Thoracoscopy is a procedure increasingly used because it is minimally invasive and assists in the diagnosis and treatment of different types of pathologies. The anaesthetic technique has evolved over time. In the beginning it was necessarily invasive, by selective or non-selective intubation; now it is non-invasive with appropriate regional anaesthesia and intravenous analgesia/sedation in selected cases. At the Hospital General de México “Dr. Eduardo Liceaga”, in a significant proportion of cases thoracoscopy is currently done with the patient awake so we consider it necessary to report some of these cases along with the results obtained.
La toracoscopia es un procedimiento cada vez más utilizado al ser poco invasivo y coadyuvar en el diagnóstico y tratamiento de diferentes tipos de patologías. La técnica anestésica ha evolucionado con el paso de tiempo de ser necesariamente invasiva, mediante la intubación selectiva o no selectiva, a ser no invasiva con una adecuada anestesia regional y analgesia/sedación intravenosa en casos seleccionados. En el Hospital General de México “Dr. Eduardo Liceaga” actualmente se realiza la toracoscopia con el paciente despierto en una proporción importante de casos por lo que consideramos necesario reportar algunos de estos casos acompañados de los resultados obtenidos.
Less invasive surgical techniques are increasingly being used to avoid complications such as infection of the surgical wound, bleeding, dehiscence and pain. As these techniques have evolved, anaesthetic procedures have improved, providing greater comfort and intra-operative safety and the appropriate management of post-operative pain with fewer complications. The technique of thoracoscopy with sedoanalgesia and local infiltration was used almost exclusively to diagnose patients with exudative pleural effusion, but currently its use has expanded to many thoracoscopic procedures, such as bullectomy, sympathectomy, pericardial fenestration and partial pulmonary resection. Increasingly, more complex procedures are performed using this technique, such as lobectomies and thoracoscopic decortications.1
This procedure often provides diagnosis and management in various pathologies all at once, in addition to being more economical in comparison to other diagnostic and therapeutic tools.2
Although thoracoscopy has a low complication rate, the most common complications are haemorrhage, bronchopleural fistula, pneumothorax and pneumonia. Other, less frequent complications include subcutaneous emphysema, skin infection at the puncture site, hypotension during the procedure and atrial fibrillation.3
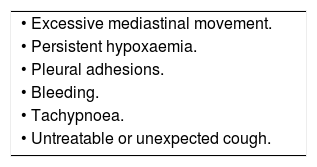
There are complications that may require changing the technique from an awake patient under sedoanalgesia plus local anaesthesia to anaesthesia in an intubated patient. These are described in Table 1.
Reasons for changing non-intubated anaesthesia to intubated anaesthesia.4
| • Excessive mediastinal movement. |
| • Persistent hypoxaemia. |
| • Pleural adhesions. |
| • Bleeding. |
| • Tachypnoea. |
| • Untreatable or unexpected cough. |
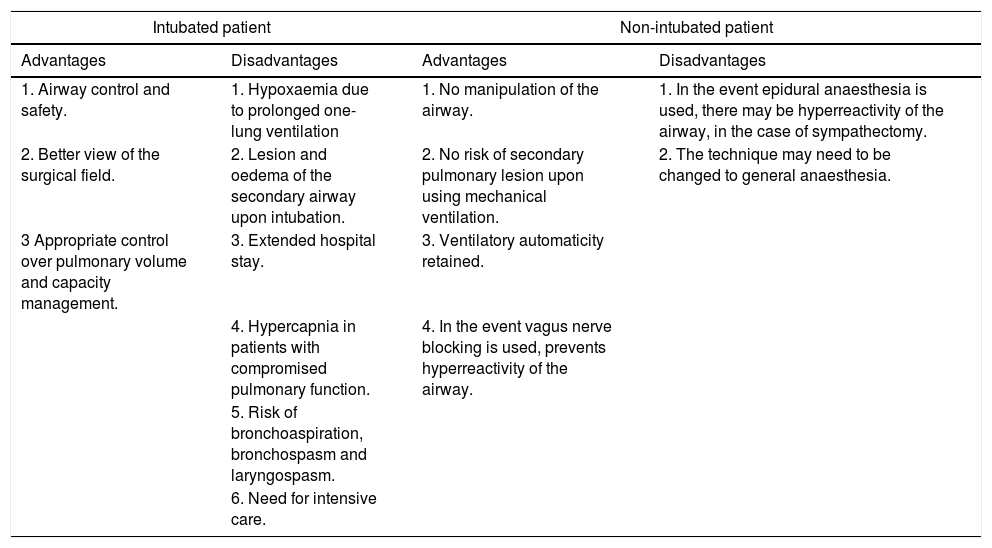
Anaesthesia management decisions in thoracoscopy depend on whether the patient will be intubated or not and based on this, certain premises are maintained, which are listed in Table 2.
Advantages and disadvantages of thoracoscopy in an intubated patient versus a non-intubated patient.
| Intubated patient | Non-intubated patient | ||
|---|---|---|---|
| Advantages | Disadvantages | Advantages | Disadvantages |
| 1. Airway control and safety. | 1. Hypoxaemia due to prolonged one-lung ventilation | 1. No manipulation of the airway. | 1. In the event epidural anaesthesia is used, there may be hyperreactivity of the airway, in the case of sympathectomy. |
| 2. Better view of the surgical field. | 2. Lesion and oedema of the secondary airway upon intubation. | 2. No risk of secondary pulmonary lesion upon using mechanical ventilation. | 2. The technique may need to be changed to general anaesthesia. |
| 3 Appropriate control over pulmonary volume and capacity management. | 3. Extended hospital stay. | 3. Ventilatory automaticity retained. | |
| 4. Hypercapnia in patients with compromised pulmonary function. | 4. In the event vagus nerve blocking is used, prevents hyperreactivity of the airway. | ||
| 5. Risk of bronchoaspiration, bronchospasm and laryngospasm. | |||
| 6. Need for intensive care. | |||
In a comparison of the advantages between management of intubated versus non-intubated patients, non-intubated patients present fewer complications, shorter postoperative thoracic drainage times and shorter hospital stays.
In 1999, eleven centres in the United Kingdom offered thoracoscopy services under local anaesthesia, increasing to 17 centres in May of 2004 and to 37 centres in 2009.1 In the Pulmonary Department of Hospital General de México “Dr. Eduardo Liceaga”, percentages have changed with regard to selective intubation, non-selective intubation and sedoanalgesia techniques. In January of 2016, 100% were performed with intubation (60% with non-selective intubation and 40% with selective intubation), a paradigm that changed in June of the same year, when 40% of thoracoscopies were performed with non-selective intubation, 30% with selective intubation and 30% with sedoanalgesia. In August 2016, 100% of thoracoscopies were performed under sedoanalgesia.
The purpose of using sedoanalgesia instead of general anaesthesia for the patient undergoing thoracoscopy was to reduce the probable effects of the anaesthetics used in general anaesthesia on blood pressure and on neuromuscular relaxation, both during administration of anaesthesia as well as post-anaesthesia. Furthermore, because patients do not need to be extubated, the duration of the anaesthesia is shorter.
Another objective is to implement a sedoanalgesia protocol that can be used in second or third-level centres where thoracic surgeries are performed.
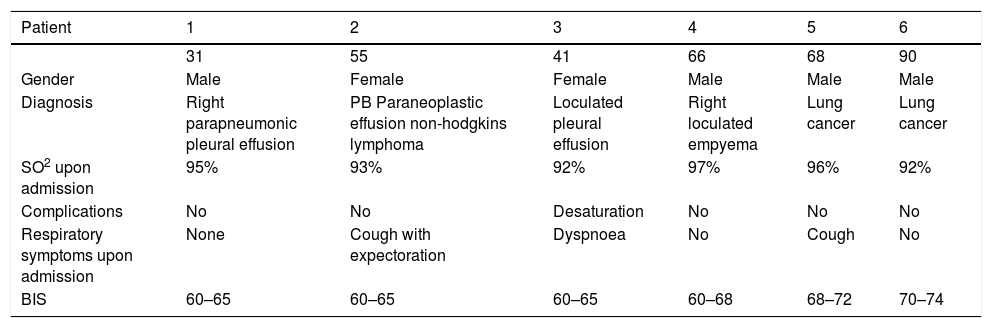
Number of cases6 cases of thoracoscopy were recorded in non-intubated patients under sedoanalgesia, performed in the pulmonary department during the months of July-August; 4 males and 2 females aged between 31 and 90 years of age. Their individual characteristics are detailed in Table 3.
Patient variables during anaesthesia in awake patients undergoing the thoracoscopic technique.
| Patient | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| 31 | 55 | 41 | 66 | 68 | 90 | |
| Gender | Male | Female | Female | Male | Male | Male |
| Diagnosis | Right parapneumonic pleural effusion | PB Paraneoplastic effusion non-hodgkins lymphoma | Loculated pleural effusion | Right loculated empyema | Lung cancer | Lung cancer |
| SO2 upon admission | 95% | 93% | 92% | 97% | 96% | 92% |
| Complications | No | No | Desaturation | No | No | No |
| Respiratory symptoms upon admission | None | Cough with expectoration | Dyspnoea | No | Cough | No |
| BIS | 60–65 | 60–65 | 60–65 | 60–68 | 68–72 | 70–74 |
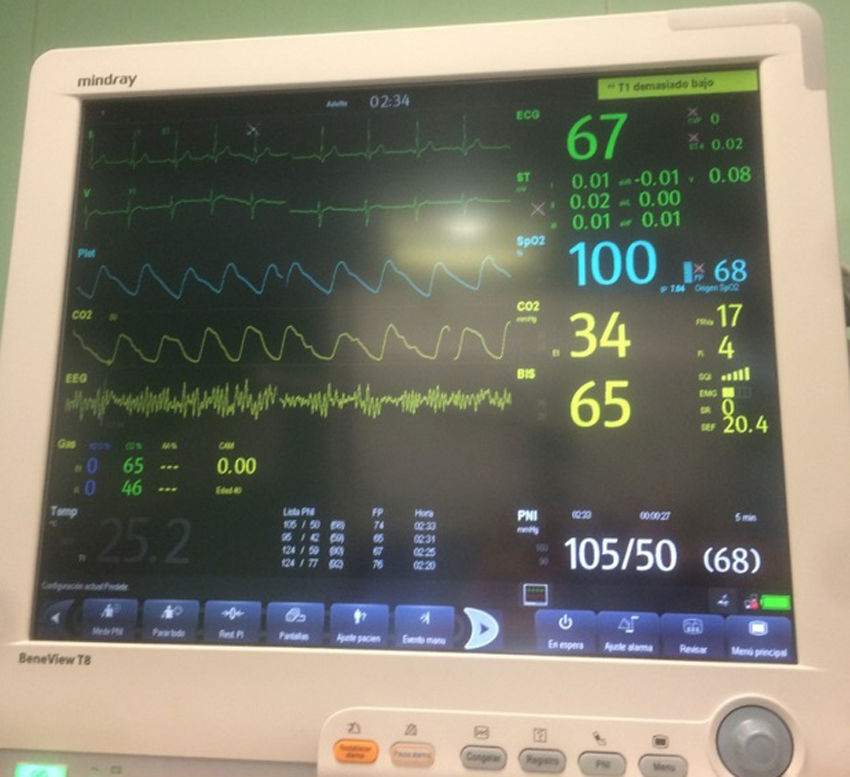
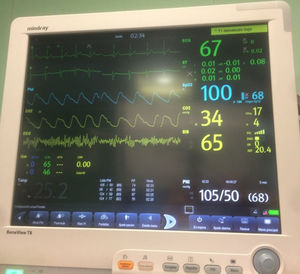
Upon arriving in the operating room, they were subjected to continuous electrocardiographic monitoring, pulse oximetry, respiratory rate, blood pressure and body temperature. Continuous end-tidal carbon dioxide monitoring (ETCO2) was performed by inserting a detector in the nasal cavity (Fig. 1). All patients admitted had a saturation of over 90%. Sedation monitoring was performed by bispectral index (BIS), maintaining a range of between 60 and 75 (deep sedation); with this degree of sedation the patients retained ventilatory automaticity, except for one case of desaturation (SaO2<90), in which 2min of manual ventilation was required. Upon achieving bispectral index values of around 60, the surgical team performed an intercostal nerve block with 0.375% ropivacaine, allowing a 5-min latency prior to starting the incision.
The patient was in the lateral decubitus position on the unaffected side for the procedure. Three minutes after being placed in position, the local anaesthetic is injected into the corresponding intercostal space at the site of the thoracoscopic port using 10ml of ropivacaine, (7.5mg/ml), divided into four steps (for each one, local anaesthetic was applied): The first step is in the epidermis, and to this end the skin is cut, above and parallel to the rib, dissecting through the subcutaneous tissue; the second step begins prior to dissection towards the aponeurosis of the thoracic muscles. The third step is performed in the muscle wall to make the incision through the thickness of the muscle wall to the rib. The fourth step consists of anaesthetising the pleura. Local anaesthetic duration ranged from 30 to 150min (70min average). Just before pleural opening, administration of a propofol IV bolus (0.5–1mg/kg IV in 10–15s) is recommended to achieve mild to moderate sedation, especially in obese patients or patients with hypertrophic muscles, since it is difficult to achieve effective pleural anaesthesia and could lead to loss of control over pain and/or vagal reflexes.
Piston-type perfusion pumps were used for the perfusion of intravenous anaesthetics. As an anxiolytic, midazolam 30μg/kg, lidocaine bolus 1.5mg/kg were administered followed by a perfusion of 15–25μg/kg/min; analgesia with sufentanil 0.3μg/kg bolus, continuing perfusion of 0.002–0.005μg/kg/min response dose; Propofol 1mg/kg bolus for 3–5min and then perfusion of 60–120μg/kg/min to keep the BIS in the range of 60–75% (Fig. 2).
To avoid periods of reduced oxygen saturation, a facial mask was used for control, with flow between 10 and 15l of oxygen per minute. The patient was kept sedated, (the goal was 3 on the Ramsay scale) with oxygen saturation always above 90% although 2 patients presented with hypercapnia due to decreased ventilatory frequency. The exhaled CO2 remained between 40 and 50mmHg. Although respiratory rate sometimes decreased when sedation with permissive hypercapnia was increased, the surgeon and assistants adjusted the instruments and range according to the respiratory rhythm in order to perform a precise dissection. Although the pulmonary collapse was not complete, it was generally satisfactory, with pulmonary movement that did not hinder the surgical manoeuvres (Fig. 3).
The coanalgesics used were tramadol 1mg/kg and paracetamol1g IV, adjuvants ondansetron 4–6mg IV and omeprazole 40mg IV.
At the end of the surgery, the propofol perfusion was stopped and since the patient was fully awake; the patient was asked to breathe deeply and cough, achieving re-expansion of the collapsed lung.
One patient presented with desaturation during delivery of the anaesthetic but the patient recovered after 5min with no gasometric alteration. All patients left the post-anaesthesia unit with Ramsay 2, saturation greater than 90% with facial mask at 3l/min. There were no post-anaesthesia complications nor any need for rescue analgesia. They were assessed after 24h showing mild to zero pain, no patient presented with signs of delirium, anxiety or residual anaesthesia.
DiscussionThe group of anaesthetists of the Hospital General de México is in favour of non-invasive monitoring by pulse oximetry, electrocardiogram and non-invasive blood pressure monitoring since, even though entry to the thoracic cavity is performed, there are few haemodynamic complications arising from the procedure. Although some articles mention that using a thoracic epidural block provides sufficient analgesia during and after the operation, we feel that the intercostal block with an appropriate sedoanalgesic is sufficient to obtain similar analgesic results without the potential complications of an invasive technique like the thoracic epidural, the cornerstone of this technique being the administration of sufentanil at sufficient plasma concentrations.
As a basis for sedation, propofol was used for its pharmacokinetic characteristics and short half-life, providing quick recovery when perfusion is stopped; Grendelmeier et al. found greater risk using propofol vs midazolam for conscious sedation, due to a greater incidence of hypoxaemia (arterial pulse oxygen saturation <90%) and episodes of hypotension (systolic blood pressure <90mm Hg).5
Although several authors recommend the vagus nerve block to prevent the cough reflex upon pulmonary manipulation, especially in the hilar region,6 at our centre, as a result of the anatomical distortion presented by most of the patients admitted for thoracoscopic surgery which makes the use of this technique difficult, it was decided to implement intravenous lidocaine perfusion as an alternative. This is a suitable option since, as described by Gonzalez et al.,5 it has been shown to reduce cough post-intubation and during the procedure in addition to being an adjuvant to improve intra- and post-operative sedation and analgesia.
Although we know that one of the tests for determining the integrity of the pulmonary interstitium is the diffusion of carbon monoxide, and that it would provide safety to the patient under thoracoscopic vision, because we do not have this procedure in the hospital, the only inclusion criteria we use are the patient's basal saturation of over 90% as well as an appropriate response to the administration of supplemental oxygen (values between 98 and 100%).
ConclusionsProviding the patient with appropriate analgesia without intubation in thoracoscopy is possible thanks to appropriate sedation and intercostal anaesthesia since lung parenchyma does not cause pain. Cough, caused by stimulation of the diaphragm and/or manipulation of the pulmonary hilum during thoracoscopy, can be stopped by blocking the vagus nerve under thoracoscopic view or with the intravenous perfusion of lidocaine, although clinical trials still need to be done to show the advantage of one technique over the other.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors declare that they have no conflict of interests.