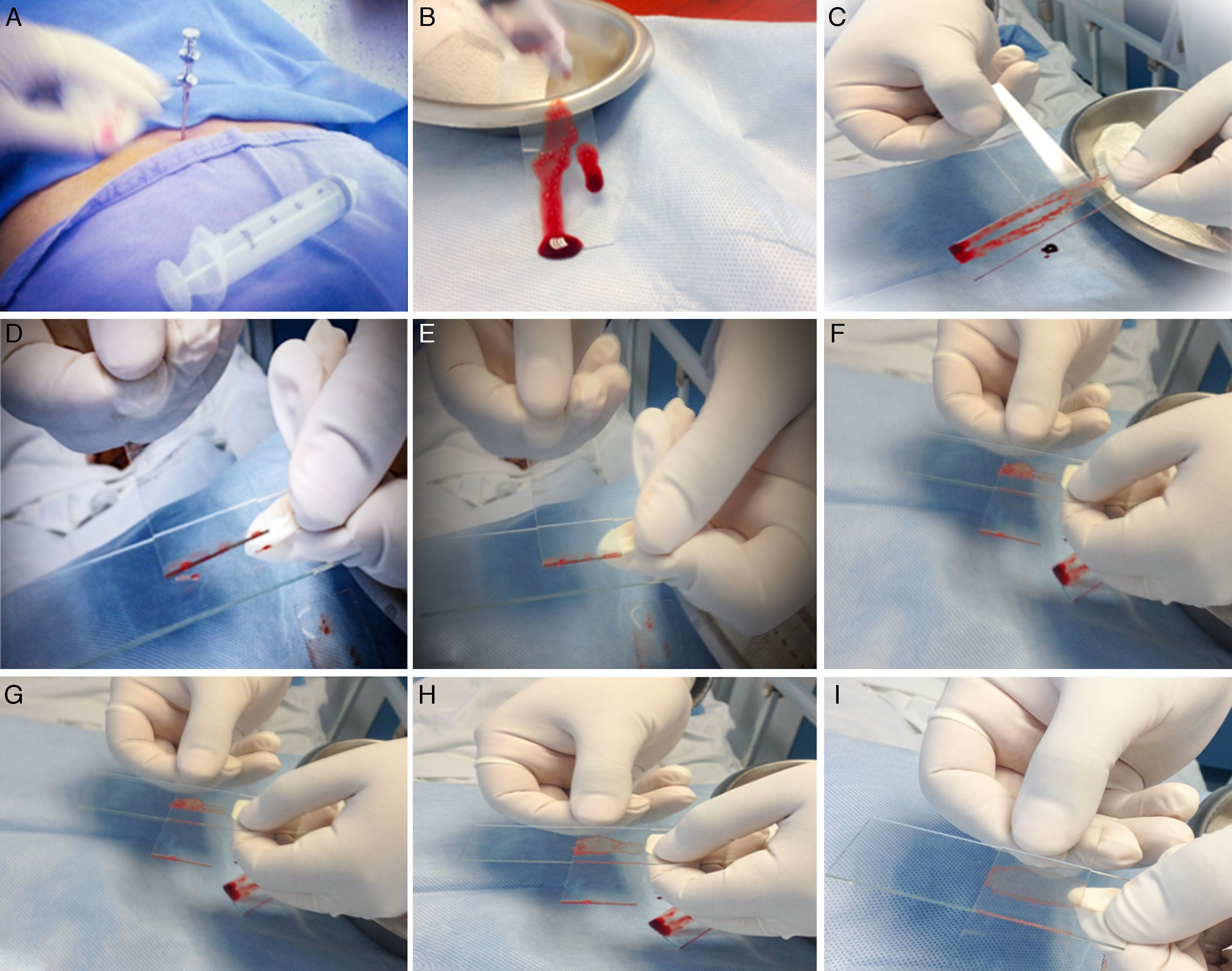
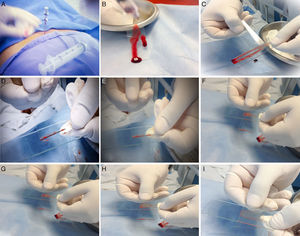
The smear technique used will usually vary from one hospital to another. Fig. 5 shows the steps involved to prepare the smear.
Figure 5.Preparing the bone marrow smear. (A) When the bone marrow aspiration needle is in place, use a 20ml syringe to draw 1ml of aspirate. (B) Place a few drops of aspirate on a slide held vertically to facilitate visualisation of the bone marrow spicules. (C) Using the edge of a second slide, separate and isolate a few bone marrow spicules from the rest of the sample. (D) Transfer these to a third slide. (E) Without applying pressure, distribute the spicules in the centre of the slide. (F) Place the second slide across the third slide to form a cross with the spicules in the centre. (G) Gently but quickly slide the second slide over the third slide to extend the spicules along its length. (H) Make sure the aspirate is spread evenly over the entire slide. (I) Allow to dry for 5min, and then send it to the lab for tincture.
(0.94MB). - 9.
Five smears are prepared, with each slide being appropriately identified.
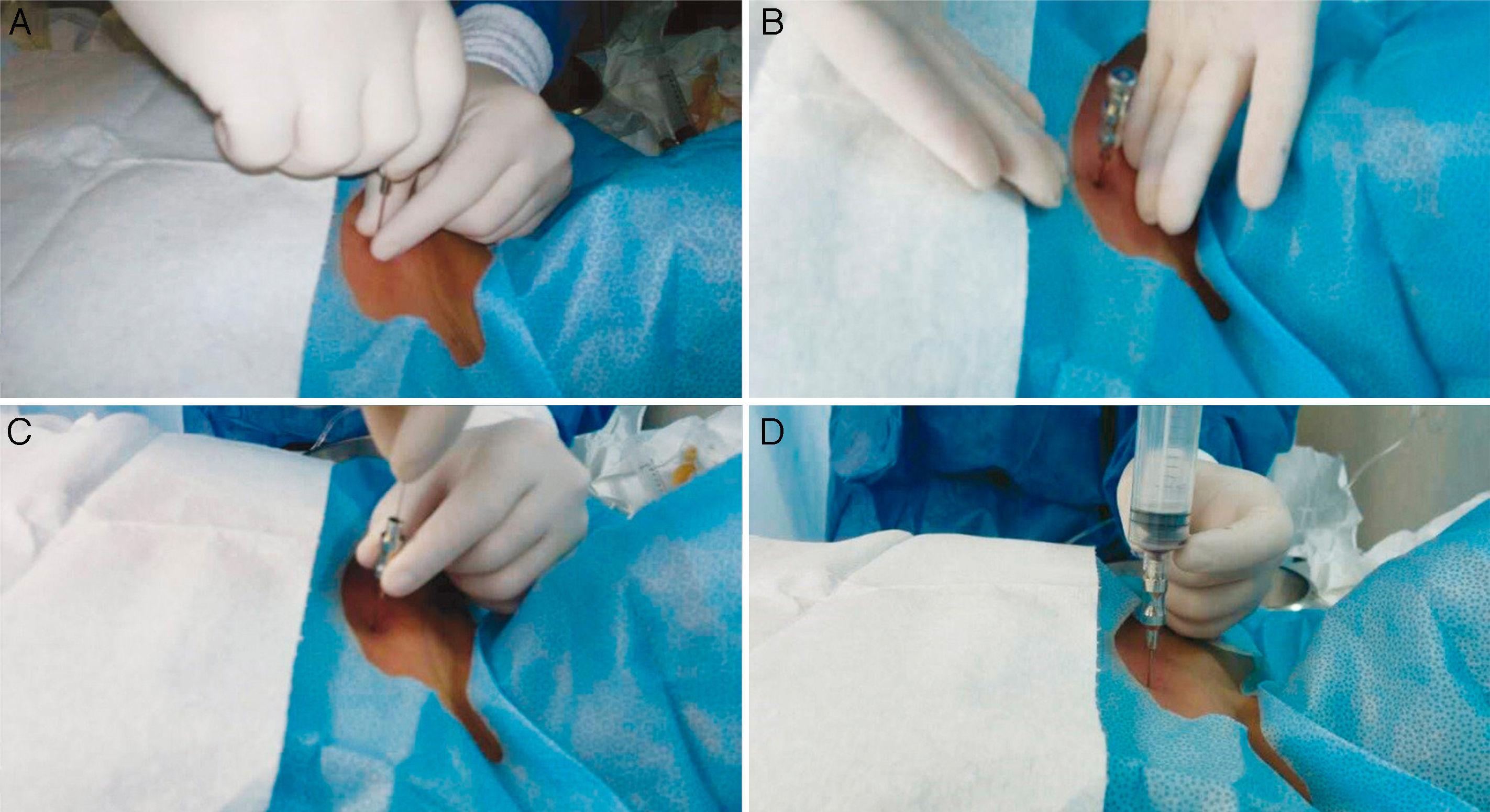
The best site for bone marrow biopsy is the posterior superior iliac spine. The biopsy is usually performed using a Jamshidi size 8–11 needle. The first step is to identify the parts of the needle, and then locate the sampling site.
- 1.
The biopsy can be collected from several different sites (anterior or posterosuperior). Mark the preferred sampling site.
- 2.
Administer anaesthesia as described for needle aspiration. When the trephine needle is assembled, it is inserted into the sampling site either directly, or after making a small (0.2cm) incision to facilitate access to the bone. The needle is pushed into the bone by rotating it on its axis.
- 3.
When the desired depth is reached, the stylet is withdrawn and the needle is advanced using the same rotating movement.
- 4.
The depth of the needle is measured using a stylet. A specimen measuring approximately 2cm in length should be collected.
- 5.
When the correct depth has been ascertained, the needle is rotated in the opposite direction to help loosen the specimen. The needle, with the specimen, is then withdrawn using a rotational movement.
Bone marrow aspiration is less sensitive than bone marrow biopsy (BMB) for detecting metastasis or lymphoid infiltration.5,6 Generally speaking, BMO does not give false positives, and is 100% consistent when performed bilaterally.7 The rate of positive diagnosis for lymphoid infiltration correlates with the length of the biopsy specimen (increasing by 35% in specimens measuring≥20mm).8 BMB is a blind sampling technique, and as such it is difficult to accurately determine the length of the specimen collected. Recently, Islam, in the Buffalo General Hospital (USA), published a study on the use of ultrasound to gauge BMB specimen size.9
Pain management strategiesNeedle aspiration and BMB are usually performed at the same time.10 Few studies have been published to date on pain management during the procedure. Park et al. evaluated the use of low-dose lorazepam in a double-blind, placebo controlled trial that measured pain on a visual analogue pain scale. Scores were similar for both lorazepam (6.0) and placebo (6.2), although patients in the lorazepam groups showed greater willingness to repeat the procedure (p=0.044).11 Recently, Kuivalainen et al. evaluated the use of sublingual fentanyl. They found no improvement over placebo, but observed a greater number of adverse effects.12 Other strategies have included nitrous oxide/oxygen (N2O/O2) administration prior to BMB, a low-cost, easily administered technique that can be used in the outpatient setting.13 Other factors that influence the sensation of pain are patient anxiety, gender, age, body mass index and level of education, along with adequate information given prior to the procedure, history of previous biopsy, extent of the operator's experience in the technique, and the duration and technical difficulty of the procedure.14 In our experience, the pain associated with the procedure has been reduced by a combination of factors: waiting for the lidocaine to take effect, continuous communication with the patient, and music therapy. Ultimately, however, bone marrow biopsy is still a painful procedure despite these strategies.
Main interpretation errors in bone marrow examinationAs mentioned above, specimen size is one the main problems encountered in the interpretation of bone marrow biopsy specimens. In the case of bone marrow aspirate, the main problem is the quality of the smear. Interpretation of a bone marrow smear will be unsafe if the sample is haemodiluted.15 The smear technique has been described in Fig. 5 above, and initially requires about 0.5ml of aspirate. The greater the volume collected, the higher the risk of a haemodiluted sample. Bone marrow smears must be performed immediately following collection; 5 or 6 smears are usually sufficient. If the smears cannot be prepared immediately, the aspirate should be placed into a tube containing ethylene diamine tetra-acetic acid (EDTA) at a concentration of 1.5±0.25mg/ml of blood. For immunophenotyping, karyotyping or molecular studies, sample collection should follow the recommendations of the respective laboratories.16
ConclusionsBoth bone marrow aspiration and BMB are essential for the diagnosis and follow-up of most blood disorders. Most interpretation problems are secondary to operator error. Further studies are needed to investigate effective pain management strategies for this procedure. Forums, such as www.painlessbiopsy.wordpress.com17 allow specialists in BMB and aspiration to pool their experience for the purpose of improving the quality and alleviate the pain associated with the procedure.
Conflict of interestThe authors declare that they have no conflict of interests.