Phlegmasia cerulea dolens is a severe form of deep vein thrombosis of the lower limbs. It consists of the clinical triad of limb oedema, acute ischaemic pain and cyanosis, leading to venous congestion with oedema, massive fluid sequestration causing circulatory collapse and shock as the cause of death.
Case reportFemale patient with deep vein thrombosis and development of phlegmasia cerulea dolens and pulmonary embolism.
DiscussionPhlegmasia cerulea dolens is a special form of deep vein thrombosis associated with proximal vein thrombosis, with signs of ischaemia. It should be suspected with the clinical symptoms of pain, oedema and cyanosis. Treatment includes: anticoagulation, thrombolysis and surgical thrombectomy; cases of acute haemodynamic ischaemias can require amputation of the limb.
La flegmasia cerúlea dolens es una forma severa de trombosis venosa profunda de los miembros inferiores. Consiste en la triada clínica de edema de la extremidad, dolor isquémico agudo, y cianosis, conduce a congestión venosa con edema, secuestro de líquido masivo ocasionando colapso circulatorio y choque como causa de muerte.
Presentación de casoPresentar el caso de un paciente femenino con trombosis venosa profunda y desarrollo de flegmasía cerúlea dolens y tromboembolia pulmonar.
DiscusiónLa flegmasia cerúlea dolens es una forma especial de trombosis venosa profunda asociada a una trombosis venosa proximal, con signos de isquemia. Clínicamente se debe sospechar con la triada de “dolor, edema y cianosis”. El tratamiento incluye: anticoagulación, trombolisis y trombectomía quirúrgica, en los casos de isquemia aguda con repercusión hemodinámica puede llegar a la amputación de la extremidad.
Thromboembolic disease comprises two conditions, deep vein thrombosis (DVT) and pulmonary thromboembolism (PTE).1 The two most devastating complications are pulmonary embolism and phlegmasia cerulea dolens. The former, in 90% of cases, originates in leg veins and the latter is a form of acute massive venous thrombosis that can lead to venous gangrene.2,3 There are no nationwide prevalence data, but Arrieta et al. report a prevalence rate of 4.6% in patients with iliofemoral vein thrombosis4 Most doctors have limited experience in the diagnosis and management of this disease.5
Case report46-year old female admitted to the Emergency Department, referring 24h of sudden onset, sharp pain in left leg, together with oedema, violet colouring, cyanosis, functional limitation, dyspnoea and chest pain.
The physical examination revealed tachypnoea, tachycardia, 80% oxygen saturation and wheezing in both lungs; the left leg was euthermic with oedema from the groin to the foot, with cyanosis, muscular stress in the entire leg, pain upon palpation, reduction in distal pulses (Fig. 1). Examination with linear Doppler ultrasound showed an absence of biphasic flows. In the Emergency Department, she evolved poorly with respiratory distress, due to which she was subjected to orotracheal intubation and the use of vasopressor amines owing to haemodynamic instability. The leg presented reduced temperature, absence of distal pulses and arterial flow and haemodynamic instability.
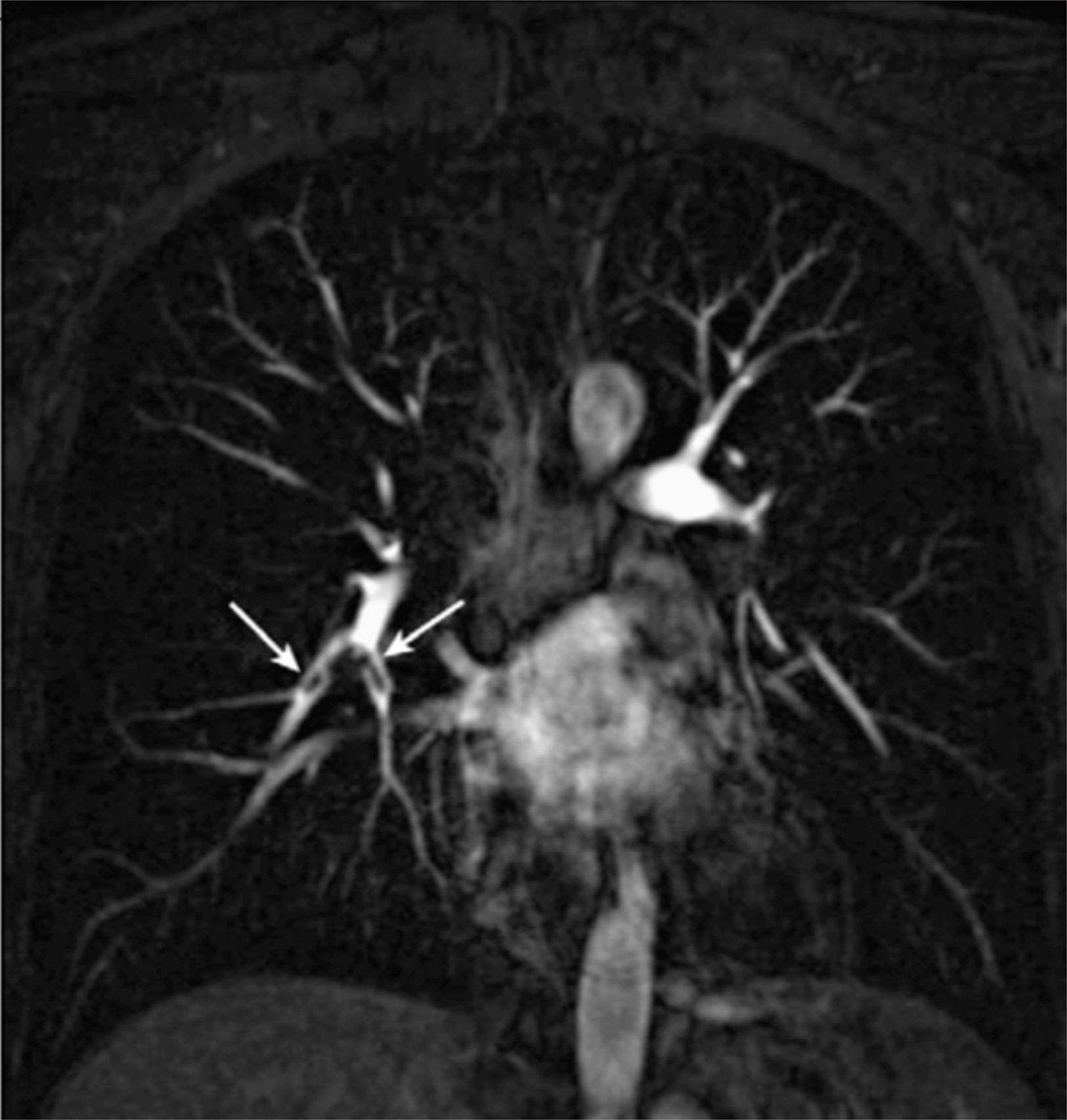
She was admitted to the Intensive Care Unit with the following test results: D-dimer positive, overloaded right ventricle on electrocardiogram and cardiac enzymes negative. Pulmonary thromboembolism was confirmed by angiotomography (Fig. 2). In two days, she presented elevation of muscle enzymes (CPK 10574 U/L and myoglobin 2563ng/ml), acute renal failure and sepsis secondary to limb ischaemia, owing to which she was subjected to supracondylar amputation due to the progressive systemic repercussion of the limb's ischaemia.
DiscussionPhlegmasia cerulea dolens is a rare form of deep vein thrombosis complicated by acute arterial ischaemia.3 It presents in 2–10% of cases of deep vein thrombosis.6 It consists of a clinical triad of limb oedema, acute ischaemic pain and cyanosis, leading to venous congestion with oedema, massive fluid sequestration causing circulatory collapse and shock as the cause of death.7
Approximately 200 publications regarding cases of the disease were found in a review of the literature of the last 30 years. In a third of these cases the condition can be attributed to malignancy. In others it was attributed to other causes, including hereditary thrombophilia (Leiden factor V, prothrombin gene mutation or protein C or S deficiency), venous stasis or the use of oral contraceptives.8
PCD is classified according to severity: non-complicated, imminent venous gangrene and venous gangrene. It progresses to venous gangrene in 40–60% of cases and has a mortality rate of 25–40%, nearly 30% of which are due to pulmonary thromboembolism. The rate is especially high when gangrene develops. The risk of serious complications such as amputation is 20–50%.3
Treatment consists of anticoagulation, thrombolysis, surgical thrombectomy and, in case of acute ischaemia with haemodynamic repercussion, amputation of the limb.8
Despite initial and opportune anticoagulation, our patient developed acute ischaemia as the result of compartmental syndrome, as well as systemic repercussion, hence she was subjected to radical life-saving treatment.
ConclusionDeep vein thrombosis is a clinical challenge for doctors of all disciplines. The greatest concern is pulmonary thromboembolism, which can be fatal. PCD is an emergency that cannot only lead to limb loss, but also to death, owing to its multiple possible systemic effects. It is therefore essential for the first doctor to come into contact with the condition to rapidly evaluate, start treatment with anticoagulation, intravenous reanimation and analgesia, rapidly determining the need to refer the patient to a specialist.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors declare that there are no conflicts of interest.